Adverse reactions to local anesthetics
By Cynthia R. Biron, RDH, MA
Many medical emergencies that occur in dental offices are brought on by apprehension to, or reaction from, the administration of local anesthesia. Most emergencies are not due to reactions to the local anesthetic itself, but to the anxiety associated with the injection.
The most common reaction is the psychogenic response commonly known as syncope, or fainting. The second most common reaction is hyperventilation or anxiety attack. Anyone who is apprehensive enough can present with either of these manifestations.
But those with other health problems - such as epilepsy, asthma, coronary artery disease (CAD), thyroid dysfunction, diabetes, and other diseases - may have reactions that are associated with their respective health problems. For example, the epileptic patient who is apprehensive has a decrease in seizure threshold and then a seizure. The asthmatic patient has an asthma attack; the CAD patient has chest pain; and the diabetic patient has an insulin reaction. Other conditions patients have might predispose them to a medical emergency.
The majority of adverse reactions to the drug itself are toxic overdose reactions. The overdose may be relative - that is to say, the normal dosage may be an overdose for a particular individual - or absolute - which means it is an overdose for any individual, more than the recommended dose for efficacy.
Many patients who experience such a reaction think they are allergic to the local anesthetic. This certainly is not the case. Allergic reactions rarely occur with the amide-type local anesthetics used today. If they did, the manifestations most likely would be characteristic of allergy symptoms, with skin reactions such as hives, rash, and itching, followed by breathing difficulty.
Predisposing factors
Predisposing factors to toxic reactions to the local anesthetic itself include:
a Patients under 6 years and over 65 years of age - Absorption, metabolism, and excretion are not fully developed before age 6, and these functions diminish after age 65.
a Underweight patients, especially those with little muscle mass - Drugs are calculated on mg of drug/per kg, or pound of weight. The less an individual weighs and the less muscle mass he has, the lower the tolerance to the drug.
a Liver disorders - Liver damage causes local anesthetic to build up in the blood. Most local anesthetics are biotransformed in the liver and broken down to products that can be eliminated from the body by the kidneys. A history of liver disease may indicate that the liver`s ability to degrade the drug is reduced. If the liver doesn`t do its part, then the local anesthetic accumulates in the blood. In such cases, local anesthesia should be used judiciously and in consultation with the patient`s physician.
* Genetic factor in patient ("serum cholinesterase") - Serum cholinesterase is an enzyme produced in the liver needed in the biotransformation of ester local anesthetics. If it is genetically missing, an overdose can result from increased blood levels.
* Kidney disorders - If the kidneys cannot eliminate the byproducts of local anesthetics, there can be toxic accumulations in the blood.
* Pregnancy - During pregnancy, kidney renal function can be disturbed. This can impair excretion and result in an increased blood level of the local anesthetic.
Drug factors
Various factors lead to toxic reactions to local anesthetics. Local anesthetics have vasodilating properties, which increase the possibility of overdose.
The amount of drug given should not be more than 1.1 dental cartridges of 2 percent lidocaine per 20 pounds of body weight. More than that amount increases the chances of toxic overdose. The rate of injection is the most important factor in preventing overdose. A rapid injection (30 seconds or less) causes rapid blood levels, which increases the chance of overdose. Injections should be administered slowly (60 seconds or more for administration of a 1.8 mL cartridge). This produces a low blood level, which decreases the chance of overdose.
Another cause of toxic overdose is intravascular injection, which occurs when the anesthetic is unintentionally injected directly into a blood vessel. Both interarterial and intravenous injections may produce overdose reactions. Intravascular injection is usually prevented by using an aspirating syringe. A return of blood into the dental cartridge is considered a positive aspiration. Even if there is no return of blood into the dental cartridge, there is still a risk of intravascular injection if the injection is administered rapidly and in close proximity to a capillary bed.
Vasoconstrictors are important
The mouth is highly vascular, making absorption of local anesthetic into the blood more rapid than at other sites. This is why the presence of a vasoconstrictor in local anesthetics is so important. The vasoconstrictor counteracts the vasodilating properties of blood vessels and decreases the rate of systemic absorption. The most common vasoconstrictor is epinephrine. Epinephrine should not be used on patients who take a variety of medications; however, there is a greater risk of medical emergency if local anesthesia is administered without it. The most common adverse drug reaction with local anesthesia is not a reaction or drug interaction with epinephrine - it is local anesthesia toxicity.
Avoiding local anesthesia overdose requires accurate patient evaluation. We must also consider the aforementioned factors of age, weight, health history and status, and select the proper local anesthetic and administer it with the correct technique.
Clinical manifestations of local anesthesia overdose
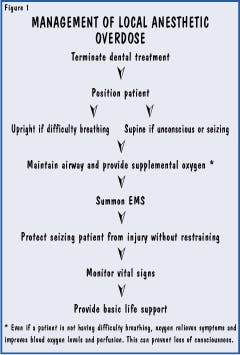
The clinical manifestations of local anesthesia overdose differ according to cause. If the cause is rapid injection, the manifestations are of rapid onset, very intense, and of short duration, with unconsciousness and seizures appearing within seconds.
If the cause is from a too-large dose of anesthetic or unusually rapid absorption, symptoms will manifest within three to five minutes, will be of mild intensity, and will last longer than five minutes.
Unusually slow biotransformation of the drug in the liver, or poor elimination of the drug from the kidneys, results in slower onset of symptoms that persist over a longer period of time. As much as 25 minutes could go by before symptoms manifest. The initial sign is tremors, followed by convulsions. When the patient is unable to rid the body of the local anesthetic, the symptoms may persist for long periods of time.
Management of local anesthetic overdose
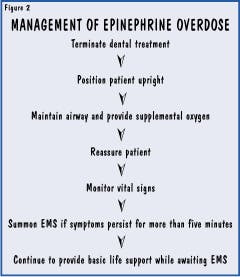
Epinephrine is the most widely used vasoconstrictor in local anesthetic. Use of anesthetic with epinephrine vasoconstrictor is contraindicated in patients with cardiovascular disease, because epinephrine increases blood pressure, heart rate, and may alter the heart rhythm. The clinical manifestations of epinephrine overdose are similar to an acute anxiety response. There is a rapid rise in blood pressure and heart rate with extreme nervousness, tremors, and restlessness. Most epinephrine overdose reactions rarely last for more than a few minutes.
Always stay with a patient who is receiving local anesthesia. Remain with the patient after the injection and observe signs and symptoms so that you may readily respond to the need for emergency management of an adverse reaction.
References
Malamed SF: Medical Emergencies in the Dental Office ed 5, St. Louis, 2000, Mosby.
Meiller T, et al: Dental Office Medical Emergencies, Hudson, Ohio, 2000, Lexi-Comp.
Little JW: Dental Management of the Medically Compromised Patient ed 4, St. Louis, 1993, Mosby.
Cynthia R. Biron, RDH, MA, is chair of the dental hygiene program at Tallahassee Community College. She is also a certified emergency medical technician.