Treatment incorporates DNA testing to track progress in sensitive case
by MONA STOFFER, RDH, BSDH
As part of a new revolution in dental hygiene, my role as a dental hygienist has evolved into oral systemic care, which can involve other medical specialties. Oral systemic health-care incorporates the mouth and body connection to heal from the outside in and the inside out. Oral systemic health-care focuses on reversal of disease instead of merely treating the symptoms. Dentistry plays an instrumental role in putting together vital information for treating other serious systemic diseases.
No research has previously reported on treating a periodontal patient who has a drug-eluting stent in an artery of the heart. My research on drug-eluting stents brought me to the conclusion that it's vital to treat that patient like any other patient with periodontal disease. Pathogens should be reduced through scaling and root debridement, chemotherapeutic irrigation or rinsing, home-care regimens, power toothbrushes, oral irrigation devices, possible local or systemic antibiotic therapy, and educating the patient on the systemic effects of inflammation and its effect on heart disease. Lifestyle change is imperative, and dental hygienists can start to assist the process in their operatories.
Drug-eluting stents, sometimes referred to as "medicated" stents, are coated with a drug to prevent them from becoming occluded by a blood clot (thrombosis). The patient is typically on aspirin and an antiplatelet drug such as Plavix for a year or more after the stent is placed. Plavix can prevent blood platelets from attaching to the stent, which can result in a thrombosis of the stent and a heart attack. The main concern is the bacterial pathogen levels of the patient prior to treatment of his periodontal disease.
In dentistry, DNA pathogen testing such as MyPerioPath and MyPerioID PST (OralDNA Labs) is a simple saliva test provided chairside that reveals pieces of the puzzle for health-care professionals to provide more than the standard of care for their patients. Along with assessment and treatment of periodontal disease, the dental hygienist has to be educated in pathogens that are responsible for periodontal disease and the relationship they have with other systemic diseases. The PerioID PST is critical for the health-care professional as well as the dental team to determine the patient's susceptibility to inflammatory responses systemically and to determine overproduction of inflammatory promoting molecules such as interleukin-1 or IL-1. Interleukin 1 is a cytokine that participates in the regulation of immune responses. It's a guide for the dental team in personalizing supportive periodontal maintenance intervals and supports validation for its frequency.³
Case Study involving drug-eluting stent
This following case study is concentrating on periodontal therapy treatment for a patient with a drug-eluting stent after a myocardial event.
The patient is a 61-year-old Caucasian male. It has been five years since the patient sought dental care, and he has never had a comprehensive periodontal evaluation. The patient has risk factors that consist of a family history of periodontal disease and family history of heart disease in both parents.
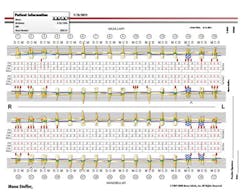
I initially consulted with the patient's cardiologist to ensure that the patient could safely undergo periodontal treatment, and I gathered a saliva sample and ran a DNA pathogen test. The pathogen test revealed severe, moderate, and less risk pathogens present with most severe above threshold (see Figure 1).
First and foremost, I wanted to decrease the pathogen levels before subgingival disruption to decrease pathogens entering the blood stream that could contribute to bacterial endocarditis. The patient was given a Sonicare Flexcare brush and was instructed to brush two times a day using 30-second quadrant intervals and to rinse nightly with chlorhexidine over a period that lasted approximately 10 weeks due to other medical complications that occurred during the home-care phase of treatment.
The patient was instructed to stop rinsing with chlorhexidine one week before the initial periodontal therapy to avoid misrepresentation with another pathogen test. The MyPerioPath test revealed a significant decrease in pathogen levels in all categories. The patient was premedicated with 600 mg of Cleocin one hour prior to his initial periodontal therapy, which consisted of data collection, pathogen testing, and coronal scaling and polishing.
The comprehensive periodontal charting revealed periodontal pocketing 4-6 mm in the posterior teeth with moderate/heavy bleeding and moderate bone loss: APA class IV (see Figures 2, 2a, 2b). I anticipated four to six visits of root debridement and pathogen disruption with antibiotic premedication, as long as pathogen levels remain above the threshold.
Premedication is not considered to be a standard indication for a drug-eluting stent, according to the American Heart Association. It is at the discretion of the treating dentist to premedicate, basing his/her decision on the oral pathology report. The MyPerioID PST test revealed that he is not at risk for periodontal disease because of over production of IL-1 (see Figure. 3). Repeating MPP is necessary in a stent situation to determine premed necessity and if the patient has periodontal disease due to other risk factors.
Homecare was modified with the use of a Sonicare Airfloss using two teaspoons of chlorhexidine in the reservoir nightly, brushing with Prevident Booster 5000 for one brushing daily for root sensitivity and interdental cleaning devices.
The patient completed five sessions of root debridement and pathogen disruption. At this point, the patient was given the recommended antibiotic, according to the OralDNA report. At the fourth week perio maintenance appointment, the patient's comprehensive periodontal charting revealed pocket depths between 2-4mm with localized 5mm and slight to moderate bleeding (see Figure 4). The MyPerioPath test was repeated, and I performed a full-mouth disruption with an ultrasonic scaler. The patient also repeated a systemic antibiotic, and was instructed to use the Waterpik in addition to his recommended daily care.
At this appointment, I did a MyPerioPath test on his wife. She had manageable pathogen involvement and one localized area of activity. I performed one session of debridement and instructed her to rinse with Peridex according to the label for eight days. She has excellent homecare and responded well. The wife and husband rinsed with Peridex together for the same length of time.
I then saw the husband at a closer interval of eight weeks and repeated a MyPerioPath test (see Figure 5) post-treatment. In the maintenance phase of periodontal therapy, I instructed the patient to use Therasol with xylitol both in a hand irrigator or Airfloss, and rinse on a daily basis to starve pathogens in their reproductive stages. During this phase, I stopped chlorhexidine use due to staining. The patient is stable and could be more compliant with homecare. However, his inflammatory markers have tremendously improved, and his recall interval was adjusted accordingly.
I also instructed my patient to seek nutritional and exercise counseling to manage and reverse cardiovascular disease. I found a Bale/Doneen trained doctor who recognizes that periodontal disease is a piece of the puzzle in the treatment and reversal of heart disease. My patient had extensive blood work and genetic testing to determine his risk factors. He has the gene associated with heart disease. This does not mean he cannot control the disease progression. There is a significant decrease in the inflammatory markers from his initial blood work taken while in periodontal therapy, to post-treatment testing six months later during the maintenance phase of periodontal therapy. By controlling inflammatory responses through diet, exercise, oral care, supplements, and medications, the effect of the gene can be otherwise managed.
Periodontal disease may not have caused my patient to have heart disease. However, the periodontal disease did contribute to the inflammation in his body that caused his heart disease. As clinicians, we need to identify our patient's risk factors: pregnancy, tobacco use, diabetes, other immune deficient diseases, a family history of heart disease, or periodontal disease. Once the risk factors have been identified, the patient's care and treatment can be personalized. Utilize the DNA testing to establish proper intervals of treatment and to determine the successful endpoint of treatment.
I will continue to educate myself in oral systemic health. Also, I will seek the clinical skills necessary to properly identify, treat, and refer to periodontists and other specialties when needed to provide overall health and wellness for my patients. This is truly a new revolution in dental hygiene. Educating our patients to make better choices and to change behaviors that are damaging to their oral health and ultimately their overall health. This paradigm shift has changed my lifestyle and the lifestyle of my loved ones. My family and I live healthier, more productive lives, and so can my patients. RDH
MONA STOFFER, RDH, BSDH, works in the practice of Dr. Caleb Robinson in New Philadelphia, Ohio. A graduate of West Liberty University in 1992, she obtained a bachelor's degree in dental hygiene. She is a founding member of the American Academy of Oral Systemic Health. She has extensive hands-on training with JP Consultants and the Las Vegas Institute for Advanced Dental Study. She can be contacted at [email protected].
Consider reading: RDH inflammation sleuth
http://www.rdhmag.com/articles/print/volume-29/issue-10/feature/rdh-inflammation-sleuth.html
Consider reading: Are you really ready?
http://www.dentaleconomics.com/articles/print/volume-102/issue-1/practice/are-you-really-ready.html
Consider reading: State of the oral-systemic union: 2013
http://www.dentaleconomics.com/articles/print/volume-103/issue-1/practice/state-of-the-oral-systemic-union-2013.html
Past RDH Issues