How hygienists can influence the odds of success
by Ann-Marie C. DePalma, RDH, MEd, FADIA, FAADH
Dental implants have changed the landscape of dentistry for many patients. Patients previously would suffer with edentulous areas that could not be restored and endure the consequences of lack of function, esthetics, speech, and health that these edentulous areas caused. Over the last few decades, implant dentistry has grown to be a $1.5 million business in the United States alone. Implants have enhanced the lives of so many patients. Hygienists play an important role in the education of patients regarding implants, initially proposing treatments, discussing surgical and prosthetic options, and providing professional maintenance care while instructing patients on home care options. Are you maintaining your education regarding the rapidly evolving implant landscape?
Dental implants are considered standard of care in dentistry for any edentulous area. All patients should be offered the options of implants for edentulous areas; however, not all patients are true candidates. Thorough medical and dental histories need to be completed on all possible candidates with special emphasis on systemic concerns. Patients with uncontrolled diabetes, smokers, alcoholics, and patients with compromised immune systems need special consideration when discussing implants. These patients may not be ideal candidates, but depending on specific circumstances, implants can be placed with proper education and protocols. However, the success rate of implants placed in patients with these conditions is greatly reduced from a general percentage of 95-98% success.
Patients need to understand the implications of systemic factors on the overall viability of the implant. Additionally, anatomical considerations such as location of the mandibular canal and sinuses, the amount of available bone surrounding an implant, the amount of interarch distance, and occlusal schemes play critical roles in the success of implants. Implants often fail due to two primary reasons, biomechanical overload and bacterial invasion. The biomechanics involves correct number and placement of implants along with an understanding of the patient’s systemic and occlusal characteristics. As hygienists, our role in implant therapy involves the education of the patient regarding reduction of the bacterial components.
In diagnosing the potential implant area, the dentist will review all available data. This includes radiographs, study models, clinical examinations, intraoral photos, and any other information as deemed appropriate for the specific patient. The gold standard of care for radiographic examination currently is the panoramic radiograph. Periapical films are also essential. With the advent of three-dimensional imaging (cone beam computed tomography, CBCT), radiographic interpretation has taken a leap forward but is not considered the standard of care as the panoramic radiograph is. This may change in the near future.
Surgical care has evolved over the years from placement of implants only in hospital operating room settings to sterile dental operatory placement, and then to “clean” placement in the dental practice. From years of only oral surgeons who placed implants, periodontists, general dentists, prosthodontists, and endodontists are now placing implants. Orthodontists even place temporary anchorage devices (TAD) using mini-implants.
The uses and availability of implants — both traditional and mini — are expanding. Traditional root form implant diameters are 3.75 mm while mini-implant root form diameters range from 1.8 to 2 mm. One can consider any implant diameter less than 3.75 as mini, depending on the manufacturer. Lengths of root form implants also vary depending on the manufacturer’s specifications.
Manufacturer differences can also be seen in the types and amount of coating placed on the titanium surface of the implant. Early implants were pure titanium but these fractured during occlusal stresses; currently implants are comprised of a titanium alloy with varying types of coatings. Coating the surface of the titanium increases surface area for stronger osseointegration.
Surgical considerations have advanced from two-stage flap surgical placement to one-stage surgical flap placement, and then to tissue punch options and to “teeth in a day.” Depending on the patient and practitioner’s needs and philosophy, options vary for surgical placement. Bone grafting and augmentation, along with tissue/blood protein enhancers, have greatly increased implant viability and success.
Prosthetic options have also expanded. Implants can be used to restore a variety of edentulous areas and are classified based on several factors. The types of restorations include:
• FP-1: Fixed prosthesis replaces only the crown and looks like a natural tooth
• FP-2: Fixed prosthesis replaces the crown and a portion of the root; crown contour appears normal in the occlusal half, but is elongated or hypercontoured in the gingival half
• FP-3: Fixed prosthesis replaces missing crowns and gingival color and portion of the edentulous site. Prosthesis most often uses denture teeth and acrylic but may be porcelain and metal
• RP-4: Removable prosthesis and overdenture supported completely by the implants
• RP-5: Removable prosthesis and overdenture supported by both soft tissue and implant.
Screw-retained implants are decreasing in usage, while cemented retained implants are the option of choice for most restorations. Cement-retained prostheses resemble traditional prosthesis and the dental professional needs to be aware of their presence in order to avoid damaging any of the critical implant supporting structures.
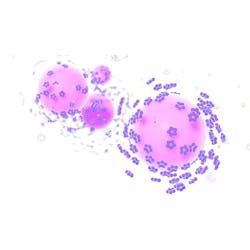
Implants do not have a periodontal ligament, and attachment is provided by circular fibers rather than the fibers found throughout the periodontal ligament structure. Once these fibers are destroyed by bacterial contamination, invasion around the implant occurs more rapidly than around tooth surfaces and can lead to peri-implantitis. Peri-implantitis is the inflammatory process around implants initiated by periodontal pathogens similar to those found in the periodontal disease process. Cement-retained prostheses must also be cleaned of all residual cement to prevent tissue irritation.
The role of the dental hygienist
Hygienists need to understand the importance of professional maintenance of implants. Controversies abound in implant dentistry and the role of maintenance is one of these areas. To probe or not, to use metal or nonmetal instrumentation are areas of concern for the hygienist in treating implant patients.
It is the opinion of this author that conservative therapy should be followed. Older style implants sat above the gingival margin; therefore, instruments were developed which did not need to go subgingivally. The early scalers for implants were big and bulky, and some practices still use these early instruments.
Today’s implant bodies are buried subgingivally into the bone, and only the abutment and prosthesis are accessible to instrumentation. However, the author’s opinion is since we do not have sufficient research available to determine the exact issues using metal or nonmetal instrumentation, it is better to use nonmetal during the maintenance appointment. Available current research shows that stainless steel, titanium-coated, and other types of implant scalers mar the soft titanium surface. The author believes that implant-friendly materials such as plastic should be used during maintenance. Ultrasonic scalers specifically designed for use on implants can also be used if needed.
Due to the nature and tenacity of calculus around implants, metal instrumentation and ultrasonics are not routinely needed. When the implant structures have been scratched and bacterial contamination increases and the implant begins to fail, then it may be appropriate to use metal instrumentation and ultrasonics.
Probing is appropriate to determine the health of the implant. Initial probing depths should be recorded at the first postprosthetic maintenance appointment. Radiographs should also be taken following prosthetic placement and then yearly as deemed appropriate for the specific patient needs. Radiographs evaluate the mesial/distal areas around implants; thus probing can be done with negative mesial/distal radiographic findings on the buccal/lingual surfaces. Gentle probing pressure should be used in order not to destroy the circular fibers. Chlorhexidine may also be used on the tip of the probe to reduce bacterial contamination during probing. Due to the nature of the prosthesis, parallel placement of the probe may be difficult; the hygienist should try to maintain as parallel positioning as possible.
Observation of soft tissue structures around the implant should also be evaluated similar to observation of tooth tissue structures including color, size, shape, texture, and bleeding/exudate. Plastic probes should be used in order to prevent marring of the implant structures. Hygienists should also evaluate for presence of mobility using a two-handle approach as mobility is evaluated in the natural dentition. Mobility can be caused by a prosthetic complication or a failing implant. Any mobility should be noted.
Implant patient homecare should be evaluated at each visit. Hygienists should be familiar with the verbal skills necessary to individualize, demonstrate and encourage patients to maintain their implants on a daily basis. A variety of products are available for homecare choices and, depending on the hygienist/practice preferences and the patient’s skills, these can be reviewed during the maintenance appointment. Educating patients about specific hygiene routines and the value of regular maintenance is essential in long-term implant success.
Implant dentistry is an essential component of clinical practice. Hygienists need to be constantly seeking education about the current status of all areas of implantology. One such avenue is to become a member of the Association of Dental Implant Auxiliaries. ADIA is a component organization of the International Congress of Oral Implantologists. ICOI/ADIA meet several times each year with programs specifically designed for all members of the dental team. Certification programs for dental hygienists, assistants, implant treatment coordinators, and practice management are held along with varying levels of membership, including Fellowship. ADIA’s goal is to provide high quality, cost-effective education to motivate team members to provide absolute best care for implant patients and make practices increasingly successful. For information on the ADIA: www.adiaonline.org.
Ann-Marie C. DePalma, RDH, MEd, FADIA, FAADH, is a Fellow of the American Academy of Dental Hygiene and the Association of Dental Implant Auxiliaries, as well as a continuous member of ADHA. Ann-Marie is currently a business/clinical advisor for Jameson Management, Inc., a comprehensive coaching firm, and also presents continuing education programs for dental team members on a variety of topics. She is collaborating with several authors on various books for dental hygiene and can be reached at [email protected] or [email protected].
Past RDH Issues