Geographic Tongue
by Nancy W. Burkhart, RDH, EdD
Your patient is a 34-year-old male, Mr. Evans, who has noticed that his tongue feels rough and has a strongly delineated white lined appearance. He is worried about the possibility of cancer since he has had a relative who developed oral cancer. He also reports that his wife has commented on the gross appearance of his tongue and is very concerned about his wife's comment.
As you examine his mouth, you notice that his tongue does appear red, and white, raised lines extend from the lateral border/tip region to the middle dorsum of the tongue (see Figure 1). He reports no pain, but has noticed a difference in appearance each time he checks the tongue. He wants to know what disease he has and what he can do to get rid of the ugly pattern.
Etiology: Geographic tongue is a benign condition that has been associated with emotional stress, allergies, diabetes, hormonal factors, and vitamin deficiency. Genetic predisposition has been reported, along with a specific association in those individuals with hereditary cutaneous disorders such as psoriasis and pityriasis. To date, no conclusive evidence supports any of the above-mentioned etiologies.
Epidemiology: Geographic tongue is reported in approximately 1% to as high as 3% of the population. It is more frequent in females with reports of a ratio of 2:1. Found mostly in adults, its presence has been reported in some children as well and recently reported in association with Robinow's syndrome (Cerqueira and de Souza, 2008) and periodic fever syndrome (Beiraghi et al. 2007). Shulman and Carpenter (2006) found a lower rate of geographic tongue in cigarette smokers with a more prevalent rate in whites and blacks compared to Mexican Americans.
Method of transmission: Geographic tongue is not contagious and cannot be given to another person.
Pathogenesis: The pathogenesis of erythema migrans is unknown, but the literature suggests that there may be a hypersensitivity to environmental factors, and possibly an association with hormonal factors since pregnancy and birth control have been reported to improve the condition. Geographic tongue has been linked to psoriasis, seborrheic dermatitis, and Reiter's syndrome with conflicting and inconclusive evidence.
Perioral and intraoral characteristics: The clinical presentation of geographic tongue has the appearance of patches with denuded filiform papillae on the dorsal surface of the tongue. The denuded areas are surrounded by a light yellow to white colored ring (see Figure 2). The denuded areas tend to migrate and to change patterns throughout the tongue region.
Additionally, the lesions may appear not only on the tongue, but they may occur on the buccal mucosa, lip, and the floor of the mouth. When lesions are found in areas other than the tongue, the term geographic stomatitis is used. Patients often may complain of burning or pain, but, in many cases, there are no symptoms or discomfort. Fissuring has been reported in some cases of geographic tongue, but there has been no definitive association of fissuring and geographic tongue reported.
Distinguishing characteristics: The characteristic red, atrophic patches with concentric yellow outlines around the denuded patches are characteristic. Although the concentric circles are characteristic, geographic tongue may have many varying appearances (see Figures 3, 4, 5).
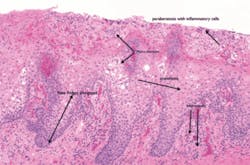
Significant microscopic characteristics: Micro abscesses are microscopically diagnostic of geographic tongue (called abscesses of Munro), inflammatory cells, and obvious loss of the epithelial surface in areas of the clinically denuded patches. The histological appearance of geographic tongue is microscopically similar to cutaneous psoriasis (see Figure 6).
Dental implications: The psychological aspect of geographic tongue is a prime consideration in consoling and reassuring the patient. Some clinicians may biopsy the areas in order to provide conclusive evidence for the patient rather than relying on the clinical presentation. In addition, some lesions that do not present with a textbook appearance may need further evaluation with a biopsy.
Differential diagnosis:
- Candida
- Lichen planus
- Reiter syndrome
- Anemia
- SCC should always be ruled out
Treatment and prognosis: We are witnessing an increase in oral cancer especially in younger individuals with no risk factors. One oral area being reported with increased malignancy is the tongue and any unusual or persistent lesions should be fully evaluated. Digital photography is beneficial in assessing tissue changes over time and the newer screening devices may provide further assurance of changes as well.
Sodium bicarbonate rinses may be recommended, as well as some antibacterial rinses. In cases where candida is present, antifungal rinses are needed; and on occasion, topical corticosteroids may be needed for treatment of ulcerative type lesions. Evaluation of sensitivity to flavoring agents, toothpaste, and other products is beneficial.
Geographic tongue is one of remission and exacerbation with unpredictable recurrences. This aspect is often psychologically difficult for the patient, as are most disorders where remission and subsequent recurrences are noticed.
About the Author
Nancy Burkhart, RDH, EdD, is an adjunct associate professor in the Department of Periodontics at Baylor College of Dentistry and Texas A & M Health Science Center in Dallas. Nancy is also a cohost of the International Oral Lichen Planus Support Group through Baylor (www.bcd.tamhsc.edu/lichen). She is the coauthor of General and Oral Pathology for the Dental Hygienist, published by Lippincott Williams & Wilkins in Baltimore, which was released in October 2007. She can be contacted at [email protected].
References:
Beiraghi S, Myers SL, Regelmann WE, Baker S. Oral Manifestations of a possible new periodic fever syndrome. Pediatr Dent 2007 Jul-Aug.;29(4):323-6.
Cawson RA, Odell EW. Essentials of Oral Pathology and Oral Medicine. 6th ed. Churchhill Livingstone, London. 1998.
Cerqueira DF, de Souza IP. Orofacial manifestations of Robinow's syndrome: a case report in a pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008 Mar:105(3):353-7.
Delong L, Burkhart NW. General and Oral Pathology for The Dental Hygienist. Lippincott, Williams & Wilkins, Balimore. 2007.
Eisen D. & Lynch DP. The Mouth: Diagnosis and Treatment. Mosby, St. Louis. 1998.
Regezi JA, Sciubba JJ, Jordan RCK. Oral Pathology: Clinical Pathologic Correlations. 4th ed. Saunders, St. Louis. 2003.
Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. W.B Saunders Company, Philadelphia. 1995.
Shulman JD, Carpenter WM. Prevelance and risk factors associated with geographic tongue among US adults. Oral Disease 2006 Jul;12(4): 381-6.