It's dirty water, but how bad is it? Is it really a low-risk gamble?
by Nancy Andrews, RDH, BS
What do you know about the hidden maze of tubing inside your dental unit? That used to be a question reserved for equipment technicians, not dental professionals. Now, the potentially dangerous problem of dental water contamination is clearly in the hands of dental clinicians, and in the mouths of their patients. We have made remarkable improvements in dental asepsis, but many of us still haven't gone far enough ... inside the equipment.
Biofilm incubators
The slime lining virtually all dental equipment harbors huge concentrations of organisms, which, in turn, contaminate the water spraying from your handpiece, air/water syringe, or scaler.
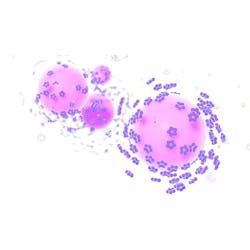
Biofilms may include many types of bacteria, fungi, algae, protozoa, and nematodes. Free-floating (planktonic) cells are vulnerable, but the slime protects the organisms from chemicals, temperatures, dehydration, and attack by immune factors when the biofilm is in living tissue.
The first bacteria attaching to a surface form a colony, and build mushroom-shaped pillars. If part of this matrix remains, active biofilm returns rapidly, even when the organisms are killed. As water flows through and by the biofilm, microorganisms and their waste products contaminate the dental water — and spread.
Drinking water is delivered to us with acceptable levels of contaminants. The pipelines build up some biofilm, but the physics of large volumes of chemically treated water moving through large pipes at fairly rapid rates keeps the microbial contamination within healthy limits.
When people drink water with more bacteria than that, they are likely to become ill. The trouble is that, in dental units, virtually all of the water sits or moves incrementally through the narrow tubing and is in constant contact with the biofilm lining the waterlines. Safe water enters our dental unit, but leaves grossly contaminated.
If biofilm is naturally found everywhere, what's wrong with the biofilm in dental lines? The answer is concentrations of organisms, and, of course, which organisms. To give you a perspective: If you measure environmental bacteria, research shows you can expect to find:
- 0 CFU/ml in freshly fallen snow,
- 3 CFU/ml in unpolluted drinking wells,
- 19 CFU/ml in city rainwater,
- 64 CFU/ml in clean river water,
- 372 CFU/ml in shallow wells,
- 2,166 CFU/ml in polluted river water,
- Anywhere from 1 to over 10 million CFU/ml in raw sewage.
Researchers have shown that dental units consistently deliver water with thousands to millions of bacteria/ml — somewhere between the levels of polluted river water and raw sewage on this chart.
Inside the tubing, biofilm bubbles out, breaking off naturally. It sloughs even more when the tubing is manipulated.
Sometimes, the pieces of biofilm can be seen by the naked eye. But very small pieces of biofilm, or individual organisms that are carried downstream, are not visible, even in grossly high concentrations.
What about just flushing water through the lines? This idea still makes sense as a precaution, but does not have a lasting effect on water contamination because the biofilm remains. In fact, flushing can dislodge very large numbers of organisms.
The link between disease and biofilm
One frequent question is, "What, exactly is our risk?" Potentially pathogenic biofilm species identified in DUWL's include Legionella, Streptococcus, Staphylococcus, Pseudomonas, Mycobacterium, Enterococcus, Salmonella, E. coli, Bacterioides, Cryptosporidium, Acanthamoeba, Candida, and even nematode worms.
These organisms are associated with pneumonia, septicemia, abscesses, appendicitis, bronchitis, and allergies. In addition, the organisms can be associated with infections such as nosocomial surgical infections, contact lens, gastrointestinal infections, and skin, head, neck, and dental infections.
These illnesses are contracted through mucosal tissue, eye, and open tissue exposure as well as breathing and swallowing organisms. People with compromised immune systems are the most susceptible to biofilm pathogens. As we get older, even if we are vital and active, we all become more immunocompromised. Lack of sleep, short-term stress, or illnesses can render us susceptible.
Dental practitioners exposed to waterline aerosols should be knowledgeable about their exposure, and consider reasonable protection. If a slime-encased bacterial biofilm becomes established inside our bodies, it is very difficult, if not impossible, to defeat the infection. Even those of us with healthy immune systems can be infected by the large numbers of organisms we're talking about.
Unless we prevent it, sloughed biofilm will enter the mouths, lungs, and bloodstream of patients, and will also be breathed in by dental workers.
Cryptosporidium and other spores can survive corrosive chemicals. This is vital information for immunocompromised people, such as AIDS victims, who may not survive an infection. These people may be boiling their drinking water at home to avoid infection, and surely would never think their dentistry is done with water that is much more contaminated than drinking water. Using water that exceeds the safety standards of regular drinking water should protect susceptible individuals. For example, point-of-use filtration simply removes spores that survive chemicals and pathogens that build up between chemical waterline treatments.
Retraction of disease factors is a known problem with dental equipment. Some units retract water into the tubing every time the water is stopped, pulling contaminants from the patient into the waterlines and releasing them later to other patients. There are many common infectious microbes, such as dental and periodontal pathogens, herpes, condyloma virus, chlamidia, and bloodborne pathogens (hepatitis and HIV) that no one wants to think could be passed from patient to patient by the water system.
Solutions to the problem
Engineering controls to defeat biofilm fall in two main categories:
- Physical prevention and/or removal of biofilm and related contaminants.
- Chemical cleaners and disinfectants.
Physical devices and methods include:
- Filtration
- Anti-retraction designs and devices
- Heat sterilization/disinfection
- Ultraviolet light
- Physical removal (friction, pressure)
Chemical cleaners and disinfectants include:
- Chemicals used historically for water sanitation, such as iodine, chlorine, and ozone.
- Chemicals used for topical infection control, such as chlorhexidine, peroxides, organic acids, and silver.
- Chemicals deployed to fight biofilms in industrial settings, such as slime dispersants and detachment agents.
In the next issue, we will compare and combine waterline management solutions.
Nancy Andrews, RDH, BS, is currently a product manager for new product development at Kerr/Metrex. She has had numerous articles published on infection prevention in peer reviewed professional journals. She also is a member of OSAP, an infection prevention association. A graduate from the University of Southern California, Andrews practiced clinical dental hygiene for 20 years and was a clinical instructor at USC.
Biofilom diseases
Bacteria that form biofilms outside human bodies can form biofilms when they infect people. The biofilm protects the organisms from immune system and antibiotics, resulting in infections that are difficult to treat, may become chronic, and may result in the need for surgical removal of the biofilm-infected tissue.
An example of a biofilm disease is Legionellosis, or Legionaires Disease.
When dentists were blood-tested, nearly half had positive antibodies to Legionella, compared to about 5 percent of the general population. According to OSHA and the U.S. Health Department, that amounts to occupational exposure.
Some of the Legionella species cause a flu-like condition called "Pontiac Fever," while a few species can cause a fatal pneumonia.
Those with lower immune defenses, and those with respiratory weakness are most susceptible. Males, those over 60 years old, alcoholics, smokers, and the chronically ill typify the high-risk person.
Legionella can live and reproduce inside amoebas found in waterlines. These amoebae are mobile, and may travel out of their protective slime. But when the protozoa are in their encysted form, encased in a slimy biofilm, they resist even the strongest chemicals.
When the amoeba travels downstream, hits the bur or ultrasonic tip, and bursts open, the Legionella and allergenic amoebae cell parts are dispersed.
This may result in runny noses, watery eyes, and sinus irritation and infections at the very least — or a flu-like episode, perhaps, and, in the worst case, death.
In at least two cases of serious and fatal legionellosis in dentists, it is thought that waterlines were the cause. Knowing this makes us view the everyday experience of dental spray quite a bit differently. You have to ask, "How many of these organisms are in that spray?" Unless, of course, you are carefully managing your waterlines.