by Harriet Kushins, CDA, RDH, BA
Routinely, the dental hygienist is the first person of the dental team to examine the patient, to review medical and dental histories, and to identify any abnormalities of the head, neck and/or oral cavity. A number of oral conditions may be diagnosed, treated, and managed by the dental health professional, including Sjogren's syndrome. Sjogren's syndrome is an oral health condition that requires serious attention.
Sjogren's syndrome is a disorder of the immune system, the body's defense against disease. The immune cells, lymphocytes (type of white blood cells) and plasma cells infiltrate and destroy the salivary and tear glands, as well as other moisture-producing glands, resulting in dryness of the mouth and eyes. The cells cause the glands to stop producing moisture.
Other parts of the body can also be affected. Sjogren's is a slowly progressing, chronic, inflammatory autoimmune disease. An autoimmune disease is an illness in which the body's immune system makes a mistake. For unknown reasons, the immune system begins treating parts of the body as foreign invaders.
Sjogren's syndrome is incurable and can lead to the inflammation of internal organs such as lung and kidney, causing the condition to be a systemic disease.
Sjogren's syndrome was first recognized by a Swedish ophthalmologist, Henrik Sjogren, in 1933 when he reported that patients who had symptoms of dry eyes and mouth were also diagnosed with arthritis. Based on further laboratory testing and examination, he observed that the results disclosed extensive chronic inflammatory cell infiltration in the lacrimal, parotid, sublingual and labial salivary glands. In 1965, Sjogren's syndrome was defined as "the triad of keratoconjunctivitis sicca, xerostomia and rheumatoid arthritis or other connective tissue disease."1 There are three types of Sjogren's syndrome:
• Primary Sjogren's syndrome involves only salivary and tear glands, and it has no other associated disorders.
• Secondary Sjogren's syndrome occurs with other autoimmune disorders such as systemic lupus erythematosus, rheumatoid arthritis, or scleroderma.
• Sicca Complex involves only the eyes and no other organ or tissue.
Speculation on disease origin
The origin of this disease is unknown, yet several possibilities are suspected: viral, hormonal, genetic, and environmental. Some evidence based on immunogenetic studies supports the genetic link predisposing an individual to Sjogren's syndrome. These patients have been found to have an abnormal immunological response to one or more unidentified antigens. These antigens can be viral or virus-altered autoantigens. Epstein-Barr, hepatitis C virus, and other herpes viruses are suspected as possible factors.
There is some speculation, however, that environmental factors trigger the autoimmune system, including irradiation and toxins such as silica dust. Questions continue to be raised concerning what specifically causes the body's immune system to lose tolerance for its own antigens and produce harmful autoantibodies.
Since Sjogren's syndrome occurs more often in women than men, the hormonal factor remains to be explored. Studies continue into the nature of estrogen and androgen and their effects on the immune system.2
What are the clinical symptoms?
Approximately two to four million Americans are afflicted. It affects all races and age groups. Most patients are diagnosed between 40 to 55 years of age. More than 90 percent of patients are women. It rarely affects children. Thirty percent of patients with an autoimmune disorder will also have Sjogren's syndrome.3
Early recognition and identification of symptoms are of special interest to the dental professional. The dental hygienist gives the patient the opportunity to disclose new, undiagnosed health symptoms during the exam. The dental appointment may well be the very first place a problem is noted.
Of great importance is the patient's chief complaint of xerostomia or "dry mouth," a major symptom associated with Sjogren's syndrome. Along with dry mouth, the reduction in salivary flow causes the mucosa to become inflamed, dry, or sticky. The parotid gland is sometimes enlarged and tooth decay is rampant. There is also difficulty in chewing, swallowing, and speaking. Ulcers and other sores of the tongue, lips, and cheek — all connected to the salivary gland's functioning — are observed. Dry, gritty, or itchy eyes, reddened appearance of the conjunctiva, sensitivity to light, a burning sensation, and eye secretions are other clinical symptoms.
The function of the salivary glands and tear glands (glands of lacrimation) is gradually diminished. These symptoms are slow and progressive, but not life threatening. The dental health team can have a major role in assisting the patient in early detection. Because of these oral manifestations, early diagnosis and intervention can slow the impact of symptoms on the mouth and eyes. Treatment reduces the discomfort and complications.
When the medical and dental teams have completed all the test results, and Sjogren's syndrome has been confirmed, management of the dental patient is established. It is important that the dental team continues to be involved in the ongoing treatment of the patient. The teeth, the periodontium, and related problems of the oral and facial areas will need particular attention.
The dental hygienist's role for such a patient begins with a complete oral examination and monitoring of the oral mucosa for candida infection. There is a greater incidence of developing oral candidiasis in patients who have chronic salivary problems. Approximately one-third of patients with chronic hyposalivary conditions develop erythematous oral candidiasis.8
Clinical appearance of a candida infection includes:
• Redness of the oral mucosa
• Angular cheilosis
• Atrophy of the filiform papillae of the tongue
The oral symptoms are:
• Burning sensation of the oral mucosa, change in taste, and acidic or spicy foods are not tolerated well.8 A fungal culture swab specimen from the mucosa can identify the candidiasis condition and the patient can begin treatment with antifungal drugs.8
Nutritional counseling is necessary at each recall visit. Discussion of proper foods and diet and emphasizing what is appropriate for menu planning help patients manage their daily lives.
If dry mouth causes speaking difficulties, a speech pathologist can be suggested to the patient for further evaluation.
Preventing and controlling rampant and recurrent decay is another critical concern that requires attention by the dental hygienist. Recommendations of three- to four-month recall visits are necessary for appropriate oral hygiene follow-up treatments.
The appointment should include a specific fluoride regime using stannous fluoride or neutral sodium fluoride. Patients should be instructed in home care, emphasizing frequent tooth brushing, and/or rinsing after eating and flossing.
Oral irrigation with an alcohol-free antimicrobial rinse can also be beneficial.9 Those patients who show high risk of tooth decay are instructed to apply 1.1 percent neutral sodium fluoride gel daily, in custom-made trays for five to 10 minutes to control tooth decay.8 This neutral sodium fluoride gel is only available by prescription.6
The hygienist is in an advantageous position to ask specific questions of all patients concerning dry mouth, whether the patient complains about it or not.
When a patient complains of dry mouth, eyes, or both, the medical history must be thoroughly reviewed. Attention to conditions of rheumatoid diseases, hepatitis, and Epstein-Barr must be given. Family history update and review also must be included. Current medications need to be discussed because they may be contributing to the symptoms of dry mucous membranes. Antihistamines, diuretics, and decongestant drugs may cause an increase of dry mucous membranes. The dental hygienist should be aware and well informed of all the adverse effects of drugs used by the patient. A knowledgeable dental health professional can make a positive impact to the dental team and to the patient.
Several questions should be directed to the patient to investigate the possibility of Sjogren's syndrome:
• Do you sip liquids to aid in swallowing dry foods?
• Does your mouth feel dry when eating a meal?
• Do you have difficulty swallowing any foods?
• Does the amount of saliva in your mouth seem to be too little or too much?
Positive responses to the first three questions and a response of "too little" to the fourth are indicative of major salivary gland hypofunction.4 A standard group of specific questions should be included in a health questionnaire.
How is a positive diagnosis confirmed?
A complete examination of the mouth, head, and neck is necessary if a patient is suspected of salivary dysfunction. Presently, there are no universal criteria or any particular test for diagnosing Sjogren's syndrome. Therefore, the following tests are recommended:
• A lip biopsy
• A whole salivary flow rate
• Blood tests
• The Schirmer's test.
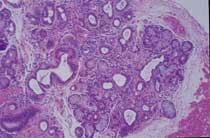
The lip biopsy (inside of the lower lip) is a very specific diagnostic measurement. The biopsy shows any pathological changes in the minor salivary glands determined by the presence of lymphocytes. Lymphocytic infiltration is histologically measured by using a focus score (defined as the number of lymphoid aggregates per mm of tissue). A focus score of more than one is considered highly probable of Sjogren's syndrome.5
The whole saliva measurements of both the major and minor glands are evaluated for salivary function. This test can be performed in the dental office because it is simple and pain-free.
The blood tests performed in a laboratory detect specific markers or autoantibodies (anti -ss -A, anti -ss -B) for rheumatoid factors.6
These two specific autoantibodies are present in more than 80 percent of patients with Sjogren's syndrome.7
The Schirmer's test is used to screen for eye symptoms. The production of tears is measured to determine what is abnormal.4 The procedure involves using a standard strip of filter paper that is placed at the junction of the middle and lateral third of the lower eyelid. After five minutes, the wetting length of the paper is measured. Wetting of less than 5 mm is indicative of diminished tear secretion by the lacrimal glands.5
Research continues in the field of genetics, viral, and environmental factors examining their influences and interaction with the autoimmune pathogens in Sjogren's syndrome. Knowledge of all oral manifestations of connective tissue diseases along with any subtle oral changes observed by the dental hygienist will enable the health professional to assist patients in proper treatment and therapy in a timely manner. Since the cause of Sjogren's syndrome remains unknown, it is the responsibility of the dental hygienist to attentively listen to all complaints mentioned by the patient, especially with xerostomia and related oral symptoms. The support of the dental and medical teams, family, and friends will make the difference in the approach and attitude that the patient will take in managing and living with Sjogren's syndrome.
For additional information, the dental hygienist can visit the Sjogren's Syndrome Foundation at www.sjogrens.com. The foundation provides education, research, and health-care modalities for patients.
The following is an abbreviated list of recommendations that the dental hygienist can share with a Sjogren's syndrome patient to alleviate discomfort:
• Moisten lips using petroleum-based lubricant
• Drink sugar-free beverages
• Chew sugarless gum and eat sugarless candy
• Sip small amounts of water throughout the day
• Avoid spicy and acidic foods
• Avoid sticky, sugary foods
• Use specific toothpaste and gels available for dry mouth
• Use saline nasal spray to moisten nasal passages
• Use a humidifier all year
• Use artificial tear products16
Harriet H. Kushins, CDA, RDH, BA, is an adjunct clinical instructorat both University of Medicine & Dentistry of New Jersey, Newark, N.J., and at Bergen Community College, Paramus, N.J.She is currently teaching radiology lab and clinical practice.
References1. Aguire A. Recognizing and managing the oral clues that point to Sjogren's syndrome. Medscape Women's Health. 2(9). 1997:>http://www.medscape.com/medscape/Women's Health Journal. Accessed April 30, 2001.
2. Vale DL. Recognition and management of Sjogren's syndrome. The Nursing Clinics of North America. March, 2000; 35(1): 267-78.
3. Sjogren's syndrome, Gale Encyclopedia. 1999, Vol. 4: 2636-2637.
4. Fox PC, Brennan M, Pillemer S, Radfar L, Eds., Sjogren's syndrome: A Model for Dental Care in the 21st Century, JADA. June, 1998: 721.
5. Gobetti JP, Froeshle ML. Sjogren's syndrome: A Challenge for Dentistry, Journal of the Academy of General Dentistry. May-June, 1997; 45(3): 268-72.
6. Fox PC, Atkinson JC. Sjogren's Syndrome: Oral and Dental Considerations, JADA. March, 1993: 78.
7. Atkinson JC, Wu AJ. Salivary Gland Dysfunction: Causes, Symptoms, Treatment, JADA. April, 1994: 412.
8. Carsons S, Harris EK, Eds., The New Sjogren's Syndrome Handbook, (New York: Oxford Press, Inc. 1998): 158.9. Thomas Jefferson University Hospital. Fact Sheet: Sjogren's Syndrome, 20, 2000: http://www.jeffersonhealth.org.Bibliography
• Aguire, Alfredo: Recognizing and managing the oral clues that point to Sjogren's syndrome. Medscape.com/medscape/Womens Health Journal. Accessed April 30, 2001.
• Alexander, Elaine L. Why is Sjogren's Syndrome Under-Recognized? The Moisture Seekers Newsletter, September 1992: 9.9.
• Atkinson, Jane C. and Philip Fox. Sjogren's Syndrome: Oral and Dental Considerations. The Journal of the American Dental Association, 124 (1993): 74-86.
• Carsons, Steven, Ed. and Elaine K. Harris, Ed. The New Sjogren's Syndrome Handbook. New York: Oxford University Press Inc., 1998.
• Cook, Allan R., Ed. Oral Health Sourcebook. 5 vols. Detroit: Omnigraphics, Inc., 1998.
• Dauphin, Sue. Sjogren's Syndrome: The Sneaky "Arthritis." Tequesta, Florida: Pixel Press, 1993.
• Fox, Philip C., Michael Brennan, Stanley Pillemer, Lida Radfar. Sjogren's syndrome: A Model for Dental Care in the 21st Century. The Journal of the American Dental Association. 129 (1998): 719-728.
• Gobetti, John P. and Mary Lynn Froeschle, Sjogren's Syndrome: A Challenge for Dentistry, Journal of the Academy of General Dentistry. May-June, 1997: 45(3): 268-72.
• Grominica-Ihle, Erika. Sjogren's Syndrome - Diagnosis and Therapy: The Clinical Picture. BT: Biomedical Therapy. (1997): 54-59.
• Olendorf, Donna, and Christine Jeryan, Eds. The Gale Encyclopedia of Medicine. 5 vols. Detroit: Gale Research Company, 1999.
• Tanzen, Jason M. Problems as Associated with Dry Mouth of Sjogren's Syndrome. Sjogren's Syndrome Foundation Newsletter Library. July/August. 1994: 1-4.
• Thomas Jefferson University Hospital. Jefferson Health System Fact Sheet: Sjogren's Syndrome. 20 Sept. 2000:
• Vale, Donna L. Recognition and management of Sjogren's syndrome. The Nursing Clinics of North America. March, 2000; 35(1): 267-78.