Even the most brief distractions can lead to an accidental injury. When sharps are involved, it`s no time to hurry.
Cathleen Terhune Alty, RDH
Lisa, Dr. Smith`s dental assistant, was stuck yesterday. She wasn`t stuck with a dead car battery or cleaning out the suction traps. She was stuck by a contaminated needle.
It`s a familiar story. She was in a hurry and really meant to use the one-handed scoop to recap it. In her haste, though, she used her left hand to steady the needle cap, preventing the cap from sliding. When the receptionist returned to ask a question, Lisa looked up at exactly the wrong time. The contaminated needle poked through her latex glove and into her finger. Ouch!
Along with the immediate pain, she was also immediately worried. "Will I get a disease, like HIV, from this needle stick? Should I check the patient`s health history? What do I do now?"
Lisa is a fictitious person with a very real and, unfortunately, common problem. Her biggest concern may be the threat of catching a disease. But she should also focus on preventing something like this from happening again.
Is infection likely?
Lisa may find some comfort when she discovers the latest research about percutaneous exposure in the dental office. For example, an incident such as above does not necessarily mean the worker will be infected, particularly with HIV. A recently published study indicates the amount of blood on the item and the type of injuries sustained with contaminated sharps may not be in themselves a high risk for HIV, even when the source patient is HIV positive.
In September 1995, the CDC Cooperative Needlestick Surveillance Group released data from a national project whose subjects are health care workers (HCWs) exposed to blood which was known to be infected with HIV. Of the 2,860 HCWs, 19 are dental care workers. Three of the 19 are dental hygienists. All of the enrolled dental workers had a percutaneous exposure to HIV-infected blood.
Of the 19 injuries, eight occurred during use of the instrument or device, and 11 occurred afterward. According to the data published in the Journal of the American Dental Association, the researchers estimated "the risk of HIV infection after percutaneous exposure to HIV-infected blood to be approximately 0.3 percent." The amount of blood from the source patient and the amount of infectious agent in the source blood are two factors which may influence this percentage. Although this study has few exposed dental care workers participating, other studies have shown similar results.
The researchers concluded, "Available information indicates that the overall risk of transmitting HIV to workers in a dental setting is very small."
If there`s a small risk, why worry?
If the chances of catching HIV from a needle stick or other percutaneous injury in the dental office is so small, why is everyone so concerned when it happens? There are several reasons.
"It`s more than just HIV," said Kathy Eklund, RDH, MHP, associate professor at Forsythe School for Dental Hygiene. "There`s hepatitis B, C, D, and many other diseases. You`re still at risk. There is still that 0.3 percent chance of HIV.
"That`s why it is important to go through post-exposure management procedures, although it can be psychologically and emotionally difficult."
Eklund said that, after enduring the medical evaluation and counseling procedures, the employee will probably be very motivated to prevent future injuries in the office.
"It`s so important to think preventively - to prevent any kind of injury, not just needle sticks. And if an injury occurs, it`s important to remember basic first aid procedures following an injury. Potentially more damage can be done if first aid procedures are not done correctly," Eklund added.
Dr. Chris Miller, director of Infection Control Research and Services at Indiana University, points out, "You never know when an exposure will lead to disease."
Dr. Miller, who is also a professor of oral biology, explains that relying solely on the body`s defense system to fight off invading microbes is not a good idea - no matter how remote the chances of acquiring a disease.
He reminds us that we are ultimately responsible for our own protection. "Only the individual can prevent their injuries," he said. "Someone else can`t do it for them. We can give them all the tools, tips, and techniques. But the bottom line is they have to protect themselves."
Injury reports from the chairside
The frequency of percutaneous injuries in an average dental practice was recently researched. An ADA study published in September 1995 examined a 20-day percutaneous injury diary of 2,304 dentists, and a total of 647 injuries were reported by the respondents. Of the 549 injuries that could be characterized, 82 percent occurred extraorally during chairside procedures, cleanup or lab work, and 33 percent occurred during restorative procedures.
The majority of these injuries were caused by burs (37 percent), sharp instruments (32 percent), and syringe needles (17 percent) on the fingers or hands (87 percent) instead of arm and face (13 percent). Seventy-three percent of the injuries occurred to the non-dominant hand.
These figures were extrapolated to project that an average dentist, working 48 weeks per year and five days a week, would experience 3.35 injuries annually.
"We see this data as a baseline, although we`d ideally like to see it at zero," said Dr. John Molinari, professor and chairman at the department of biomedical Sciences at University of Detroit Mercy School of Dentistry. "If you think before you act and just use common sense, most injuries could be avoided."
He said, for example, burs cause about one-third of the injuries. He advocated making sure burs are positioned away from you. "Hang them upside down if necessary or turn them toward the bracket tray. The new dental equipment is designed to keep burs out of the way."
Dr. Molinari said hollow-bore needles cause another one-third of the injuries, and sharp instruments, such as scalpels and curettes, cause a third of injuries. "If we eliminate hand scrubbing and insist on heavy duty utility gloves this will reduce injuries," he said.
Dr. Miller emphatically goes a step further. "Handscrubbing instruments should be outlawed," he said. "Use the ultrasonic cleaner with its basket and don`t stick your hands down into it. And don`t get too confident with the heavy utility gloves because a sharp instrument can still stick through it. The less you handle instruments, the less chance of injury."
He recommended putting sharps where they belong and disposing of scalpel blades, used needles, and broken instruments at chairside.
"You need to slow down and watch what you`re doing. Never take your eyes off a sharp. Everyone knows this; it`s common sense. But we need to be reminded," Dr. Miller said.
The entire office, Dr. Miller said, needs to work together to prevent sharps injuries. Injury prevention should be discussed at staff meetings and signs posted. He said, "No matter how silly it sounds, it can`t be emphasized enough."
An infection control expert at the ADA pointed out that engineering controls prevent percutaneous injuries from happening in the dental office. "It is more important to follow the correct procedures than to cut corners and hurry through it," he said. "Staff members seem to be ignoring prevention, and it is very important. OSHA is seen as an avenging god who is out for punishment, when in reality OSHA is there to protect workers."
Eklund added, "Accidents happen. People do make errors. We should not focus on blaming. Instead, we should look at what, why, and how the injury happened, what are the behaviors, and how can we change it so it doesn`t happen again." She stressed that staffs need to learn from mistakes, and evaulations should include the near-misses, the "times when we were almost exposed."
She said dental offices often try to conform safety to the environment instead of conforming the environment to safety. "We need to look at our behaviors. It`s very easy to get into habits that aren`t safe." For staff members who have been exposed via a percutaneous injury, fear seems to be the dominant emotion. Dr. Molinari said, "In seminars people who have been exposed say they were very concerned for awhile. Most characterized the incident by blaming their own stupidity. We need to use some of that fear energy to correct the situation."
An expensive mistake
It can also be costly to be injured. There are medical costs, administrative costs, and potential OSHA fines. For example, once an employee reports an exposure incident, OSHA requires a confidential medical evaluation and follow-up, including counseling. The source individual`s blood also needs to be tested if their serostatus is unknown.
OSHA also has very specific regulations regarding the filing and storage of this information. If the required OSHA injury log in the office documents exposure incidents without indications of training to prevent these injuries from reoccurring, fines can be levied for insufficient training or "willful noncompliance."
Last, but not least, office personnel need to be prepared. "This has gone beyond infection control. It`s now a health and safety issue," says Eklund. "Who wants to be in the 0.3 percent? We need to talk about exposure incidents before they happen. We need to prepare ahead - why, when, what it means. We need more education and training to heighten their awareness as well as more research to examine these injuries."
Office personnel need to be aware of local and regional resources for help. The psychological impact of being exposed can be great. Eklund says counseling is a very important part of the evaluation and follow-up after an injury. "Counseling can put the injury in perspective," she said.
Many questions surrounding percutaneous injuries still need consideration. What about the source patient? The patient is not under obligation to be tested or share any test results. How will the exposed employee`s personal life be affected?
The exposed individual is often encouraged to practice safe sex practices, possibly up to a year after exposure. Is the exposure incident established as an occupational injury, subject to worker`s compensation? Postponing serostatus testing can be a problem if tests are positive for HIV.
Obviously prevention is the key.
Cathleen Terhune Alty, RDH, is a contributing editor for RDH and is a member of the Office of Sterilization and Asepsis Procedures Research Foundation.
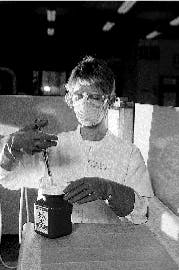
Kathy Eklund of Forsythe demonstrates proper protocol to prevent injuries.
Six wise steps to remembering safe behavior all day long
Obviously, the experts agree that prevention of percutaneous injuries is critical and not to be taken lightly. Some things to keep in mind:
- Use common sense.
- Adherence to OSHA and CDC requirements and recommendations regarding safe work practices, particularly with sharps.
- More education and training on avoiding sharps injuries: staff meetings, component dental society meetings, and continuing education courses.
- Greater awareness of the circumstances surrounding possible percutaneous injuries and how to avoid them.
- Think first, act second, when holding sharps.
- Remember what happens when exposure occurs: worry from being exposed, time off work for medical evaluations and follow-ups, counseling, mental anguish waiting for test results, paperwork and record keeping, concern for spouse and loved ones, etc.
OSHA`s view of percutaneous injuries
If you are injured by a sharp, OSHA requires that the employer make immediately available to the exposed employee a confidential medical evaluation and follow-up. Related documentation must note the route of exposure, the circumstances under which the exposure incident occurred, and identification and documentation of the source individual.
The employer must provide the health care professional evaluating the employee following an exposure incident:
- A copy of the bloodborne pathogen standard.
- A description of the exposed employee`s duties as they relate to the incident.
- Documentation of the route and circumstances of exposure.
- Results of the source individual`s blood testing (if available).
- All medical records relevant to the appropriate treatment of the employee, including vaccination status.
The employer must also obtain and provide the employee with a copy of the evaluating health care professional`s written opinion within 15 days of the completion of the event. Medical records must be kept confidential and maintained for the duration of employment plus 30 years.
For further information and details regarding percutaneous injury follow-up, consult the OSHA Bloodborne Pathogen Standard.