by Nancy W. Burkhart, RDH, EdD
[email protected]
Your patient is Henry, who is a 15-year-old male and has been in your practice for several years. Henry presents with noticeable, coalescing ulcerations appearing clinically as multiple, aphthous ulcers created by granulomatous tissue enlargement in the soft tissue folds.
Figure 1: Photo depicts an unusual ulcer appearing within the soft tissue folds. Courtesy of Dr. Hiroyashu Endo.
Henry complains that this is an ongoing problem. He says sometimes various areas of his mouth are affected, including his tongue and the floor of the mouth. He tells you that the ulcers are often very deep and quite large. As you examine the tissue, you also notice some scarring from previous lesions. Henry is later diagnosed with Crohn’s disease (see Figure 1).
Etiology: Reported in 1932, Crohn’s disease is described as a chronic, idiopathic granulomatous inflammatory disease. The true etiology of Crohn’s disease is unknown, but it is probably genetically and immunologically mediated.
For many years, a relationship between Crohn’s disease and vitamin D deficiency has been noted, but it is unclear whether the vitamin deficiency is an etiologic factor or occurs secondary to the altered nutrition associated with the disease. However, a recent research study suggests that vitamin D deficiency may play a contributory role at the molecular level in development of the disease (Wang et al. 2010).
A genetic propensity to Crohn’s disease has been reported in approximately 10 to 20% of those affected.
Crohn’s lesions are found in the gastrointestinal tract, presenting as abscesses and noncaseating epithelioid-type granulomas, which may occur at localized sites throughout the entire GI tract from the mouth to the anus, affecting the lining of all involved areas. Obstruction and abscess formation in the intestinal wall is common in long-term Crohn’s disease, and an increased risk of colon cancer has been reported in chronic Crohn’s disease.
Symptoms such as nausea, diarrhea, vague or acute pain, and cramping are routinely reported. When symptoms are prolonged, anemia can occur due to internal bleeding, and the patient may suffer from severe weight loss. Vitamins B and D, folic acid, iron, and other nutrients are poorly absorbed because of the inflammatory process. Anemia may be a detectable indication of Crohn’s disease.
In the head and neck region, granulomatous diseases are often classified using a broad term of orofacial granulomatosis (Wisenfield et al. 1985), because similar lesions may result from a diverse group of granulomatous diseases that may induce noninfectious granulomatous disorders of the face, lips, and oral cavity. These include Melkersson-Rosenthal syndrome, oral tuberculosis, cheilitis granulomatosa, sarcoidosis, or even contact allergic reactions.
Determining the exact diagnosis obviously may require multiple tests. Yet even using these tests, the final diagnosis is often made by excluding other conditions. The diagnosis of oral Crohn’s disease is sometimes difficult because oral lesions may precede lesions in more typical sites of the GI tract. Final diagnosis of Crohn’s disease usually requires GI tract biopsy confirmation. Specific tests are used to diagnose tuberculosis and sarcoidosis. It is unclear if orofacial granulomatosis is a separate entity or merely an early presentation of sarcoidosis or Crohn’s disease.
Perioral and intraoral characteristics: Poor vitamin absorption and synthesis may result in papillae atrophy of the tongue, mild fissuring of the tongue, and oral tissue changes with an oral effect described as cobblestoning. Large aphthouslike ulcers may be a problem for patients (they are also prevalent in the general population) as well as coalescing, ulcerative lesions usually in the vestibular folds of oral tissue as shown in Figure 1.Figure 2: The slide depicts pyostomatitis vegetans. The patient, a 21-year-old female, was diagnosed with ulcerative colitis several years prior to presentation in the clinic. Courtesy of the Baylor College of Dentistry Stomatology Center.
Pyostomatitis vegetans (see Figure 2) is associated with ulcerative colitis and Crohn’s disease and may indicate exacerbation of the gut lesions. The lesions are usually painless, vegetative folds of tissue containing micro-abscesses. The lesions are most often reported on the facial gingiva, as well as the labial and buccal mucosa. The presence of the lesions should alert the clinician that further evaluation is needed regarding the current state of intestinal problems associated with the possibility of Crohn’s disease.
The lips may be affected with ulcerations and swelling that extend well beyond the wet line of the lips (see Figure 3). The facial and oral characteristics of Crohn’s disease are within a wide array of idiopathic granulomatous diseases of the oral cavity, the lips, and the perioral areas of the face.
Extraoral characteristics: The skin, eyes, and joints have also been identified with changes related to Crohn’s disease. Often, the oral sites are affected before the intestinal tract. Youths are affected more frequently, especially teenagers. Subtle, less dramatic symptoms with vague, persistent complaints may often go undiagnosed for many years, even into adulthood.
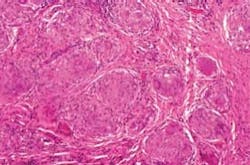
Histology: Classically, Crohn’s disease exhibits a non-necrotizing granulomatous inflammation. Histologically, the granulomas are noncaseating epithelioid type and multinucleated Langerhans giant cells may be found within the oral mucosa. On other areas, ulceration may be evident, as well as the micro-abscesses of pyostomatitis vegetans. The detected inflammation will vary from patient to patient. Specific tests are conducted to rule out other disease states (see Figure 4).
Figure 4: The photomicrograph depicts the histology of Crohn’s disease, showing noncaseating epithelioid granulomas. Courtesy of Dr. John Wright.
Treatment and prognosis: The identification of a specific disease is crucial, differentiating it from other disease states when orofacial granulomatosis is present. Historically, the oral sites are often affected before the intestinal tract, and dentists and hygienists may be the first health-care providers to notice the changes in oral tissues, since the patient usually presents twice a year to a dental office. In addition, there is some evidence to indicate that the appearance of oral lesions in individuals with established Crohn’s disease may indicate a flaring of the other GI lesions. Often, oral lesions do not respond well to treatment until the other GI lesions have been controlled.
Referral to the patient’s physician is always needed, and treatment will vary according to the severity of the disease state. Corticosteroids applied topically provide some relief for the patient. Vitamin deficiency will be treated with supplementation and nutritional counseling. Segments of the bowel may need to be removed in severe cases.
Immune system mediator analysis may be a part of general treatment. Large, aphthouslike ulcerations are common, especially in the oral vestibule and at the base of tissue folds. Topical corticosteroids are often needed as well as intralesional injections of corticosteroids.
Discussion: Medical diagnosis and management of Crohn’s disease is required. However, careful observation of patients in the dental office may lead to diagnosis and may alert the physician of a possible flare of the condition. Remember that, to date, there is no known permanent cure for the condition, so occasional exacerbations should be expected. It is also important to realize that Crohn’s disease and other bowel disorders such as ulcerative colitis can lead to nutritional deficiencies. The dental health-care provider should remain alert for overt oral signs of nutritional deficiency, such as loss of tongue papillae and pale oral tissues.
Early recognition and treatment of all diseases is crucial in the total health and well-being of our patients. Keep listening to your patients and continue to always ask good questions!
References
Delong L, Burkhart NW. General and Oral Pathology, Lippincott, Williams & Wilkins, Baltimore, 2008.
El-Hakim M, Chauvin P. Orofacial granulomatosis presenting as persisitent lip swelling: review of six new cases. J Oral Max Surg., 62:9; 2004 114-117.
Grave B, McCullough M, Wiesenfeld D. Orofacial granulomatosis. Oral Diseases 15, 2009 46-51.
Rees TD. Orofacial granulomatosis and related conditions. Periodontology 2000. 21;1999. 145-147.
Regizi J, Sciubba J, Jordan R. Oral pathology: clinical pathologic correlations. 4th ed. St. Louis: W.B. Saunders, 2003.
Wang TT, Dabbas B, Laperriere D, Bitton AJ, Soualhine H, Tavera-Mendoza LE, Dionne S, Bitton A, Seidman EG, Behr MA, White JH. Direct and indirect induction by 1,25-dihydroxyvitamin D3 of the NOD2/CARD15-defensin beta 2 innate immune pathway defective in Crohn’s disease” Journal of Biological Chemistry Volume 285, Pages 2227-2231, doi: 10.1074/jbc.C109.071225: 2010.
Nancy W. Burkhart, BSDH, EdD, is an adjunct associate professor in the department of periodontics, Baylor College of Dentistry and the Texas A & M Health Science Center, Dallas. Dr. Burkhart is founder and co-host of the International Oral Lichen Planus Support Group http://www.bcd.tamhsc.edu/outreach/lichen/ and coauthor of General and Oral Pathology for the Dental Hygienist. Her Web site for seminars is www.nancywburkhart.com.