The goal of instrument processing is to provide sterile instruments at chairside for use on the next patient. Instrument sterilization is an essential part of a dental practice’s infection control program, and must be performed properly to better ensure patient and practitioner safety.
Improper technique can lead to a variety of difficulties. For example, instruments may be damaged, discolored, dulled, or even experience rusting during sterilization, especially if processed through a steam autoclave.
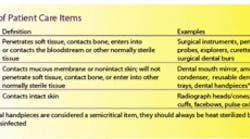
Categories of patient care items
The Centers for Disease Control and Prevention (CDC) have categorized patient care items as critical, semicritical, or noncritical based on the potential risk of infection to patients during their use. The CDC uses a classification system based on one first proposed by Spaulding in 1968 (Table I). The CDC recommends that all critical and semicritical items first undergo a thorough cleaning followed by sterilization, preferably by heat.
Semicritical items that are heat-sensitive must undergo, at a minimum, cleaning and treatment with a high-level disinfectant.
Cleaning followed by treatment with a low-level disinfectant when no blood is visible is appropriate for noncritical items. Intermediate-level disinfectants must be used when blood can be seen.
Sterilization of dental instruments
Instrument preparation involves seven sequential activity sets:
• Chairside and transport
• Holding (presoaking)
• Cleaning
• Corrosion control/drying/lubrication
• Packaging
• Processing
• Storage
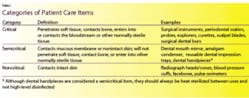
One must perform processing correctly to keep instrument damage to an absolute minimum. Instrument processing can harm instruments. However, there are steps that keep damage at a minimum (Table II). There are protective procedures for each step of instrument sterilization.
Corrosion associated with moisture and heat affects stainless steel instruments less than some carbon steel instruments. Some instruments are made of stainless steel but have carbon steel cutting edges because they keep their sharpness longer.
Unfortunately, carbon steel has a tendency to corrode and lose sharpness during stream sterilization. Rust-inhibiting dips and sprays can reduce corrosion. Processing in unsaturated chemical vapor or dry heat generally produces less rusting and dulling of carbon steel items. Generous rinsing during holding and cleaning will help remove biological debris and chemicals that could reduce sterilization efficiency and instrument integrity.
Sharpening instruments chairside
So, how can we maintain aseptic technique and sharpen instruments effectively chairside? We all know that sharp instruments increase our efficiency with scaling, debridement, and root planing. Sharp instruments are also critical for enhancing the level of patient comfort, reducing fatigue, enhancing tactile sense, and increasing refined manipulation. Sharp instruments also decrease the likelihood of the dreaded burnished calculus.
The ideal safety recommendation would be to clean, sterilize, sharpen, and resterilize the instruments before the patient arrives. It would be prudent to have a variety of individually wrapped, sterilized sharp instruments to replace dulled instruments during patient treatment. This is a safer option compared to sharpening orally contaminated instruments chairside. Sharpening of contaminated instruments presents an increased risk for disease transmission through an occupational exposure - cut, abrasion, or puncture.
If you must sharpen chairside with a seated patient, there are techniques to diminish risk. These include:
• Performing sharpening procedures away from the patient’s view
• Use armamentarium that can be completely (and easily) sterilized
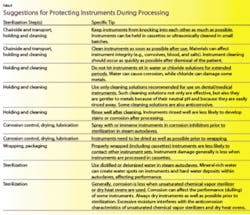
• Use safe, stable sharpening techniques. First, start with a clean stone. Wash or, better yet, ultrasonically clean sharpening stones before sterilization (steam, chemical vapor, or dry heat).
Again, any sharpening aid, template, or device you may consider using at chairside must also be able to survive sterilization - not merely disinfection, but sterilization (Table III). Dissemble sharpening devices and sterilize each part after each use.
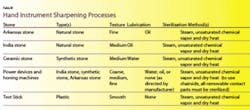
Sharpening techniques are as varied as the instruments themselves, but when using manual stones you must first decide whether to sharpen by moving the stone or by moving the instrument. Always refer to the manufacturer’s guidelines for power-sharpening devices and sharpening templates. Either method requires a stable, well lighted, protected working surface to ensure control of sharpening strokes, to aid in maintaining integrity of instrument design, and to guard against injury. Secure a protective cover to a flat surface (countertop) with tape. A ceramic stone is best for chairside sharpening because the lubricant used is water. Steam autoclaves can sterilize water. Natural stones require oil lubricants, which cannot undergo sterilization. Thus, natural stones are less desirable for chairside sharpening while treating patients.
Moving the stone
When choosing to move the stone rather than the instrument, place your arm flat on the stable surface, hold the instrument in the palm of your nondominant hand, and secure the instrument with your thumb. The surface requiring sharpening will be lower than the countertop edge and will face your dominant hand. Adjust the angle of the cutting edge, not the handle, perpendicular to the flat table surface.
It is critical that you recognize the instrument design in order to keep the intended cutting edge intact. Hold the stone in your dominant hand and begin to move the stone in an up-and-down motion, following the lines of the cutting edge. To avoid injury, hold the stone on the edges so that your fingertips do not risk coming into contact with the instrument blade.
Evaluate your efforts with a sterile test stick, remembering to test stroke away from you and with fingers clear from the direction of the stroke. Carefully wipe residual materials from the instrument, using double or triple gauzes.
At the end of the appointment, discard the protective cover, scrub or ultrasonically clean the sharpening stones, wipe them dry, and place the stones in an instrument cassette or package for sterilization.
If choosing to move the instrument over the stone, place the stone on a protected flat surface and move the instrument over the stone toward you. Most instruments can be sharpened by placing the stone either perpendicular to the countertop edge or parallel to the edge. With this technique, you will have to change your body position to allow for the best view of the cutting edge. Use a finger or hand fulcrum to prevent instrument slippage and to guide the instrument in a continuous controlled sweep over the stone.
Unless the instrument is in need of recontouring, use only light to moderate pressure. Stabilize the stone with your nondominant hand, making sure to keep fingertips clear of the direction of the sharpening stroke.
No matter what your preferred method of sharpening, all chairside methods carry the risk of injury. By following simple guidelines for caution, you can protect yourself from disease-promoting injury or merely the inconvenience of a sore finger.
Elizabeth Hughes, RDH, MS, is clinical assistant professor at Indiana University School of Dentistry in the Department of Periodontics and Allied Dental Programs.
Charles John Palenik, MS, PhD, MBA, is professor of oral microbiology and director of Infection Control Research and Services at Indiana University School of Dentistry.
Questions concerning this article or any infection control issue can be electronically submitted to [email protected].
Suggested Reading
Darby M, Walsh M. Dental Hygiene Theory and Practice. 2nd Edition. Saunders, St. Louis, MO, 2003.
Marquam B. Keep an eye on sharpening techniques to prevent disease transmission. RDH 12: 20-23, 1992.
Miller CH, Palenik CJ. Infection Control & Management of Hazardous Materials for the Dental Team. 3rd Edition, Elsevier Mosby St. Louis, MO, 2005
Nield-Gehrig JS. Fundamentals of Periodontal Instrumentation & Advanced Root Instrumentation.5th Edition, Lippincott Williams & Wilkins, Baltimore, MD, 2004.
Rossi R, Smukler H. A scanning electron microscope study comparing the effectiveness of different types of sharpening stones and curettes. J Perio 66:956-961,1995.
Stach DJ, et al. Effect of repeated sterilization and ultrasonic cleaning on curette blades. J Dent Hyg 69: 31-39, 1995.
Hutcheson CL. Taking care of your instruments, what you need to know to protect your instruments and your patients. Dent Equip & Mater 9:22, 2004.
Organization for Safety & Aseptic Procedures. From Policy to Practice: OSAP’s Guide to the Guidelines. OSAP, Annapolis, MD, 2004.