Ultrasonics & Ergonomics
The green approach to instrumentation
by Anne Nugent Guignon, RDH, MPH
Four decades ago, ultrasonic instrumentation was in its infancy. No one considered the long-range impact of workplace safety issues with this equipment. Many hygienists embraced the advances in ultrasonic technologies and released their fear of relying on hand scaling as the gold standard. They are enjoying the ergonomic benefits of power scaling while delivering quality care.
Today's ultrasonic scalers are mainstream and considered by many to be the standard of care in clinical dental hygiene, supplemented by hand instrumentation as the need arises. As with any technology change, a corresponding change must be made to ensure that the tool or task is adapted to the user rather than the user compromising work postures to use the tool or technology.
With the advent of more sophisticated machines, tip designs, and emerging research about plaque biofilm, ultrasonic scalers are rapidly becoming the primary instrument of choice for today's clinicians. Some will always prefer hand scaling, but a growing number of clinicians are using power scalers every day — often on every patient, unless there is a specific contraindication. There is a variety of things to consider that make ultrasonic scalers effective and a joy to use with minimal stress on our bodies.
Ultrasonic scaling is not a one-size-fits-all, point-and-shoot technology. Rather, it's a sophisticated methodology that allows clinicians to efficiently disrupt and remove hard deposits, surface stains, and plaque biofilm.
Anytime a tool is used over and over, a risk exists for repetitive stress injuries; however, it is possible to use ultrasonic scalers in a manner that is safe for both clinicians and patients. The basic principle of ergonomics is to have the tool or task adapt to the user, not have the user adjust his or her body to accommodate the situation or equipment.
Our goal in scaling is to disrupt plaque biofilm and remove hard deposits and stain, reducing the overall microbial load to a level that a patient's own immune system can create a positive healing response. This must be done with the least amount of damage to natural tooth surfaces and restorative materials. Despite our loftiest goals, we'll never be able to remove every microbe from every tooth surface, but quality instrumentation with today's ultrasonic scalers is critical to help us achieve outstanding clinical outcomes.
The three types of power scaling technologies are sonic, magnetostrictive, and piezoelectric. Sonic devices can remove hard deposits and stain but do not produce cavitation, a function critical to the disruption of complex biofilm communities. The other two technologies are classified as ultrasonic devices that generate vibrations that create deposit and biofilm disruption via sound wave energy and tip movement.
Magnetostrictive vs. piezoelectric ultrasonic scalers
While it is possible to achieve excellent clinical debridement with both types of technology, there are significant differences in how these two types of scalers operate, much like the differences between gasoline-powered combustion engines and those operating with diesel fuel. The tips on magnetostrictive scalers move in an elliptical, figure-eight pattern. While there are varying power levels on different tip surfaces, it is relatively easy to adapt the side of a magnetostrictive scaler tip to a variety of tooth surfaces.
Piezo technology features a linear tip movement, so the most ideal scaling is done with the lateral surfaces of the insert tip. This technique produces the smoothest vibration pattern, similar to erasing marks off a chalkboard but can require more wrist movement for adequate adaptation.
• Tip selection and installation — Tip selection is a critical component of ultrasonic scaling. Even at low settings, a large diameter tip produces more powerful vibrations than one of the newer ultra-slim tips. Studies indicate that heavy vibration over prolonged periods of time is a risk factor for a workplace musculoskeletal disorder; however, the slimmer tips, used on low settings, reduce vibration.
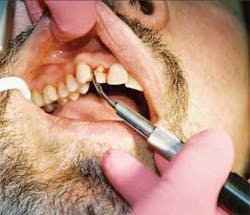
A number of tips designs are available for both technologies. Universal tip designs range from robust to ultra-thin, which are used for microultrasonic scaling procedures. Right and left configurations are perfect for accessing furcations (see Figure 1), deep interproximal defects, malpositioned teeth, and working around orthodontic appliances. One of the best ergonomic benefits that right and left inserts offer is the ability to maintain a neutral wrist position when scaling lingual surfaces of the lower anterior teeth that are in lingual version.
Magnetostrictive inserts slip easily in and out of the handpiece, presenting little ergonomic challenge in installation. Piezo tips are short and screw into the unit handpiece and require a final tightening with a special wrench. Initial installation of a small tip in the handpiece can be challenging for clinicians with a compromised pinch grip. Typically, the tips are small and easy to lose, and there is a potential for a puncture wound when tightening with a traditional wrench.
Both the Hu-Friedy Symmetry IQ and the EMS Piezon Master units offer piezo tips that are housed in a unique tip/wrench system. These special torque-limiting wrenches are easy to grip and make it easy to both install and remove small tips. The design also eliminates the potential for puncture and prevents over tightening.
• Handpiece features — The size, weight, diameter, balance, and surface texture of the handpiece — as well as cord torque — each play a critical role in creating a safe ergonomic power scaling experience.
Everyone's hands are a different size. So what fits one clinician may well not be optimal for another.
Magnetostrictive handpieces are generally long, with a uniform diameter and little to no surface texture. 25K machines have longer handpieces than 30K units and feel more balanced to most clinicians because the weight is distributed over a longer length. Piezo handpieces are shorter and chunkier than magnetostrictive, with most being shaped like our wide body polishing handpieces. The shape is necessary to accommodate the active components housed in the handpiece. Typically, piezo handpieces feature textured surfaces, which facilitate a light grasp, especially in moist environments.
• Surface texture, padding, and grips — The first magnetostrictive inserts were all metal. Those who work with manually tuned units typically favor all-metal inserts because of the smooth vibration patterns.
In recent years, companies have focused on developing inserts and handpieces that have larger diameter, textured, medical-grade silicone autoclavable gripping surfaces. Texture equals traction and silicone padding improves comfort. Texture, padding, and larger grip diameters reduce pinch grip and hand fatigue. Color-coded silicone grips, like Riso's Soft Dental Grips or Practicon's Chub-Eze grips can also be added to existing magnetostrictive inserts to achieve these goals.
• Reducing cord torque — Cord torque is an ongoing problem in many older or more inexpensive units. Bulky cords that do not bend or flex easily create undue stress on a clinician's hands, forearms, and shoulders. Clinicians should not have to fight a heavy, resistant cord just to scale a tooth.
There are several solutions to this annoying problem. Dentsply Cavitron SPS units feature the SteriMate handpiece that has a hose-end swivel. Some older models can be retrofitted with this handpiece. A decade ago, Hu-Friedy introduced the first magnetostrictive insert that featured a fingertip swivel. Discus Dental's new Insight insert has this feature as well. Some units such as the USI 25 MPLC, Hu-Friedy's Symmetry IQ and the NSK Varios are made with long, flexible cords that have low cord torque.
If a unit with a lightweight hose or swiveling handpiece is not available, it is still possible to redistribute the weight of the hose and handpiece. A looped portion of the hose can be held between the pinkie and ring finger, wrapped around the forearm (see Figure 2), held in the palm of the hand, looped around a clinician's neck, or threaded over the overhead light handle. Some even use a vertical metal ironing board cord holder to redistribute the hose weight (see Figure 3).
• Unit size, location, and easy access to controls — It is critical that the unit be placed on a countertop or tray that is easy to reach in order to make minor adjustments in power, frequency, or water. This is especially important when using more than one type of tip during the appointment. Avoid putting the machine behind the clinician or locations that involve bending, twisting, or leaning your torso to access the controls or change tips or inserts.
The footprint of units varies considerably between technologies and manufacturers. While a petite unit may appear very attractive, consider that the controls may be hard to activate or adjust. Petite dials and switches are harder to disinfect or cover with a barrier than larger knobs or flat touch pads. Loosely fitting barriers interfere with pinch grip and reduce the ability to manipulate a switch or knob, and those that tightly adhere to the control surface can restrict free movement of controls.
Some equipment manufacturers design multipurpose dental units that incorporate an ultrasonic scaler. An all-in-one unit may seem attractive, theoretically reducing the scaler's cost; however, this type of bundling creates potential problems that may crop up at future dates. If repairs are ever needed, the scaler will have to be removed from the unit, often requiring the services of a dental repair specialist. Built-in units with short handpiece hoses create strain on the clinician's wrist, hand, forearm, and shoulder. Built-in units eliminate a clinician's personal preference for where the unit is positioned during the procedure — a factor that may come into play when both right- and left-handed users are expected to use the same equipment.
• Foot switches — Most foot switches are small, corded, on/off, foot-activated devices that require clinicians to maintain constant contact to keep the tip vibrating. Continuous contact over a prolonged period of time can lead to static body postures. A number of manufacturers now provide multifunction foot switches that control basic power and boost functions, as well as lighting and irrigation. Both manually tuned magnetostrictive and the piezoelectric devices are made that have true “cruise control” foot switches that, once activated, continue to scale without the clinician maintaining continuous contact with the device. Dentsply's cordless foot control allows each clinician to determine the ideal position.
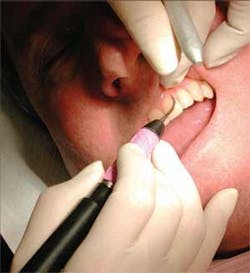
• Activating and adapting the insert — Today's ultrasonic scalers are effective tools in biofilm disruption, as well as removal of both soft and hard deposits. As with any other tool, specific techniques will enhance procedural effectiveness while limiting ergonomic stress. Grasp the handpiece so it is evenly balanced in the web of the hand between the thumb and index finger. Holding the handpiece with a light pen grasp enhances tactile sensitivity, making it much easier to detect small subgingival deposits (see Figure 4). Support the handpiece with a probelike grasp. A light grasp also reduces hand fatigue and facilitates gentle rotation of the handpiece to accommodate challenging tooth surfaces.
Think of power scaling as a probe with power — the power to destroy the enemy. It is not necessary to apply a heavy hand or use brute force. Keep the side of the tip adapted to the tooth in a parallel manner. Gentle, overlapping strokes will remove deposits and imbedded organisms. The key is spending enough time. One swipe through the sulcus probably won't be enough, even in a patient who only needs biofilm debridement.
It takes time and patience to disrupt debris. Remember, the fluid irrigant not only flushes and creates washed field visibility; it also has a bactericidal function because of cavitation and acoustic microstreaming. The end point is reached when there are no more clinically detectable deposits and the fluid irrigant flushing out the pocket is clear and free of visible debris.
• Fulcrum alternatives and patient positioning — Traditional hand instrument fulcrums are not recommended for ultrasonic scaling. Most clinicians utilize a combination of different extraoral fulcrums. Some of the more popular fulcrums include a soft tissue rest on the cheek or chin while using a single-finger pinky fulcrum or a multifinger rest. A light pen grasp is essential for an extraoral fulcrum. This type of grasp can be applied to polishing procedures as well.
Patient positioning is critical as well. Fluid evacuation is a constant challenge when using ultrasonics. When working in a 9 to 11 o'clock, or a 1 to 3 o'clock position, elevate the back of the patient chair 30 to 45 degrees so the patient's head is higher than their knees (see Figure 5). Rather than have the fluid irrigant run down the back of their throat, have the patient turn toward you so the fluid can be quickly suctioned from the buccal vestibule. While a 12 o'clock position, with a patient fully reclined, improves access to the lower anterior teeth, fluid evacuation can be an issue.
Some clinicians hesitate to ask patients to reposition their heads during an appointment, but it is critical to remember that they are in the dental chair for a short period of time. On the other hand, clinicians spend hours every day in compromised postures. Neck pillows provide comfort for patients who have chronic neck problems. A small pillow placed between the base of the neck and shoulder blades makes it easier to access the oral cavity when working on large patients.
Once reclined, ask your patient to scoot to the top of the chair to improve access. To keep your wrist and forearms in a neutral posture, position the chair height so the working field is waist high.
Clinician seating is another critical component in creating a safe ergonomic environment. Ideally, the size, shape, and height of the clinical stool should fit the user. Chairs with adjustable arms and lumbar supports, saddle chairs, and ball chairs are designed to provide optimal upper body support (see Figure 6).
• Controlling fluid irrigation and suction — Being able to see the clinical field clearly is another key to successful and comfortable ultrasonic scaling. Three factors come into play that ensure optimal visibility. Controlling fluid irrigant spray and washed field visibility are critical (see Figure 7). Fluid irrigants cool magnetostrictive tips, but creating microscopic fluid cavitation is the most important contribution. Ideally, clinicians should control the irrigation so a steady, heavy drip with a light mist surrounds the activated tip. Heavier sprays obscure the working field. The Dentsply SteriMate has a fluid flow control built in to the handpiece.
Hands-free suction devices are the most ideal ergonomic solution. Hygoformic saliva ejectors and Otis Formeject saliva ejectors with an ergonomic bend keep the field free of excess fluid. The Blue Boa suction extension is a lightweight, autoclavable device that attaches to the high volume suction (see Figure 8). Several different designs and lengths are available that can accommodate either a small or standard diameter saliva ejector.
Mirror suction devices can do double duty during scaling, but it is important to look for lightweight products that have clear mirror surfaces. A combination mirror suction device that features a swivel coupling is currently under development. This new device virtually eliminates stress on the wrist. The Isolite suction system combines the benefits of focused source illumination, suction, and functions as a mouth prop.
• Mouth mirror magic — Mouth mirrors are a basic form of illumination. It is important to keep the surfaces fog-free and reduce droplet formation that interferes with illumination and visualization. A variety of products will do the trick, but most mouthwashes work just as well. Wipe the surface with a mouthwash-dampened 2x2, spray the surface, or dip it into the liquid. The surface tension of the mouthwash causes fluid to sheet across the surface and prevents fogging. Several applications may be necessary during scaling.
The type of mirror is also important. Double-sided mirrors aid in both tongue-and-cheek retraction while providing enhanced imaging with less contortion. Zirc's Crystal Mirror is made with a unique surface that reflects more light and truer colors than a standard rhodium mirror.
Several companies offer lighted mirrors with varying degrees of illumination. LED models feature clean, white light that can be directed anywhere in the oral cavity. Devices such as Young Dental's foil-coated Dri-Aids also reflect light during scaling.
Scratched mirrors reduce visibility. Replace mirrors that are worn out. Consider using a mirror protector such as the Mirror Gear silicone covers to extend the working life of your mirrors. The colorful, flexible covers are designed to protect mirror surfaces during instrument cleaning procedures, sterilizing, and storage (see Figure 9).
• Enhancing visual acuity — It is well known that adequate, shadow-free lighting reduces fatigue and stress. In addition to headlights, there are inserts that contain small LED lights, handpieces that are fabricated with fiber-optic lighting, and miniature lights that clip directly on to the ultrasonic scaling handpiece. The intensity and color of the illumination varies per device, and strides are being made every day to improve the illumination output of these devices.
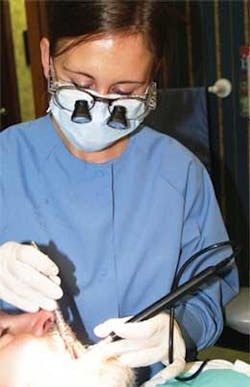
The ultimate visual acuity enhancement comes with using some form of magnification and auxiliary lighting. Surgical microscopes provide an amazing view for any clinical procedure. However, the most widely used enhancements are magnification loupes and auxiliary headlights. All of these devices improve visual acuity and, if properly fitted, aid in nonstressful clinical postures while enhancing the clinical outcomes from ultrasonic scaling.
Remember to keep the overhead light lens clean to maximize light output. Dust and smudges are disconcerting to patients, cut down on light, and are easy to remedy. Just like mouth mirrors or face shields, plastic lens covers on overhead lights scratch over time. A replacement lens cover is an inexpensive way to improve the amount of light.
Facemasks and shields fit into the ergonomics of ultrasonics, especially when using magnification loupes. Certain brands of facemasks are designed to reduce or eliminate fogging. Consider using a mask that helps support the weight of loupes on the nose. Keep the face shield clean and replace scratched shields. Consider using one that attaches directly to the temples of your loupes to ensure a more custom fit.
• Hearing protection — Recent studies now indicate hearing loss can occur from prolonged, frequent exposure to lower level noise, rather than being limited to sounds exceeding 90 decibels. A growing number of clinicians now use hearing protection while performing noisy procedures.
• Data collection — With the information explosion and the increasing numbers of medically complex patients, accurate data collection and record keeping are the foundation for quality patient care. Document, document, document is the mantra. A number of excellent products facilitate initial data collection or aid in ongoing patient re-evaluation, and many facilitate our goal to practice more efficiently and safely.
Developing and maintaining accurate records of the oral cavity is tedious and time consuming — and fraught with misinterpretations if recorded by hand or without help. Both the Dental RAT, a foot-activated mouse that interfaces with most charting software (see Figure 10), and PerioPal, a voice-activated charting system, fulfill sound ergonomic principles.
On a more basic level, it is easier to visualize probing depths using a probe made with contrasting color segments like yellow and black, or red, white, and green. Automated probes such as the Florida Probe ensure consistent calibrated recordings. The newest product designed to facilitate data collection is Orascoptic's lighted perio probe. A small, disposable, fiber-optic strand extends neatly from a thin metal housing. The probe marks are quite easy to see when the device is illuminated and the white light provides a limited amount of illumination in the surrounding area.
Keeping patients comfortable
Anxious, tense patients create enormous ergonomic challenges. It's nearly impossible to work on a patient with a rigid body posture or who can't or won't position their head for easy access. Unless a patient has some type of physical disability, fear is usually the basis of their apprehension. If you can determine the root cause, then it is easy to create an environment that will defuse their anxiety.
The physical environment needs to be calm and comfortable. Earplugs, comfortable neck pillows, blankets, chair massagers, soothing music, and soft lighting melt tension. Some patients worry about pain or gagging. Others have had less than ideal experiences with ultrasonics — a problem that generally stems from teeth that are sensitive to cold, air, or touch. There are great ways to resolve each issue. A locally applied anesthetic such as Oraqix helps many overcome their fear. Frequent pauses for fluid evacuation are appropriate for those worried about gagging.
Many new products can be applied preprocedurally to eliminate dentinal hypersensitivity. Two of the most effective are Colgate's Sensitive Pro Relief desensitizing paste that contains the arginine/bicarbonate complex called ProArgin, and Dentsply's NuSolutions prophy paste that contains NovaMin. In most cases, patients achieve immediate relief from these products due to tubule occlusion.
Ultrasonic scaling is not a one-size-fits-all, point-and-shoot technology, but rather a sophisticated methodology that allows clinicians to efficiently disrupt and remove hard deposits, surface stains, and plaque biofilm. The green concept is based on conserving natural resources. Preventing needless workplace cumulative trauma disorders and preserving the health of the clinician while delivering quality care through ultrasonic scaling are perfect examples of how dental hygiene practice can join the green movement.
About the Author
Anne Nugent Guignon, RDH, MPH, is the senior consulting editor for RDH magazine. She is an international speaker who has published numerous articles and authored several textbook chapters. Her popular programs include ergonomics, patient comfort, burnout, and advanced diagnostics and therapeutics. Recipient of the 2004 Mentor of the Year Award and the 2009 ADHA Colgate Irene Newman Award, Anne is an ADHA member and has practiced clinical dental hygiene in Houston since 1971. You can reach her at [email protected] or (832) 971-4540, and her Web site is www.anneguignon.com.