Keratoacanthoma
by Nancy W. Burkhart, RDH, EdD
[email protected]
Your patient today is 62-year-old Andy. His appointment is for a prophylaxis and dental exam, having been a patient of record for over 30 years in your practice. Recently retired, Andy had worked for 20 years on several fishing boats out of New Orleans.
Figure 1: Keratoacanthoma of the lower lip. From DeLong and Burkhart, General and Oral Pathology for the Dental Hygienist. Courtesy of Dr. Amy Brooks.
He has been very diligent about getting appointments for dental exams and coming in sooner if there has been a problem with his mouth. However, Andy has not been seen for more than 18 months because of an increase in job duties before retirement. The gulf oil spill added extra work hours and commitments, making it difficult to schedule his dental appointments.
As you examine him, you are most concerned about the lesion on his lower lip (see Figure 1). As you question Andy, you are somewhat relieved when you discover that he has already taken steps to have the lesion evaluated by a dermatologist. Andy reports that the lesion has been present for one year and is asymptomatic. He is scheduled for removal of the lip lesion in a few days.
The final diagnosis was keratoacanthoma (KA).
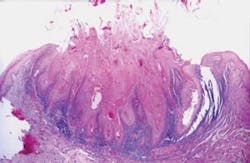
Figure 2: Keratoacanthoma histology. From DeLong and Burkhart, General and Oral Pathology for the Dental Hygienist. Courtesy of Dr. Valerie A. Murrah.
The keratoacanthoma is a benign epithelial proliferation and commonly appears on the vermilion border of the lip. The KA has many common characteristics with the squamous cell carcinoma that is frequently found in the same location. Differentiation is only accomplished through the gold standard of biopsy with histological differentiation. Some pathologists consider the KA to be a subtype of squamous cell carcinoma (Ko, 2010).
Etiology: The keratoacanthoma has several possible etiologies:
- Sunlight exposure. In this case, ultraviolet light is the strongest etiology since Andy is a fisherman and spends a lot of time in the southern part of the United States and fished as his occupation almost daily.
- A compromised immune system is another factor in the development of these lesions. Anytime the immune system is compromised, the person is at an increased risk of opportunistic infections and serious health issues.
- Exposure to HPV with multiple types of the virus being linked to this lesion.
- Exposure to tar and/or pitch.
- The presence of chromosomal abnormalities of the skin.
- Correlated with disturbance of the outer root sheath of the hair follicle, since the KA is often found in areas of the skin with many hair follicles.
Epidemiology: Keratoacanthomas are rare in younger individuals under 20 years of age and those with dark skin. The lesion is usually found in an older population of over 60 years of age. Males have a higher incidence than females. However, clinical documentation of both females and those in a younger age group are reported in the literature (Ramos et al. 2009).
Pathogenesis: The lesions are associated with the sebaceous glands and hair follicles. The size will vary with a 1-2 cm span and tend to increase in size with time. KAs over 2 cm are classified as giant keratoacanthomas. KA is also found in the Ferguson-Smith syndrome in which a patient may have several lesions or as many as 100 in number. KAs are also found in Grzybowski syndrome, Witten-Zak syndrome, and Muir-Torre syndrome. The histological features, size, and clinical appearance vary with each type.
Extraoral characteristics: As depicted in the slide presented, the lesion is usually sessile with a dome shape. The loss of the vermilion border is evident in the slide presented and probably due to excessive sun exposure. The lips present with a pink, stretched appearance and loss of definition.
A core plug of keratin is evident in the center of the lesion within the central crater.
Perioral and intraoral characteristics: The keratoacanthoma is found on the lower lip, but also in areas with hair follicles or extremities in other external surfaces. Although the KA is usually a solitary lesion, it may be multiple in some cases.
Distinguishing characteristics: The lower lip is also a prime location for squamous cell carcinoma (SCC). Removal of the KA and a biopsy are needed to differentiate between the two lesions. The core, central keratin plug is a distinguishing characteristic.
Significant microscopic characteristics: As depicted in Figure 2, the keratoacanthoma is cup-shaped with central keratin and inflammatory cells. Most cases of KA are diagnosed with clear features; but some can be challenging for the oral pathologist with unclear, conflicting features that resemble SCC.
Dental implications: Patients with keratoacanthoma are at an increased risk of melanoma and should guard against sun damage to the skin. The higher SPF sunblocks should be used as well as a lip balm with SPF sun protection. Small kerataocanthomas may be missed in early stages. The extraoral exam with palpation and notation of the head and neck is especially important.
Treatment and prognosis: Complete surgical removal is necessary for a pathological diagnosis. The prognosis is excellent for the keratoacanthoma with complete removal through biopsy. Scar tissue is usually a common complaint because of the size and amount of tissue that needs removal for complete excision.
References:
DeLong L, Burkhart N. General and Oral Pathology for the Dental Hygienist. Lippincott, Williams & Wilkins. Baltimore. 2008.
Ko CJ. Keratoacanthoma: facts and controversies. Clin Dermatol. 2010 May-June; 28(3):254-61.
Ramos LM, Cardoso SV, Loyola AM, Rocha MA, Durighetto-Junior AF. Keratoacanthoma of the inferior lip: review and report of case with spontaneous regression. J Appl Oral Sci 2009 May-June; 17(3): 262-5.
Nancy W. Burkhart, BSDH, EdD, is an adjunct associate professor in the department of periodontics, Baylor College of Dentistry and the Texas A & M Health Science Center, Dallas. Dr. Burkhart is founder and co-host of the International Oral Lichen Planus Support Group (http://bcdwp.web.tamhsc.edu/iolpdallas/) and co-author of General and Oral Pathology for the Dental Hygienist. Her Web site for seminars is www.nancywburkhart.com.
Past RDH Issues