Dimensions in Imaging
by Mary Roper Hurley, RDH, MA
Consider reading: New dental X-ray recommendations
http://www.dentistryiq.com/articles/2012/12/autism-spectrum-disorder-new-dental-x-ray-recommendations.html
Consider reading: The Impact Of Technology In Dental Hygiene Education
http://www.rdhmag.com/articles/print/volume-32/volume-12/features/the-impact-of-technology-in-dental-hygiene-education.html
Consider reading: American Dental Association updates dental X-ray recommendations
http://www.dentistryiq.com/articles/2012/12/ada-updates-dental-xray-recommendations.html
Dental imaging rises to a new level with the use of cone beam computed tomography (CBCT). This exciting advancement provides 3-D views of head and neck anatomy that enable accurate diagnoses, more efficient workflows, and better treatment planning. CBCT images contain vast amounts of data that can be maneuvered with software tools for more in-depth viewing of an area and to see things that don’t show up in conventional 2-D images.
I was fascinated and intrigued with these images and wondered when or if this technology would become more mainstream. In particular, I wanted to learn what a hygienist needs to know about CBCT, and if CBCT has a place in a general dentistry office. To find answers, I did Internet research, read brochures, and talked with representatives from CBCT imaging manufacturers. I then had the opportunity to visit with Sue Moore, RDH, and her boss, Dr. Mitch Quintner, at Sensitive Care in Milford, Conn., and I attended a lecture on CBCT by Dr. Alan Lurie, chairman of oral and maxillofacial radiology at the University of Connecticut’s School of Dental Medicine.
The results of my research indicate that we as hygienists need to be able to describe the CBCT procedure to patients and explain the rationale for using it. This boils down to knowing why this type of X-ray is needed, its benefits, and how it compares to traditional imaging. This article provides information you can use to talk about CBCT with your patients.
Traditional imaging vs. CBCT
Traditional CT scanners use a narrow beam that rotates around the patient. Each rotation acquires one or more “slices,” but there can be gaps in information between each rotation. The system software reconstructs the data from the slices into images. The required number of rotations for a CT scan ultimately delivers more radiation to the patient than a CBCT scan does. The medical CT scan costs more than a CBCT scan, and therefore puts a higher cost on the health-care system.
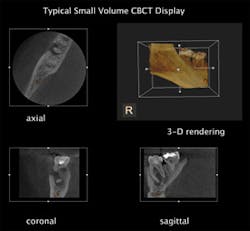
A CBCT scan collects all the anatomical data (known as a volume or data set) in one rotation. The system’s software then deconstructs the collected data to show dimensionally accurate images of the scanned area in different planes. The software allows manipulation of these images to show different slices at different angles, varying depths and thicknesses, 3-D reconstructions, and some renderings of soft tissue — all without image distortion. However, the detail of soft tissue shows better in medical CT images than it does in CBCT images.
How the CBCT system works
The CBCT system consists of an X-ray generator, a detector, and a computer. The generator and detector are mounted on opposite ends of an arm that rotates around the patient’s head. Most CBCTs look and move like a panoramic machine.
After the anatomical data is acquired and processed by the software, images can be displayed on the monitor in a variety of modes. All systems have panoramic, multiplanar, 3-D, and some sort of soft tissue rendering display modes. Some systems also offer maximum intensity projection and other special display modalities.
Software tools allow image enhancements in all planes for more intense viewing and/or diagnosis. Tool options include adding color to contrast different areas, zooming into or magnifying an area of interest, and measuring the size of a lesion or the distance between areas.
Exposure considerations
Radiation exposure with use of CBCT is relative to the size of the selected field of view (FOV) that is exposed. In general, effective radiation doses from CBCT images are greater than those of the same area exposed with conventional 2-D technology, such as cephalometric and panoramic images. However, the benefit derived is that CBCT images often provide more useful information than their 2-D counterparts.
The J. Morita Company brochures tout a 30% to 40% dose reduction on all their 3-D units and indicate an effective dose 25% less than a full-mouth series using E speed film. The i-CAT brochure states that a TMJ FOV with their system delivers 10 times less radiation than that of a traditional medical CT of the same area.
Sue Moore, dental hygienist at Dr. Quintner’s office, indicates that their system (the Sirona Galileos) has technology that can adjust the radiation dose by as much as 40% for young, small patients. Dr. Lurie adds that this technology is appearing in many of the new CBCT units.
CBCT applications
The areas where CBCT really shines appear to be in implantology, endodontics, and oral surgery. In implantology, CBCT provides the ability to see all three dimensions of the implant site with no geometric distortion. This allows a thorough bone analysis with accurate evaluation of anatomy that could affect proper selection, placement, and osseointegration of the implant. Among the many structures that CBCT images show are bone thickness and trabecular density, the exact location of the mandibular canal, the floor of the maxillary sinus, disease in the sinuses, and dental pathology.
For endodontics, CBCT images are powerful instruments for showing hidden or tiny canals, root fractures, and periapical disease. Being able to see what the problem is and where it’s located helps determine the correct patient treatment.
CBCT assists in oral surgery cases by locating root configurations that could pose potential complications. Being able to see this before surgery allows for better preparation and smoother procedures for patients and doctors.
Other areas where CBCT has significant impact on treatment planning include:
- TMJ analysis — CBCT images show bone morphology, joint space and function, trauma, and degenerative disease.
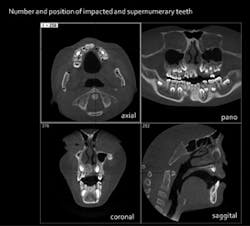
- Locating supernumerary teeth — CBCT images show the positions of supernumerary teeth and provide the means to determine an accurate relationship between the extra teeth and the structures surrounding them.
- Periodontal evaluation — CBCT images allow mapping of the bone defects associated with periodontal disease.
- Obstructive sleep apnea — In systems where the patient lies down for the exam, CBCT images allow analysis of the airway.
One area where CBCT is not recommended is routine orthodontic workups. Dr. Lurie said he is not aware of any study that shows cephalometric analysis using a large volume CBCT scan results in any different treatment outcomes than traditional cephalometric analysis using panoramic and lateral cephalometric radiographs.
CBCT technology does have a few downsides. These include the cost of the unit, the space it requires in an office (which is about the size of a panoramic machine), the learning curve, and the fact that it’s more of a bone imaging technology and does not significantly differentiate soft tissues.
CBCT in a general practice
The list of applications mentioned points to the system’s target audience being primarily specialty practices. However, there appears to be a place for this technology in general practice. Dr. Mitch Quintner says his group practice initially got their CBCT system to assist two of the doctors in the group, Dr. Alex Quintner who places implants, and their visiting periodontist.
Dr. Alex uses the CBCT scan to evaluate potential implant candidates, which saves them a trip to a medical facility for a more expensive and higher radiation dose CT scan that provides equivalent information. He also uses the system to perform virtual implants prior to the treatment to ensure a smooth, accurate, and efficient procedure the day of the implant. Because the office uses the CEREC system, Dr. Alex can send data from the scan to the CEREC that then constructs the stent that will guide the insertion of the actual implant. The visiting periodontist additionally uses CBCT for accurate viewing of bone loss and periodontal pathology.
The other doctors in this practice found the information in the CBCT images so useful that they wanted their patients to have the benefit of this technology. So when one of their patients has clinical indicators that point to prescribing a panoramic X-ray or FMX, they often recommend a CBCT scan instead. Both the patient and doctor feel the benefits. Although patients receive a dose of radiation approximately double the panoramic dose, they get a more comprehensive and dimensionally accurate exam for the same fee. The doctor gets more data and the ability to manipulate it for a more thorough patient exam. Findings that are questionable and beyond the scope of conventional dentistry are referred to specialists for further investigation.
Conclusion
It appears that the benefits of CBCT frequently outweigh its downside, and that CBCT can often be incorporated into patient care within the scope of radiation safety guidelines. Being able to provide images that allow more definitive diagnosis, help with treatment planning and follow-up care, and result in precise and favorable outcomes are clearly plusses for all involved. Being able to get information on teeth and bone structures roughly equivalent to that of higher-dose medical CT scans at lower cost and faster turnaround times are also plusses for patients.
With all that it has to offer, CBCT seems to hold a promising future in dentistry. I believe we’ll see its use increase in specialty practices and general dentistry. RDH
MARY ROPER HURLEY, RDH, MA, works part-time as a dental hygienist and as a technical writer for mammography and breast biopsy systems. Mary is also a freelance voiceover artist. She can be reached at mrhproductions.com or [email protected].
Past RDH Issues