High blood pressure blues
By Dianne D. Glasscoe
Dear Dianne,
One of the hygienists I work with advises that a patient with a blood pressure of 180/110 or higher is contraindicated for dental treatment. I thought the safe range was lower, but I really am not sure. Can you clear this up for us?
Confused Hygienist
Dear Confused,
I'm glad you brought up the issue of blood pressure and dental treatment. This gives me an opportunity to answer your questions and open some dialog about the importance of blood pressure screening at hygiene visits.
For review, blood pressure is the pressure that blood exerts against the walls of the arteries. The amount of pressure depends upon the strength and rate of the heart's contraction, the volume of blood in the circulatory system, and the elasticity of the arteries.
When air is pumped into the blood pressure cuff, the inflated cuff presses down on the arteries. This stops the flow of blood, and no sound can be heard through the stethoscope. As the air is slowly released from the cuff, the pressure of the cuff becomes less than the blood pressure and the blood flow returns. The pressure at which the flow resumes is called the systolic pressure. It represents the blood pressure when the heart is contracting. As more air is let out of the cuff, the sounds become muffled. The pressure at this point is called the diastolic pressure. It represents the blood pressure while the heart is relaxing. Therefore, the first number is the systolic pressure and is normally around 120 millimeters. The second number, the diastolic pressure, is normally around 80.
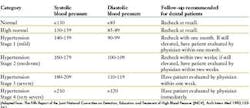
Hypertension is defined as a persistent elevation in blood pressure that is considered to be higher than normal. More specifically, the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure defines hypertension as a systolic blood pressure greater than or equal to 140 mm Hg or a diastolic blood pressure greater than or equal to 90 mm Hg as recorded during two or more readings on two or more occasions (office visits).
It is estimated that at least 58 million Americans have, or are receiving treatment for, systemic hypertension. Primary (or essential) hypertension has no clearly identifiable etiology, and accounts for 90 to 95 percent of cases. An estimated 10 to 15 percent of white adults and 20 to 30 percent of black adults in the United States currently have primary hypertension. Between 70 and 90 percent of affected individuals have mild (stage 1 or early stage 2) primary hypertension. The age of onset of primary hypertension usually ranges between ages 25 and 55. There is no clearly defined sex predominance for the disease.
Hypertension is classified by etiology as being either primary (essential, idiopathic) or secondary. Current evidence suggests the disease is caused by varying combinations of many potential interacting factors. Patients with primary hypertension do not appear to share any one, or a specific combination of, suspected etiologic factors.
No clearly established genetic pattern has been established for primary hypertension. However, blood pressure levels appear to have strong familial tendencies. Children with one (and to a greater degree two) hypertensive parent(s) tend to have higher blood pressures and are perceived to be at an increased risk to develop hypertension.
Complications of untreated hypertension are numerous. The degree of damage to susceptible "target" organs is closely related to both the duration and severity of the hypertension. These complications include:
• Cardiovascular disease — Hypertension is the most important etiologic factor for cardiovascular disease in the United States. Cardiovascular and atherosclerotic complications are the major causes of morbidity and mortality in patients with primary hypertension. In adults, systolic blood pressure elevations usually are considered to be more a determinant of cardiovascular risk than are diastolic blood pressure elevations. Hypertension accelerates the development and progression of atherosclerosis (leading to peripheral and coronary vascular insufficiency), and subsequently increases the patient's risk for myocardial infarction. Hypertension also causes left ventricular hypertrophy, which may result in congestive heart failure, ventricular arrhythmias, myocardial ischemia and sudden death. Hypertension is a major etiology for both dissecting and atherosclerotic aortic aneurysms, and also acts as an exacerbating factor in the progression of these conditions. Retinal vascular narrowing, hemorrhages, exudates and papilledema are also consequences of hypertension.
• Cerebrovascular disease — Hypertension increases the risk of cerebral vascular insufficiency, and is a major cause of stroke (cerebrovascular accident), especially those resulting from intercerebral hemorrhage, cerebral infarction or subarachnoid hemorrhage.
• Renal disease — Untreated hypertension may lead to nephrosclerosis and accounts for 40 percent of cases of chronic renal failure (end-stage renal disease). Hypertension also may accelerate the progression of other forms of renal disease such as diabetic nephropathy.
Physical and dental exam
Establish the patient's baseline blood pressure at the first dental appointment. Two to three blood pressure measurements separated by at least five minutes should be taken, and the results averaged to determine the patient's baseline blood pressure. The patient's baseline blood pressure will serve as a point of reference from which to make decisions for the emergency management of the patient should a cardiovascular or adverse reaction develop during dental treatment. The patient's blood pressure should be checked at all subsequent appointments prior to the use of a local anesthesia.
There are no specific treatment-planning modifications or considerations for patients with controlled hypertension. However, no elective dental procedures should be performed on a patient with severe or uncontrolled hypertension. Additionally, the clinician should avoid stimulating the gag reflex in patients with a history of hypertension. Uncontrolled hypertension also can cause excessive bleeding during procedures. The clinician should consider that some patients may be unable to lay back comfortably due to pulmonary congestion.
Much of the information above was adapted from an excellent article by F. John Firriolo, DDS, PhD. The article can be viewed on the Web at http://www.dental care.com/soap/intermed/hyperten.htm.
Untreated hypertension generally has no symptoms — hence it is the "silent killer." Every dental hygienist is educated in hygiene school about taking blood pressures on patients. Blood pressure recordings are taken routinely on every patient seen by dental hygiene student. It is the standard of care. Why is it that so many clinicians neglect this valuable service to patients upon finishing school and entering the real world of clinical practice?
We can offer many excuses as to why we do not take blood pressure. But every obstacle can be met and overcome with planning. Given the dire consequences of undiagnosed hypertension, identifying hypertension is a valuable service that may just save lives. If you are not routinely taking blood pressure, start immediately. Doing less is operating below the standard of care.
Dianne
• Reduce stress and anxiety during dental treatment. Consider the use of N2O-O2 inhalation sedation and/or premedication with oral anti-anxiety medications such as benzodiazepines.
• Do not use local anesthetics with vasoconstrictors in patients with uncontrolled or poorly controlled hypertension. This is defined as any patient with a systolic blood pressure greater than or equal to 180 mmHg and/or a diastolic blood pressure greater than or equal to 100 mmHg.
• For patients with controlled hypertension, where the use of local anesthetics with vasoconstrictors is not contraindicated because of potential drug interactions, limit the total dose of vasoconstrictor to maximum of 0.04 mg of epinephrine (2.2 carpules of 2 percent lidocaine with 1:100,000 epinephrine) or 0.2 mg of levonordefrin (2.2 carpules of 2 percent carbocaine with 1:20,000 levonordefrin).
Dianne D. Glasscoe, RDH, BS, is a professional speaker, writer, and consultant to dental practices across the United States. She is CEO of Professional Dental Management, based in Lexington, N.C. To contact Glasscoe for speaking or consulting, call (336) 472-3515, fax (336) 472-5567, or email [email protected]. Visit her Web site at www.professionaldentalmgmt.com.