Oral Lymphoepithelial Cyst
By Nancy W. Burkhart, BSDH, EdD
Your patient today is Andy, a 20-year-old college student. Andy has noticed a white to yellow swelling on the right side of his tongue that does not go away and has been present for at least four months. He has concern about this growth and, since he uses both alcohol and tobacco on a regular basis, he knows these habits place him at a higher risk for oral cancer.
His diet is poor, and he admits to eating "junk food" on a daily basis. He has no other health issues but believes that he is usually stressed with activities related to college and his part-time job. He has not had a dental visit in several years but has no other complaints except the noticeable growth.
Andy does show you a series of images of the growth in the floor of the mouth that he has taken with his cell phone over the course of several months. Andy tells you that the growth is non-tender without any sensations of pain. He believes the swelling has increased over time. At one point, he injured the nodule while eating and this caused some pain.
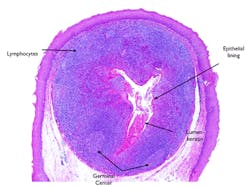
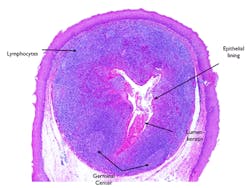
As you inspect the area in question, you note that the nodule is well defined, raised, and with a light yellow-white hue. It is moveable, soft, and exhibits no exudate (see Figure 1).
Oral lymphoid tissue is normally found in the area of the mouth called Waldeyer's ring that encompasses the posterior aspect of the mouth, including primarily the palatine tonsils, lingual tonsils, and pharyngeal adenoids. This area of the mouth has received much attention within the past few years because of the focus on oropharyngeal cancers that have been found in this region of the mouth and associated with HPV16. The tonsillar region is rich in lymphoid tissue and the crypts of the tonsil region can harbor bacteria, often walling off foreign material. This makes the formation of a cyst more likely.
-------------------------------------------------------------
Other articles by Burkhart:
-------------------------------------------------------------
Oral lymphoepithelial cysts (OLC), also known as intraoral lymphoepithelial cysts (LEC) or tonsillar crypt cysts, usually appear as a white or slightly yellow submucosal nodule. They are soft on palpation, less than 1 cm in size, and the patient usually reports a noticeable, painless swelling. Younger individuals may be affected, but these cysts may develop in any age group.
The prime area of the OLC is the floor of the mouth (see Figure 1) followed by the lateral border of the tongue, as well as the posterior tongue (see Figure 2). Most reported cases of the OLC occur unilaterally. However, a recent report by Silva et al. (2013) reports on a bilateral case of the OLC.
The OLC can also occur in the parotid area and may be an early indication of immunodeficiency when observed in the salivary region or parotid gland. Sujatha et al. (2013) makes the case that when OLCs occur in the parotid region, and there is suspicion of immunodeficiency in the patient, the finding may be helpful in treating early symptoms of immunodeficiency, since the prognosis is not as favorable in the later stages. Additionally the OLC is the most common cyst found in the immunocompromised patient. The patient should be tested for HIV infection. Fine needle aspiration cytology, imaging, as well as immunohistochemistry will assist in a definitive diagnosis.
Other areas in which the OLC may be found include the soft palate, mucobuccal fold, and anterior faucial pillars. Equal distribution in males and females has been documented. Yang et al. (2012), in a retrospective study, reported results from 120 patients who were diagnosed with OLC. The researchers found a male-to-female ratio of 1:2.24 with the mean age of the patients at 44.1, and an age range of 2 to 75 years of age. Although the OLC is considered an uncommon cyst of the oral cavity, the lymphoepithelial cyst may also occur in other areas of the body such as the thyroid, thymus, and pancreas.
Pathogenesis
It is believed that the OLC may be due to a traumatic injury that may cause proliferation of the lymphoid tissue. Damage to the salivary gland duct may also cause proliferation of the tissue with exuberance. Several theories exist, but the most accepted theory of its pathogenesis involves the accumulation of desquamated epithelial lining in the tonsillar crypt. This results in a dilated obstructed crypt of the oral tonsil region that presents as a mass lesion.
Histology
The oral lymphoepithelial cyst is composed of a cystic cavity. As with all true cysts, it has an epithelial lining. The cyst appears encapsulated by the surrounding lymphoid tissue (see Figure 3). The cyst is formed by dilation of the epithelial crypt normally present in lymphoid tissue, producing a cyst lined by stratified squamous epithelium.
The cyst lumen is filled with desquamated keratin and sometimes mucous cells are found in the epithelial lining. Germinal centers are present in the lymphoid tissue of the cyst wall. The fluid is viscous, and keratin content is present. Sometimes a cyst will occur in the proximity of the parotid gland or the lateral aspect of the neck as well. When the cyst is derived from degenerative tissue of the second branchial arch, it is referred to as a cervical lymphoepithelial cyst or a branchial (cleft) cyst.
Treatment
The treatment for the OLC is surgical removal, and recurrence is not expected. When the occurrence of the OLC is in the floor of the mouth, confusion may exist with mucous retention cyst and the lymphoepithelial cyst.
Additionally, because of the yellow hue of the OLC, there may be confusion with that of a lipoma, although the lipoma typically occurs in the buccal mucosa region. Salivary stones may have a similar appearance as well, but usually will involve pain. Other considerations may be dermoid cysts and salivary gland tumors. Biopsy confirmation is needed for a definitive diagnosis.
As always, keep asking good questions and always listen to your patients.
References
Silva IHM, Romanach MJ, Carvalho AT, de Almeida OP, Leao JC, Gueiros LA. Bilateral lymphoepithelial cyst of the tongue: a case report. Gen Dent 2013; Sep-Oct; 61(6): 32-4.
Sujatha D, Babitha K, Prasad RS, Pai A. Parotid lymphoepithelial cysts in human immunodeficiency virus: a review. J Laryngol Otol 2013; Nov 127(11): 1046-9.
Yang Xi, Ow A, Zhang CP, Wang LZ, Yang WJ, Hu YJ, Zhong L. Clinical analysis of 120 cases of intraoral lymphoepithelial cyst. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(4):448-452.
NANCY W. BURKHART, BSDH, EdD, is an adjunct associate professor in the department of periodontics, Baylor College of Dentistry and the Texas A & M Health Science Center, Dallas. Dr. Burkhart is founder and cohost of the International Oral Lichen Planus Support Group (http://bcdwp.web.tamhsc.edu/iolpdallas/) and coauthor of General and Oral Pathology for the Dental Hygienist. She was a 2006 Crest/ADHA award winner. She is a 2012 Mentor of Distinction through Philips Oral Healthcare and PennWell Corp. Her website for seminars on mucosal diseases, oral cancer, and oral pathology topics is www.nancywburkhart.com.
Past RDH Issues