Mucous membrane pemphigoid
by Nancy Burkhart, RDH, EdD
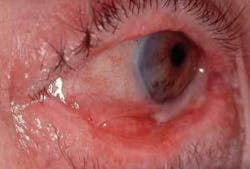
Presentation: A 50-year-old woman is your patient today. “Ann” is a maintenance patient that you have treated for the past year, and her last recall was a little over six months ago (Figure 1).
Notes and findings: Ann has complained about spontaneous bleeding of the gingiva for a couple of years and reports the bleeding occurs with normal brushing. She also tells you that the raw, red surfaces are very painful. Although she is not classified as a periodontal patient, she has some 4 mm bone loss in the molar regions and notable areas of recession. You noticed in her records that the previous hygienist used an ultrasonic cleaner and an air polisher during her procedures. The patient complained that it was quite painful after her maintenance appointments and requested that they not be used during subsequent appointments. She also has some papules on the skin that have recently occurred, and she tells you that she plans to see her dermatologist.
The patient takes the following medicines: Synthroid, ibuprofen, and multivitamin supplements.
Clinical impressions: The gingiva appears inflamed with marginal irritation and loss of stippling. Generally, the tissue appears edematous and exhibits a Nikolsky sign (stripping of the epithelium when sliding pressure is applied) in several gingival areas.
Diagnosis: Mucous membrane pemphigoid (benign mucous membrane pemphigoid, cicatricial pemphigoid).
Etiology: Mucous membrane pemphigoid (MMP) is a vesiculobullous disease and is classified as an autoimmune disease. Approximately 85 percent of patients with MMP have oral involvement. When affecting the gingiva, MMP is often referred to as desquamative gingivitis, which is a general term suggesting inflammation and sloughing of the gingiva. Pemphigoid-like lesions have been reported as drug-induced in some cases by such medications as carbamazepine, clonidine, or penicillamine. In other cases, a direct cause is unknown, other than MMP is believed to be an autoimmune response.
Method of transmission: There is no contagion factor.
Pathogenesis: Mucous membrane pemphigoid is rare in children and tends to affect women most often in the fifth decade of life. As with most autoimmune disorders, women are affected more often than males and, in the case of MMP, by a 2 to 1 ratio. Additionally, MMP most often involves the oral cavity followed by the conjunctiva and genitalia. MMP is caused by antibodies that target the basement membrane and weaken the underlying attachment to the connective tissue. A similar condition is bullous pemphigoid that affects an older group of individuals usually in the seventh to eighth decade of life and primarily affects the skin, although oral lesions are occasionally found.
Perioral and intraoral characteristics: The gingiva is the target site for MMP and has the appearance of generalized gingivitis exhibiting sloughing. The tissue is easily injured by food, brushing, and even through preventive maintenance when prophylaxis is administered. The tissue is very fragile and may strip with any pressure, leaving a raw surface that is termed Nikolsky’s sign (the epidermis can be separated at the basal layer and rubbed off when pressure is applied in a sliding motion).
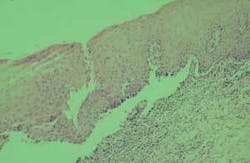
Extraoral characteristics: Although the oral tissues are involved most frequently, the skin, genitalia, nares, rectum, urethra, and esophagus may also be involved. The eyes may form symblepharon, entropion (the enfolding of the eyelid), scarring and blindness. Referral for professional eye examinations is crucial (Figure 2).
Distinguishing characteristics: Stripping of the epithelium and the presentation of chronic gingival inflammation are distinguishing characteristics. However, confirmation cannot be made without other tests.
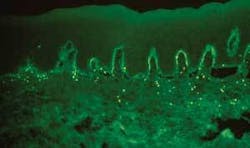
Significant microscopic features: (Figure 3) Subbasal separation of the epithelium from the underlying connective tissue is characteristic. Immunofluorescence is positive and demonstrates a linear pattern of IgG and complement in the basement membrane.
Differential diagnosis: Pemphigus vulgaris, bullous pemphigoid, pemphigus, erosive lichen planus, erythema multiforme, discoid lupus erythematosus, and allergy-type responses such as contact allergies would be considerations. Many mucosal diseases appear very similar; therefore, a complete diagnosis cannot be made without utilizing several clinical tests such as viewing the tissue histologically (under the microscope) and using immunofluorescence to confirm the diagnosis. The patterns viewed in immunofluorescence will present with different staining variations depending upon the disease state. As seen in the slide, the basement membrane is targeted which has weakened the attachment to the underlying connective tissue. The fluorescent antibodies C3 and Immunoglobulin (IgG) and fibrin at the basement membrane, form a linear pattern of fluorescence (Figure 4). Using immunofluorescence in conjunction with the histological and clinical appearances is true confirmation of the diagnosis.
Treatment and progress: Most patients with gingival disorders such as MMP have difficulty in maintaining good oral hygiene and need to be seen frequently for prophylaxis. Procedures should be performed as atraumatically as possible. Patients may have other disease states in addition to MMP such as contact allergies and other vesiculobullous diseases. Although MMP is a benign process, a patient may develop other disease states that may be different than the original diagnosed disease. The development of dysplasia, cancer in situ and carcinoma should always be considered in long-term erosive diseases that progress and do not heal.
As with most of the mucosal diseases, exacerbation and remission are common themes and this failure of a final treatment is very frustrating for the patient. As the lesions improve, the patient may believe that the disease has been “cured” and then a bout of discomfort appears that may last for some time. Mucosal diseases are difficult for the practitioner as well, since dental practitioners are most satisfied with case-closed procedures.
Assessment of the home-care practices, types of products used by the patient and a diet analysis should be performed. The tissue of patients usually responds better when a soft bristle brush and an antimicrobial rinse are used. Some common allergens related to dental products may play a role in the inflammatory process in any mucosal disease. These may be toothpaste and mouth rinses containing sodium laurel sulfate, and hidden flavoring agents such as cinnamon, wintergreen, and spearmint. Many flavoring agents are contained in food products as well. Additionally, preservatives may be a problem for some patients and these often go undiagnosed. Salsa, processed foods, and colas are often contributors because of the preservatives and flavoring agents for patients who are sensitive to these additives.
As with most mucosal lesions, a picture is worth a thousand words, and intraoral photography is a great asset in evaluating the tissue during each appointment. Maintenance appointments should occur every three to four months with as little disruption to the tissue as possible, using nonabrasive products for prophylaxis.
Corticosteroids are often used to control the erosive lesions of mucous membrane pemphigoid. Along with topical corticosteroids, intralesional, or systemic corticosteroids are other modes of treatment. Because candida infections often result with the long-term use of corticosteroids, nystatin and other antifungal treatment are often needed as well. Sometimes in long-term treatment, antifungal medications are used in conjunction with corticosteroids when patients are prone to these infections.
References
• Endo H, Rees TD, Kuyama K, Kono Y, Yamamoto H. Clinical and diagnostic features of mucous membrane pemphigoid. Compend Contin Educ Dent. 2006 Sep;27(9):512-6; quiz517-8.
• Fatahzadeh M, Radfar L, Sirois DA. Dental care of patients with autoimmune vesiculobullous diseases: case reports and literature review. Quintessence Int. 2006 Nov-Dec;37(10):777-87.
• Plemons JM, Gonzales TS, Burkhart NW. Vesiculobullous diseases of the oral cavity.Periodontology 2000.1999; 21:158-175.
• Tricamo MB, Rees TD, Hallmon WW, Wright JM, Cueva MA, Plemons JM. Peridontal status in patients with gingival mucous membrane pemphigoid. J Periodontol. 2006 Mar;77(3:398-405.
Nancy Burkhart, RDH, EdD, is an adjunct associate professor in the Department of Periodontics at Baylor College of Dentistry, Texas A&M Health Science Center in Dallas. Nancy is also a co-host of the International Oral Lichen Planus Support Group through Baylor (www.bcd.tamhsc.edu/lichen). She can be contacted at [email protected].