The Noncompliant Patient
Dear Dianne,
I love treating periodontal patients, but occasionally I get someone who refuses to follow through with the homecare regimen that I teach. It is so frustrating! I work very hard to get all the debris off patients’ teeth, but patients seem unwilling to do anything beyond even a cursory brushing. I’ve had a few people who looked as if they never brushed at all between quadrant scaling appointments. People that do not practice good homecare, especially while undergoing periodontal treatment, often continue to exhibit bleeding, which is very discouraging. Do you have any tips to help me improve patient compliance with homecare techniques, which are so vital to success?
Anna, RDH
Dear Anna,
It is beyond comprehension why some able-bodied, capable people take so little interest in keeping their oral cavity clean. I wonder how some people can stand their mouths! There have been times I’ve wanted to get in a patient’s face and say, “You’re wasting my time and your money if you don’t keep your teeth clean!” Mind you, I’ve never said it, but the urge is great.
I believe hygienists come out of hygiene school slightly traumatized. After all, didn’t we get points counted off our grades if we left one little speck of plaque or calculus? We carry that mindset right into the workplace after we graduate. We believe that if every one of our patients doesn’t achieve some preconceived level of oral hygiene mastery, we’re a failure. The reality is that we take it far too personally if our patients refuse to comply with our instructions.
What about those homecare instructions? Is it possible that we expect our patients to perform homecare measures that are beyond their ability? Do we sometimes ask too much or put a homecare burden on them that they are unable to bear? Do we overestimate their dental IQ? Far too many times I’ve observed dental hygienists overwhelming their patients with too much information during one sitting. They teach a particular brushing technique, give detailed flossing instructions, bridge threaders, give interproximal brush instructions, use chlorhexidine, recommend an irrigating device, and then expect a patient to remember everything. It can be overwhelming to patients. The hygienist is lucky if patients will convert to even one new homecare behavior.
Some of our periodontal patients are dental cripples, meaning they have avoided care for so long that they have given up. The reasons they have avoided care vary but include money woes, drug or excessive alcohol use, apathy, lack of education, and an outright fear. Often, we don’t stop to consider why our patients have periodontal disease in the first place. Sometimes we don’t really care. All we know is that we have to fix it. Lack of compassion can hinder our communication efforts. One of my favorite sayings is, People don’t care how much you know, but they know how much you care.
Further, lack of passion on our part can negatively impact how well we communicate with our patients. Patients can sense whether or not we love what we do. They can sense if we are just going through the motions or if we are excited about how our efforts will improve their overall health and control oral infection. Hygienists should receive great personal fulfillment and professional satisfaction from taking a patient (through a series of appointments) from a state of disease to a state of good oral health. I believe you have passion for your work, because you state that you love treating periodontal patients.
We know from many studies that a patient’s level of personal oral hygiene is extremely important in achieving long-term success from our treatment. If the scaling has been thorough and we remove the hard accretions from the teeth, and if the patient performs excellent oral hygiene at home, the chances for a successful outcome are much better than for a patient with substandard oral hygiene.
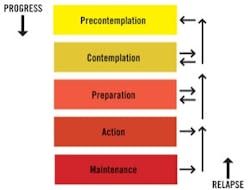
Before a patient will change his or her homecare behavior, there is a series of steps to pass through. The Transtheoretical Model of change was introduced in 1977 and describes a definitive process of change. In the “precontemplation” stage, a person is not ready for change and is unaware that change is needed. In the “contemplation” stage, a person recognizes there is a problem. In the “preparation” stage, a person intends to take action toward change. In the “action” stage, a person makes changes to a particular behavior. The next stage, “maintenance,” means the person has been able to sustain a new behavior. Finally, the “termination” stage means the person will not return to a former unhealthy mode. A person is said to “relapse” if he or she reverts back to former ways.
It is our challenge to help patients adopt healthy homecare routines. We must customize our instructions based on each patient’s needs and abilities. All people do not possess the same levels of manual dexterity. People that have been unsuccessful with dental floss may find success using any one of the available interdental cleaners available. We must be very careful about overwhelming our patients with too much information at one time. Try to master one thing, such as basic brushing, before expanding into more advanced homecare techniques.
The Transtheoretical Model of change was introduced in 1977.
Our patients must develop something called self-efficacy before they will adopt new homecare modalities. Self-efficacy is the belief that one is capable of performing a desired behavior. Lack of self-efficacy is the reason that a majority of our patients do not use dental floss correctly or on a daily basis. We can help our patients develop self-efficacy by taking small steps regarding homecare expectations. For example, if I dispense a power brush as part of my periodontal treatment protocol, I might ask the patient to use the new brush only on the teeth I scale that day for the first quadrant of scaling. That might be only five or six teeth. I would demonstrate the technique, put the brush in the patient’s hand, and help the patient learn. At the next quadrant scaling, the patient would bring the brush back, I would check the technique, and then add more teeth into the routine.
So what do we do about those patients who simply refuse to perform adequate oral hygiene? How can we “step on their toes” without “messing up their shine”? Here’s a good script to use.
“Mr. Jones, I’ve noticed consistently when you come in for your appointments that there is a lot of soft debris and food particles on your teeth. If these teeth aren’t kept clean – especially during this treatment phase – we can expect a much poorer result than we would get if the teeth were kept clean. Please tell me how I can help you with this problem.”
Help people where they are. Don’t overwhelm them with too much information. Show compassion, have passion for your ability to help people, and don’t take it personally when someone is noncompliant. After a while, you (like me) will come to the conclusion that “not very good” is the best some people will ever do with their personal oral homecare.
Best wishes,
Dianne
Dianne Glasscoe Watterson, RDH, BS, MBA, is a professional speaker, writer, and consultant to dental practices across the United States. Dianne’s new book, “The Consummate Dental Hygienist: Solutions for Challenging Workplace Issues,” is now available on her website. To contact her for speaking or consulting, call (301) 874-5240 or email dglass [email protected]. Visit her website at www.professionaldentalmgmt.com
Past RDH Issues