The evolution of analgesia and anesthesia in oral health care
by Maria Perno Goldie, RDH, BA, MS
Control of pain is a large component of dental hygiene and dental procedures. Patient comfort is essential to create an aura of trust and feeling of comfort for the patient. In addition to commonly used local anesthetics and nitrous oxide/oxygen sedation, narcotics, hypnosis, virtual reality, and nonpharmacologic analgesics have been shown to be effective for dental pain. This article will discuss the evolution of analgesia and focus on local anesthesia in oral health care.
History
The history of modern anesthesia can be traced back to medieval times. The use of narcotics to reduce pain was a universally accepted practice. Mandrogora, cannabis, hembane, opium, and alcohol were used most frequently.1 These drugs were addictive, caused adverse side effects, and did not meet the necessary standard of care. Efforts to minimize pain were not confined to the inhalation drugs in the early days of anesthesia. Pressure on blood vessels, local applications of ice water, ethyl chloride spray, and sometimes a crack on the head with a mallet were among the methods employed to reduce pain during an operation!
Prior to the introduction of ether by Morton in 1842 and nitrous oxide by Wells in 1844, little could be done to lessen the discomfort associated with the performance of dental and other oral procedures. These agents were used mainly for analgesia or anesthesia during extractions and other surgical procedures, and most patients did not experience anesthesia for other types of dental procedures (such as restorative) until after the introduction of conduction anesthesia in the late 1800s.2 In 1884, Carl Koller discovered the analgesic properties of cocaine.3 Shortly after, in that same year, William S. Halsted introduced conduction anesthesia by using cocaine to block the inferior alveolar nerve. Although cocaine was effective for achieving profound anesthesia, it was found to be highly addictive. In about 1905, procaine was created by Einhorn and Uhfelder in Germany. When mixed with a very small proportion of epinephrine, this agent was found to be highly effective and safe as a local anesthetic agent for most patients. Procaine (Novocaine®) was widely used by physicians and dentists into the 1950s, and Novocaine is still the name that patients commonly associate with local anesthetics. By the 1950s, lidocaine (Xylocaine®) became widely accepted. Although many other local anesthetic agents are currently in use and nitrous oxide is often used for its analgesic effect, lidocaine is still one of the principal anesthetics in use today.
Local anesthetics
Local anesthetics are deposited near a nerve between the site to be anesthetized and the brain, and serve as a chemical barrier that prevents the pain impulse from reaching the brain. By definition, local anesthesia is an anesthetic drug that inhibits nerve excitation or conduction.4 Anesthetics used today in North America are: Lidocaine HCl 2% plain; Mepivacaine HCl 3% plain; Prilocaine HCl 4% plain; Intermediate duration — with vasoconstrictor; Articaine HCl 4% + epinephrine 1:100,000; Articaine HCl 4% + epinephrine 1:200,000; Lidocaine HCl 2% + epinephrine 1:50,000; Lidocaine HCl 2% + epinephrine 1:100,000; Mepivacaine HCl 2% + levonordefrin 1:20,000; Prilocaine HCl 4% + epinephrine 1:200,000; and Bupivacaine HCl 0.5% + epinephrine 1:200,000.
A new product, phentolamine mesylate (OraVerse™), is an injectable that accelerates reversal of soft–tissue anesthesia.5 It produces an alpha–adrenergic block of relatively short duration resulting in vasodilatation when applied to vascular smooth muscle. The median time to recovery of normal lip sensation was significantly reduced for patients treated with phentolamine mesylate compared to the control group: 50 vs. 133 minutes for the maxilla, a 62% reduction, and 70 vs. 155 minutes for the mandible, a 55% reduction. In mandibular procedures, the median time to recovery of normal tongue sensation was reduced 52%, 60 vs. 125 minutes. There were no serious adverse events and no discontinuation due to adverse events. The majority of adverse events were mild and resolved within 48 hours.6
As with any product, safety is of utmost concern. Tachycardia, bradycardia, and cardiac arrhythmias may occur with the use of phentolamine or other alpha–adrenergic blocking agents. Although such effects are uncommon with OraVerse (phentolamine mesylate), clinicians should be attentive to the signs of these events, predominantly in patients with a history of cardiovascular disease. Following parenteral use of phentolamine at doses between five to 15 times higher than the recommended dose of OraVerse, myocardial infarction and cerebrovascular spasm and occlusion have been reported, usually in association with marked hypotensive episodes producing shocklike states. See the full prescribing information before use of the product.7
Another landmark product is the STA™ System, or the Single Tooth Anesthesia (STA) System from Milestone Scientific.8 It is a computer–controlled local dental anesthetic system where just one injection at a single tooth is delivered, and can be used for multiquadrant cases. STA has real–time visual and audible feedback technology, allowing the clinician to easily obtain proper needle placement between the tooth and bone. Called the “magic wand” by some, it has been shown to reduce the likelihood of disruptive behaviors during the initial moments of an injection in children.9 When delivering a traditional mandibular alveolar block, analgesia was less painful when using the Wand than when using a traditional syringe.10
Oraqix
Last, but certainly not least, this is a product that the author refers to as “the best thing since sliced bread”! Needle–free Oraqix® (Dentsply Pharmaceutical, York, Penn.), a subgingival local anesthetic, is primarily for adults who need localized anesthesia in periodontal pockets during scaling and/or root planing. Oraqix is a gel, containing lidocaine 25 mg/g plus prilocaine 25 mg/g. It has a 30–second onset and 20–minute duration, and is FDA approved for scaling and root planing procedures. The thermosetting property keeps Oraqix in place for effective absorption. Local anesthesia is specifically confined to the periodontal tissues, without residual numbness of lips and tongue. Oraqix is often erroneously classified as a topical agent, when in fact, it is a local anesthetic delivered subgingivally.11 The Oraqix Web site has professional and patient portals.11
One study suggested that a somewhat less profound anesthesia was achieved with the gel (Oraqix), but that it was preferred by patients because of the low incidence of postprocedure problems as compared to conventional injection anesthesia.12 We know that most patients like the anesthesia while in the office, but do not like the prolonged effects, especially of mandibular blocks. The majority of patients (60%) who preferred the gel were also willing to pay for it! We have also experienced this issue in an office, when patients like the concept of a product or procedure, but are unwilling to pay out–of–pocket if insurance does not cover it.
Another study showed favorable anesthetic efficacy of active gel over placebo in selected pain–sensitive patients, suggesting that the gel may be a valuable alternative to conventional injection anesthesia.13 I trust we have all had the experience of sensitive patients who were unwilling to receive traditional local anesthesia, as they were fearful of the injection. So now, rather than patient and clinician both being stressed, we have a viable option to treat these individuals. In fact, September 2004 was the month Oraqix was introduced to the dental hygiene and dental communities, and will celebrate its five–year anniversary this year!
Oraqix is very easy to deliver, and its use is permitted by dental hygienists in most states. Dental hygienists are legally able to administer local anesthesia in 44 states, with Maryland being the newest state to enter the fold.14 Washington State started the ball rolling in 1971, with New Mexico, Missouri, Oregon, Idaho, Arizona, California, and Colorado all following suit in the 1970s.
Technique for delivery
For an animation video, visit the Web site.15 Oraqix is applied to the gingival margin around the selected teeth using the blunt–tipped applicator included in the package. The operator waits for 30 seconds, and then fills the periodontal pockets with Oraqix using the blunt–tipped applicator until the gel becomes visible at the gingival margin. The clinician waits another 30 seconds before beginning treatment. A longer waiting time does not enhance the effect of the anesthesia. Anesthesia, as assessed by probing of pocket depths, has a duration of about 20 minutes, with an average individual overall range of 14 to 31 minutes.16 It should not be injected or used on patients with a sensitivity to the amide type of local anesthetics or any other component of the product.17
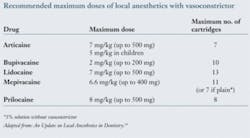
Oraqix may be reapplied if needed. The maximum recommended dose of Oraqix at one treatment session is five cartridges. Remember to use the weight of the patient as a guide, and count any traditional local anesthetics carpules that may be administered at the same time for other procedures. The maximum dose for local anesthetic solutions is about 70 mg to 500 mg for an average 70 kg (154 lb.) patient. The maximum dose depends upon the age, weight, and health of the patient, the type of solution used, and the presence of a vasoconstrictor in the solution.
When administered, Oraqix should be a liquid. If it has formed a gel, it is too warm and should be placed in a refrigerator (do not freeze) until it becomes a liquid again.
We all strive to deliver the best care in the safest possible manner. Patient centered, evidenced–based care (EBC) is an ideal to which we should all strive, remembering that EBC takes into account the scientific evidence, experience and judgment of the clinician, the clinical circumstances, and importantly, patient preferences. Local anesthetics are safe, efficacious, and provide patient comfort. Which drug to choose should be based on the estimated duration of action required, the patient's medical history, and possible drug interactions. Local anesthetic solutions without vasoconstrictor may be selected for short procedures where vasoconstriction is less important. Mepivacaine and prilocaine plain are injectable choices, and Oraqix is a noninjectable option. They may also be used when epinephrine should be avoided, as in patients with severe ischemic heart disease or recent myocardial infarction. “Happiness is your dentist telling you it won't hurt and then having him catch his hand in the drill.” — Johnny Carson
References
- Pirok DJ, Finley JM, Galiene RL, Kokos R, Parey M, Page D, Opdahl JH, and VanBladel TJ. The evolution of pain control in dentistry. Journal of the American Dental Society of Anesthesiology, May 1964; 156–180.
- Fillebrown T. A textbook of operative dentistry. Philadelphia, P. Blakiston, Son & Co., 1889.
- Schulein TM. Journal of the History of Dentistry, July 2005; 53(2):69.
- http://www.thefreedictionary.com/Local+anesthetic
- http://www.novalar.com/
- Hersh EV, Moore PA, Papas AS, et al. Reversal of soft–tissue local anesthesia with phentolamine mesylate in adolescents and adults. JADA 2008; 139(8):1080–1093.
- http://www.novalar.com/assets/pdf/adult_sci_summary.pdf
- http://www.milestonescientific.com/products_dental.html
- Gibson RS, Allen K, Hutfless S, Beiraghi S. The Wand vs. traditional injection: a comparison of pain–related behaviors. Pediatr Dent. Nov.–Dec. 2000; 22(6):458–62.
- Palm AM, Kirkegaard U, Poulsen S. The Wand vs. traditional injection for mandibular nerve block in children and adolescents: perceived pain and time of onset. Pediatr Dent. 2004; 26:481–484.
- http://www.oraqix.com/default.aspx?pageid=1
- van Steenberghe D, Bercy P, De Boever J, Adriaens P, Geers L, Hendrickx E, Adriaenssen C, Rompen E, Malmenäs M, Ramsberg J. Patient evaluation of a novel noninjectable anesthetic gel: a multicenter crossover study comparing the gel to infiltration anesthesia during scaling and root planing. J Periodontol 2004; 75:1471–1478.
- Magnusson I, Geurs NC, Harris PA, Hefti AF, Mariotti AJ, Mauriello SM, Soler L, Offenbacher S. Intrapocket anesthesia for scaling and root planing in pain–sensitive patients. J Periodontol 2003; 74:597–602.
- Local Anesthesia Administration by Dental Hygienists State Chart. ADHA, 2009.
- http://www.oraqix.com/default.aspx?pageid=69
- Friskopp J, Nilsson M , Isacsson G. The anesthetic onset and duration of a new lidocaine/prilocaine gel intra–pocket anesthetic Oraqix®. Journal of Clinical Periodontology 2001; 28(5):453–458(6).
- http://www.oraqix.com/assets/oraqix/oraqix_pi.pdf
- Haas DA. An update on local anesthetics in dentistry. Journal of the Canadian Dental Association, Oct. 2002; 68(9):548.
- Sackett DL, Rosenberg MC, Gray JA, Haynes RB, Richardson WS. Evidence–based medicine: what it is and what it isn't. BMJ, 1996; 312:71–72.
About the Author
Maria Perno Goldie, RDH, BA, MS , is a professional member of the National Speakers Association and president elect of the International Federation of Dental Hygienists. As a noted researcher, author, and speaker, she has presented seminars nationally and internationally on topics such as Women's Health and Wellness, Oral Care for the Cancer Patient, Oral Cancer, and Immunology and Periodontal Disease. Maria is visiting faculty at the University of Rome for the Interdisciplinary Master's Degree Program in Advanced Technologies in the Sciences of Oral Hygiene. Maria was the 1997–1998 president of the American Dental Hygienists' Association.