to Premedicate or not?
By Jamie Collins, RDH, CDA
Last week a patient of mine returned to the office for her perio-maintenance appointment after a six-month interval. I seated her and asked one of my most repeated questions of the day, "Has there been any changes to your medical history, medications, surgeries, or anything different since your last visit?" Boy, did I open a can of worms with that one! She had a knee replacement seven weeks before, and had been battling an infection with the new joint. In addition, she had been undergoing chemotherapy for bladder cancer for the past three months.
Her immune system was overworked, and I wasn't about to treat her at this visit without a medical consult and antibiotic prophylaxis. I explained the conditions and possible risks with her before spending a little time visiting about the fun stuff like family, and before sending her on her way until we could consult her physician concerning treatment. This renews the question of antibiotic prophylaxis prior to dental treatment and who should be covered, and for how long.
The bacteria that live in the mouth enter the bloodstream through the daily activities of chewing, brushing, and flossing. Also, we all know we initiate a little bleeding with even the best of prophy visits. For most of the population with healthy immune systems, it poses no risk for infections. However, antibiotic prophylaxis is recommended for a percentage of the population to reduce the risk of infections elsewhere in the body as a result of the bacteria that is introduced into the bloodstream during dental treatment. In the 16 years that I've been in dentistry, I recall only three patients that suffered either a joint failure or endocarditis in correlation to dental treatment (thankfully before becoming patients at our practice). With the changing guidelines and so many conditions to be aware of, it's never easy to know when to premedicate a patient for treatment.
-------------------------------------------------------------------------
See related articles
- To premedicate or not to premedicate: The question continues to confuse many dental clinicians
- Insufficient evidence to premedicate patients with joint replacements prior to dental procedures: Great, but what should I do in my office?
- Premedication conundrum
-------------------------------------------------------------------------
Every few years the ADA, American Heart Association, and the American Academy of Orthopaedic Surgeons evaluate the existing guidelines and make or update the recommendations regarding premedication and conditions that should be considered. There are known risks when taking antibiotics, including stomach upset, allergic reactions that may include anaphylactic shock, and C. difficile infection, which can cause severe diarrhea and a host of other intestinal problems. Of course, we can't forget the ever-present risk of antibiotic resistance. For a group of individuals, the probable benefits associated with antibiotic prophylaxis outweigh the risks.
Endocarditis
The American Heart Association and the ADA previously recommended that nearly every type of congenital heart defect needed to be treated with antibiotics one hour before any dental treatment. The antibiotic premedication was intended to prevent an infection in the lining of the heart, heart valve, or blood vessels. Infective endocarditis (IE), also known as bacterial endocarditis (BE), is rare, but some individuals with certain heart conditions are at an increased risk of developing it.
Shunts and stents in the heart do not require premedication prior to treatment. This is a question that hygienists often ask. Many patients with heart murmurs have been told that they need to premedicate for life. They are now being told this is no longer necessary. The risk of endocarditis is extremely low and less than the risk associated with antibiotics.
In 2007 the AHA revised the recommendations on which individuals need antibiotic prophylaxis before dental treatment. This simplified the recommendation to include only the following:
1. An artificial heart valve, or a valve repaired with artificial material
2. A history of endocarditis
3. A heart transplant with an abnormal heart valve function
4. Certain congenital heart defects, including:
a. Cyanotic congenital heart disease (a birth defect with oxygen levels lower than normal) that has not been fully repaired. This includes children that have had a surgical shunt or conduits.
b. A congenital heart defect that has been fully repaired with artificial material or a device for the first six months after the repair procedure.
c. Repaired congenital heart disease with a residual defect, such as persisting leaks or abnormal flow at/or adjacent to a prosthetic patch or prosthetic device.
If may be confusing and a little unnerving for a patient that has spent years taking antibiotic prophylaxis every six months to suddenly be told that they no longer need it. I have had it happen in clinical practice several times, so I spend a little extra time explaining the reasoning, and then refer the patient to his or her physician for confirmation and peace of mind.
One of the three patients I had seen had a history of infective endocarditis following dental treatment. It put him in the hospital for nearly a month while his body battled the infection. He said he had not taken antibiotic prophylaxis before his dental visit like he had done for previous treatments. He simply forgot. Also, the clinician had not asked if he had taken the antibiotic prophylaxis prior to treatment, and it had nearly cost him his life. The lack of follow-up on the clinician's part left her vulnerable to being held legally responsible for the patient's resulting condition. Luckily for her, the patient considered it his fault for forgetting instead of holding the provider responsible.
Joint replacements
In 2012 the ADA and the American Association of Orthopaedic Surgeons (AAOS) evaluated and updated the guidelines for individuals with prosthetic joint replacements and antibiotic prophylaxis treatment. The risk of developing an infection within or around a prosthetic hip or knee joint was determined to be low, around 2%. In a statement released nearly a year ago, the AAOS and the ADA found insufficient evidence to recommend routine premedication for patients with prosthetic implants prior to dental procedures due to no direct evidence that routine dental treatment causes prosthetic joint infections. In addition, the AAOS recommends providers consider changing the longstanding recommendation of premedication prior to dental procedures. It finds no direct correlation between prosthetic joint infection and dental procedures. The AAOS no longer has a two-year minimum limitation on premedication recommendation.
I consulted with a few of the orthopedic surgeons concerning their opinion and recommendations about antibiotic prophylaxis and prosthetic joint infection risks. Most agreed that the individual should receive premedication for at least a short period of time after any joint replacement surgery. For individuals with a compromised immune system, antibiotic premedication may be appropriate, regardless of the amount of time that has passed after a joint replacement.
With the immune system compromised, the body is not able to ward off infectious microorganisms as easily and a patient is at risk to develop infections. Some examples of this may include diabetes, rheumatoid arthritis, cancer, chronic steroid use, and chemotherapy. Many people who have had prosthetic joint replacements are in the later part of life, and many of those have other health conditions as well.
The other two patients that I saw in the past suffered through a joint failure due to infection, which they believed was after dental treatment with no antibiotic prophylaxis. One of the individuals had to have the joint replaced a second time to alleviate the symptoms after the infection.
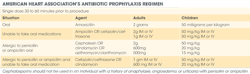
Antibiotic regimens
Now that you have decided that the patient needs to have antibiotic prophylaxis before dental treatment, what antibiotic do you use? The AHA has "wallet cards" that an individual's cardiologist may issue detailing the antibiotic and proper dose that should be administered. Remember that pediatric dosage depends on a child's weight, and may change over time. The most common recommended prophylactic antibiotic use is 2 grams amoxicillin for adults one hour before dental treatment. Amoxicillin is a broad-spectrum antibiotic that will help prevent many microorganism infections that may target the heart or joints. In case of an allergy to the -cillin family, clindamycin 600 mg is the next acceptable drug.
According to the AHA, antibiotic prophylaxis is recommended for all dental treatment except the following procedures -- anesthetic injections through noninfected tissue, dental radiographs, placement of removable prosthodontic or orthodontic appliances, adjustment of orthodontic appliances, placement of orthodontic brackets, shedding of deciduous teeth, and bleeding from trauma to the lips or oral mucosa.
A medical history should be updated at all dental visits and notated in the chart, even if there are no changes. At every office where I've worked, we have had a secured prescription of both amoxicillin and clindamycin on hand to administer if needed with the dentist's consent and prescription. Some patients may forget to take it before they arrive, or may not know it is necessary to take. Having it on hand makes it available to administer in-office instead of rescheduling and losing production. When administering an antibiotic premedication in the office, the clinician should wait at least 30 minutes before initiating any treatment that may cause bleeding. This will allow the medication to begin metabolizing in the bloodstream.
When in doubt, obtain a medical consultation with the individual's physician. It may be an inconvenience to both the clinician and patient, not to mention it almost always puts the office behind schedule, but it is better to err on the side of caution. There are many elements to consider, from the patient's health to your license and liability.
Most importantly, document in the chart the physician recommendation, date, drug prescribed, and dosage. If the physician does not want an antibiotic administered, document that information as well. Document that the patient needs premedication in an area in the chart that is easily visible for future appointments to assure everyone in the office knows to ask the patient at each visit. In most cases, if patients need to reschedule pending a consultation, I have found they are very responsive and grateful that you are watching out for their well-being.
Jamie Collins, RDH, CDA, resides in Idaho with her husband, Cory, and their four children. She currently works as a full-time hygienist as well as an educator at the College of Western Idaho. In addition, she acts as a content expert and contributor in multiple upcoming textbooks. She can be contacted at [email protected].
Past RDH Issues