Implant Dentistry is becoming a highly accepted and viable option for natural tooth replacement. In 2005, the United States dental implant and final abutment market, comprised of regular (> 3.0mm) and small (<3.0 mm) diameter dental implants and abutments, was valued at $488.7 million.1 With the increase in our aging population - combined with dental implant systems becoming more streamlined - the projected market growth could be $868.8 million by 2010.1
Although the success of dental implants is steadily improving and considered permanent tooth replacement, failure of dental implants can result from many sources. The primary cause is unsuccessful ossteointegration of the implant, and the second leading cause is bacterial infection.2, 3 Peri-implantitis is defined as “an inflammation of the tissue around a dental implant.”4 It can develop when bacterial microorganisms and their by-products are allowed to accumulate around the implant site similar to periodontal disease in natural teeth.
The micro-flora found in the peri-implant sulcus is similar to those found in the natural dentition sulcus. In a diseased peri-implant site, gram-negative rods and spirochetes - similar to those found in chronic periodontal disease - can be present. This could include Prevotella intermedia, Fusobacterium nucleatum, and Prophyromonas gingivalis.5, 6 Meffert in 1996 concluded that “periodontis equals peri-implantitis in etiology and therapy.”7
Therefore, a recare maintenance program is critical to the long term success of dental implants as well as overall oral health.
The benefit of ultrasonic instrumentation
Ultrasonic instrumentation has been shown to be as effective as hand scaling in nonsurgical periodontal therapy.8 Moreover, the acoustical streaming, acoustical turbulence, and cavitational effects produced by ultrasonic instrumentation, have a positive impact in the reduction of oral micro-flora.9 Baehni reported in 1992 that spirochetes and motile rods in a periodontal pocket were reduced to 0.1 percent after exposure to ultrasonic vibrations.10 Therefore, the conclusion can be drawn that ultrasonic scaling around dental implants will alter the micro-flora in the peri-implant sulcus accordingly.
The lack of an ultrasonic insert designed for safe use on implants has prohibited the incorporation of ultrasonic therapy into implant maintenance procedures. With the recent launch of ultrasonic inserts designed specifically for implant maintenance, the ability to incorporate power instrumentation into implant maintenance therapy will become standard of care. With these specially designed inserts, the proven benefits of ultrasonic instrumentation in the disruption of plaque, biofilm, calculus, and endotoxins can now be incorporated into implant maintenance procedures.
Currently, the two manufacturers offering these specialty inserts are DENTSPLY Professional and the Tony Riso Company. Both of these inserts are designed for use with magnostricitive technology. The Cavitron® SofTip™ Implant Insert by DENTSPLY has a resin grasp and Thru Flow® water port. The Titanuim Implant Scaler by the Tony Riso Company is designed with an external water port. Both inserts have a single-use, disposable plastic tip that is placed securely over the metal tip on the insert. This simple assembly process is required prior to using the insert, and instructions are included in the package.
Technique for implant debridement
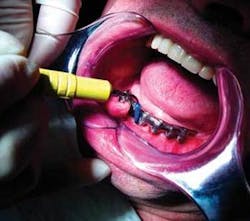
The instrumentation technique utilized for implant debridement is similar to the technique used with other ultrasonic inserts. The operator should use a gentle, modified pen grasp with light pressure, and establish a stable intraoral or extraoral fulcrum. Since calculus and biofilm can not adhere as tightly to the smooth implant surface, it is recommended that the implant insert be used at a low power or BlueZone™ setting, and at the lowest power setting possible within that zone to debride the site.
Adaptation is similar to other inserts. Activate the insert before adapting to the implant surface to ensure patient comfort. Minimize tissue distension by entering with the tip parallel to the long axis of the implant when instrumenting subgingivally. Overlapping horizontal, vertical, or oblique strokes can be utilized in the instrumentation process.
Magnetostrictive technology creates an elliptical stroke pattern, allowing for four active sides on the tip area. It is recommended that the two lateral sides and the back be adapted to the implant surface for maximum efficiency and patient comfort.
Caution needs to be taken so the point of the insert is not directed into the implant surface as this can cause damage to the outer surface of the implant or abutment. A light touch will help ensure that the implant fixture will maintain its structural integrity, and not experience excessive vibration which could comprise the stability of the implant.
The patient’s home care also impacts the health of the implant site. It is critical for the dental hygienist to educate the patient on proper techniques and products, which will assist with their self-care. Specific techniques and modifications to home-care products, such as bending brush handles, may need to be implemented, since the design of the implant restoration may be different than the design of a natural tooth. Currently, options are available on the market to meet these needs - a variety of interdental brushes, various floss designs and materials, and an assortment of power or manual toothbrushes.
Research, evidence, and experience have proven that dental implants are a viable option for tooth replacement. To increase the long-term success of dental implants, it is important to utilize appropriate maintenance techniques to ensure their success. Specially designed ultrasonic implant inserts gives the dental professional another option in providing optimal maintenance therapy for our dental implant patients.
References
1. Millennium Research Group. (2006) US market for dental implants 2006. Toronto, ON
2. Scarano A, Piattilli M, Vrespa G, Caputi S, Piattelli A. Bacterial adhesion on titanium nitride-coated and uncoated implants: An in vivo human study. J Oral Implant 2003; 29:80-85.
3. Becker W, Becker BE, Newman MG, Nyman S. Clinical and microbiologic findings that may contribute to dental implant failure. Int J Oral Maxiollfac Implants. 1990; 5:31-38.
4. Wilkins E. (2005). Clinical Practice of the Dental Hygienist. Baltimore: Lippincott Williams & Wilkins
5. Maksoud M. Manipulation of the Peri-Implant tissue for better maintenance: a periodontal perspective. J Oral Implant 2003; 29 120-123
6. Chen S, Darby I. Dental implants: Maintenance, care and treatment of peri-implant infection. Australian Dental Journal 2003; 48:4 212-220.
7. Meffert R. Periodontitis vs. peri-implantitis: the same disease? The same treatment? Oral biology & Medicine. 1996; 7:278-291
8. Drisko, CH., et al Sonic and ultrasonic scalers in periodontics. J Periodontal (2000): 71; 1792-1801.
9. Drisko CH. Root instrumentation. Power driven vs. manual scalers, which one? Dent Clin North Am. 1998 Apr; 42(2): 229-244.
10. Baehni B, Chapuis B, et al. Effects of ultrasonic and sonic scalers on dental plaque microflora invitro and invivo. J Clin Periodontal. 1992: 19: 455-459
Shirley Branam, RDH, MBA, is the Central Clinical Educator for DENTSPLY Professional. She received her bachelor’s in dental hygiene from the University of Michigan and continued on to complete a master’s degree in health care management from the University of Phoenix. Shirley’s background includes over 20 years in clinical and educational experience in the dental assisting and dental hygiene professions. While a member of the University of Michigan School of Dentistry, she held various appointments including hygiene faculty member, staff hygienist in the Graduate Prosthodontic Clinic, and research Coordinator. Her areas of expertise include clinical dental hygiene, biomaterials, implants, local anesthesia, and nitrous oxide sedation. She currently lectures for DENTSPLY Professional, covering topics on ultrasonic and hand instrumentation, principles of ergonomics, and optimizing caries risk reduction.