Understanding caries detection devices: Technology assists minimally invasive dentistry
The technology assists the efforts associated with minimally invasive dentistry
By Susan Vogell, RDH, MBA, BS
There has been a paradigm shift within modern medicine to perform surgery more conservatively than in the past. Procedures that once required aggressive cutting can now be performed with laparoscopy or endoscopy. These minimally invasive approaches reduce injury to the surrounding tissues, muscles, and organs, which can lead to fewer complications, faster recovery, and often less pain. When it comes to the treatment and management of dental caries, modern dentistry is following in the footsteps of modern medicine.
Historically, it was believed that the only way to manage dental caries was through restorative intervention or extraction of teeth.1 Extensive research has shown that this is not the case. Dental caries is a bacterial disease. The bacteria that cause dental caries remain in the plaque biofilm on the teeth, capable of creating new areas of decalcification and subsequently, new caries. Cavitated lesions require restorative treatment. When identified early on, noncavitated lesions can be treated therapeutically. Modern caries management has evolved from a surgical approach to a noninvasive/preventive or disease management approach.
Along with the traditional caries lesion detection methods such as radiographs, air, and visual clues, new technology is available to help clinicians locate carious lesions in time to arrest and reverse the disease. Dental hygienists should familiarize themselves on the different available caries detecting technology to be aware of the correct indication and use. This article discusses commercially available caries detection devices. (Table 1 provides a list of the technology discussed.)
Minimally invasive dentistry
The new medical model of dental care, called minimally invasive dentistry (MID) is a conservative dental restorative philosophy that emphasizes the preservation of the tooth.2 MID is accomplished by risk assessment, early caries detection, remineralization, and-when needed-restoration of tooth structure.2 In cases when restorative intervention is needed, the goal is to preserve maximum tooth structure.2
Oral health professionals can use risk assessment tools, such as CAMBRA (caries management by risk assessment) to assess an individual's susceptibility to caries. The caries risk assessment (CRA) identifies the protective, pathological, and risk factors of a patient. Based on the CRA findings, patients are assigned to low, moderate, high, or extreme risk groups. By identifying patients who are at risk, early on, the disease can be prevented.3 Initial carious enamel lesions can be reversed or repaired by increasing the amounts of calcium, phosphate, and fluoride in the patient's saliva.3
Traditionally, dental caries has been diagnosed visually and by using explorers and radiographs. Some studies recommend that explorers no longer be used to detect caries, as the sharp tip of the explorer may disrupt areas of remineralization.4 Additionally, studies suggest that explorers may be inaccurate, because the tip can easily stick into a narrow, deep fissure with no decay present.4
Radiographs can detect interproximal caries when the lesion affects 30%-40% of the enamel surface; however, it is more commonly diagnosed at or beyond the dentinoenamel junction (DEJ).5 Due to the convexity of teeth buccolingually and the trajectory of the x-ray beam, occlusal decay is observed radiographically only after it has reached the DEJ.5 Therefore, radiographs are not the ideal method to detect incipient carious lesions.
The International Caries Assessment and Detection System (ICADS) was developed more than a decade ago to be used as a universal framework to diagnose coronal and root surface decay visually.6 The clinical scoring system is from 0-6, where 0 signifies sound enamel and 6 is severe decay into the dentin. Remineralizing products are recommended on a tooth with a score of 1 or 2.6 A score of 3 or higher warrants the need for more invasive intervention. The system relies on the physical limitations of diagnosing decay and the subjective interpretation of the clinician.7
Caries detection devices
Caries detection devices aim to overcome the limits of traditional diagnostic methods and can help identify caries at an earlier stage. Currently, there are numerous choices on the U.S. market, using a variety of technology. Most products employ the use of light, while others employ electrical signals to detect caries. All of the devices discussed are noninvasive. To date, none of the early caries detection devices have demonstrated the sensitivity (the true identification of caries, or true positive) or the specificity (the true identification of sound tooth structure, or true negative).8 For this reason, all caries detection devices must be used only in conjunction with the conventional methods for diagnosing decay.
Although it is the dentist who makes the dental caries diagnosis, the dental hygienist will perform a thorough assessment of the individual's oral health within the dental hygiene process of care.9 This assessment includes the evaluation of hard tissue for the presence of demineralization, caries, enamel defects, and the condition of existing restorations and sealants.9 In addition, the dental hygienist assesses the individual's caries risk by examining factors such as fluoride exposure, dietary practices, and salivary function.9 By evaluating a patient's caries susceptibility, the individual needs of the patient can be met.
There are many opportunities for dental hygienists to use caries detecting devices. Most often, caries detection devices are used for evaluating a visually suspicious area on a tooth. They can be used to evaluate enamel structure prior to sealant placement, and some early caries detection devices can also be used to check the sealant margins over time.10 They can also be used to gauge the effectiveness of remineralizing efforts. Finally, they can be used to monitor the successful caries risk reduction strategies of patients with moderate to high CRA scores. Furthermore, some quantifiable early caries detection devices can be used on patients longitudinally and any changes can be recorded, addressing treatment as needed. The technology allows clinicians to provide individualized patient care. The patients' level of involvement with their treatment plans increases as they are shown visual images of their teeth. Patients may be motivated to alter their oral hygiene efforts or make dietary modifications based on the information provided from using these devices.
CarieScan in use
DIAGNodent in use
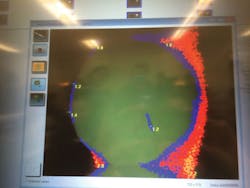
Image captured from Spectra
Fluorescent technology
Light fluorescence is most commonly used in caries detecting devices. The visible light spectrum makes up the colors the human eye can see.11 Wavelength is what makes the difference between colors and has a range of 400-700 nanometers (nm). Violet has the shortest wavelength and red has the longest.11
Fluorescence is the process where light of a short wavelength is absorbed and is emitted back at a longer wavelength.12,13 This amount of reflected light can be measured because the light absorption and reemission is different for carious tooth structure than for healthy tooth structure. Carious tooth structure will fluoresce, while healthy tooth structure will not.14
The disadvantage of using fluorescence technology is that any plaque, calculus, stain, or residual prophy paste can interfere with the caries detection, causing the areas to fluoresce when caries are not present.13 This is known as a false positive. To prevent false positives from occurring, the tooth must be thoroughly cleaned with either sodium bicarbonate or pumice and rinsed thoroughly.
DIAGNOdent- DIAGNOdent (KaVo, Biberach, Germany) is one of the first devices to use diode laser fluorescence technology to aid in the detection of caries. This small, handheld, battery-operated device contains two tips, one for smooth surfaces and one for occlusal surfaces.
The DIAGNOdent emits a red laser light at a wavelength of 655 nm.15 When caries is present, the light is absorbed and released back (fluoresces) at a higher level, 680 nm.16 There are two reasons for this occurrence. First, the tooth stimulates fluorescence due to the porosity associated with demineralization.17 The second reason is because the cariogenic bacteria, Streptococcus mutans, release metabolites known as porphyrins, which can absorb the energy and release it back at a higher wavelength.15-17 This infrared fluorescence corresponds to a numerical value between zero and 99.
A value between five and 10 signifies enamel caries, while a value between 10 and 20 indicates early dentin caries. A value higher than 20 denotes advanced dentin caries. While the DIAGNOdent detects dentin caries, it does not detect enamel demineralization.
The DIAGNOdent needs to be calibrated in the patient's mouth before it is used for caries detection. The clinician must continually move the device around the surface to obtain the highest value, and a signal sounds as values change throughout the exam. A newer version of the product is the DIAGNOdent pen, which can be used for interproximal areas.
Spectra- The Spectra Caries Detection Aid System (Air Techniques, Inc., Melville, N.Y., www.airtechniques.com) is another fluorescence-based caries detection system. The technology used is similar to that of the DIAGNOdent.14 Spectra uses six light-emitting diodes (LEDs) to project a blue-violet wavelength of 405 nm.18 The system connects to a computer via USB port and uses software analysis to determine the level of caries involvement.
The Spectra has two modes: detection and analyze. The detection mode is displayed in color. Healthy enamel is green while caries appears as red. In the analyze mode, the software provides numerical values. The values are as follows: 1.0 indicates early enamel caries, 1.5-2.0 denotes deep enamel caries, 2.0-2.5 indicates dentin caries, and 2.5 and higher signifies deep dentin caries.
The Spectra wand is handheld and portable, and an autoclavable rubber spacer fits over the lens. The spacer must be in contact with the tooth to produce consistent images. Images can be saved for monitoring. The device is self-calibrated, but the tooth must be dried thoroughly. Spectra can detect recurrent decay around existing amalgam and composite restorations.18
Soprolife- Soprolife (Acteon Imaging, La Ciotat, France, www.acteangroup.com) is a light-induced fluorescence intraoral camera system. Soprolife uses two types of LEDs to illuminate the tooth and evaluate changes in mineral density.19 Images can be captured in three different modes: daylight, diagnosis, and treatment. The daylight mode uses a high-level magnification intraoral camera illuminated with white LEDs.
The diagnosis and treatment modes use fluorescence via four blue LEDs at a 450 nm wavelength.20 This second light is directed at the tooth surface and produces a superimposed image over the white light image, a phenomenon known as autofluorescence.19 Soprolife uses a color-coding system. Green fluorescence is considered an indicator of healthy tissues, and red fluorescence indicates a carious lesion. The treatment mode can be used as a guide during cavity preparation. Images can be saved for future comparisons.
Caries ID- The Midwest Caries ID (Dentsply Professional, York, Pa.) is a handheld, battery-operated device that uses a light-emitting diode (LED) between 635 nm and 880 nm to measure the reflectance and refraction of light from the tooth surface.13 The Caries ID evaluates changes in the mineral density of the teeth.9,21 Demineralized or carious areas turn the LED from green to red, which is converted by fiber optics into an audible signal.9,21
The speed of the signal corresponds to the depth of the lesion; a fast signal indicates a deep lesion. The Caries ID has a one-step calibration. In addition to occlusal and smooth surfaces, it can be used on interproximal surfaces. Finally, it operates in a wet field and is not hampered by fluoride, making it particularly useful on children.22
The CanarySystem- The Canary System (Quantum Dental Technologies Inc., Ontario, Canada) uses a combination of laser light-induced luminescence and heat. The changes between emitted and absorbed energy from the tooth are converted into unique thermal and light signatures. The Canary System measures both the reflected light and the released heat from the tooth to examine the crystal structure of the tooth, thereby detecting the presence and/or the severity of decay.23
The science behind this technology is called Photothermal Radiometry and Modulated Luminescence (PTR-LUM).17 PTR-LUM makes it possible to detect caries under sealants and around the margins of existing restorations. Additionally, The Canary System does not require a dry field and is not hampered by stain.
The handheld wand and console are connected to a computer and can be transported to and from operatories. The Canary System uses a scoring system from 0-100, whereas 0-20 indicates a healthy tooth, 21-70 denotes an early carious lesion, and 71-100 signifies advanced decay.
CarieScan- The CarieScan (Dundee, Scotland) is another handheld, battery-operated device that uses multiple electrical frequencies to measure the mineral density of the tooth, thereby detecting the presence and severity of caries.17 The technology is called the Alternating Current Impedance Spectroscopy Technique (ACIST).15 Healthy or sound enamel exhibits high electrical resistance (impedance) and demineralized areas have lower resistance.19 Numerical values are as follows; 1-20 indicates sound enamel, 21-90 denotes enamel caries, 91-99 signifies early dentin caries, and a score of 100 is considered established dentin caries.
The CarieScan is not affected by staining as it does not rely on light, but rather electrical current.17 A low-voltage electrical current is delivered to the dried tooth and a lip hook is used to close the ACIST electrical circuit.19 The current is undetectable to the patient; however, due to the nature of the CarieScan, it cannot be used on patients with a pacemaker. The device is equipped with a test sensor to confirm that the device is working correctly.
CariVu- The CariVu (Dexis, Hatfield, Pa.) uses a newer approach called near infrared (NIR) transillumination to detect occlusal and interproximal carious lesions in their earliest form. Additionally, the CariVu can identify cracks. NIR transillumination uses longer wavelengths, allowing for deeper penetration into the tooth.24 In the NIR range, enamel appears translucent and carious lesions appear dark due to a scattering effect.24 An advantage to using this technology is that it does not require a clean tooth surface or calibration.
The CariVu is compact and portable. The black and white images read similarly to a radiograph and can be captured, saved, and stored to compare present and past images. It comes with two different sized tips, which can be autoclaved.
Oral health professionals can halt or reverse the caries disease process by detecting caries in its earliest form, thereby avoiding surgical intervention and preserving the natural dentition. New caries diagnostic technology aids in the support of minimally invasive dentistry by helping clinicians differentiate noncavitated areas from cavitated ones, and allows remineralization efforts to be employed.
Dental hygienists are at the forefront of MID, as prevention is the very essence of the profession. As part of the dental hygiene process of care, hygienists thoroughly assess patients' oral health, including an overall assessment of hard tissues. Caries detection devices would be most beneficial when used during this assessment phase. Dental hygienists should become familiar with caries detection devices, introduce this valuable supplemental tool to their patients, and help raise the standard of care. RDH
Susan L. Vogell, RDH, MBA, BS, is a clinical assistant professor of dental hygiene at New York University College of Dentistry and a clinical instructor at Farmingdale State University, where she provides dental hygiene clinical education. She has more than 15 years of private practice experience.
References
1. Clinical Affairs Committee. Guideline on Restorative Dentistry. Revised 2014. http://www.aapd.org/media/Policies_Guidelines/G_Restorative.pdf#xml=http://prdtsearch001.americaneagle.com/service/search.asp?cmd=pdfhits&DocId=424&Index=F%3a%5cdtSearch%5caapd%2eorg&HitCount=46&hits=3+1d+44+66+7a+b7+19c+1a4+1ed+22f+26d+274+28c+291+2c4+366+651+a42+b65+b7d+c8e+cfb+d89+e06+10ae+11ad+11c9+12ea+12fd+1417+142e+1473+14a0+155f+1912+1c96+20a6+23fa+2475+24aa+259b+25ed+2647+26f9+2873+28aa+&hc=1715&req=restorative+guidelines. Accessed September 22, 2014.
2. Murdoch-Kinch CA, McLean ME. Minimally invasive dentistry. J Am Dent Assoc. 2003;134(1):87-95.
3. Featherstone JD, Domejean-Orliaguet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35(10):703- 713.
4. Stookey G. Should a dental explorer be used to probe suspected carious lesions? No- use of an explorer can lead to misdiagnosis and disrupt remineralization. J Am Dent Assoc. 2005;136(11):1527, 1529, 1531.
5. Garg N, Garg A. Dental Caries. In: Textbook of Operative Dentistry. 2nd ed. New Delhi, India: Jaypee Brothers Medical Publishers (P) Ltd; 2013:chap 5.
6. http://icdas.org. Accessed January 10, 2015.
7. Altarakemah Y, Al-Sane M, Lim S, Kingman A, Ismail Al. A new approach to reliability assessment of dental caries examinations. Community Dent Oral Epidemiol. 2013;41(4):309-316.
8. Patel SA, Shepard W, Barros J, Streckfus C, Quock R. In vitro evaluation of Midwest Caries ID: A novel light-emitting diode for caries detection. Oper Dent. 2014;39(6):644-651.
9. www.adha.org/resources-docs/7261_Standards_Clinical_Practice.pdf. Accessed January 10, 2015.
10. Marsh L. Advances in caries detection. Dimensions of Dental Hygiene. 2014;12(5):42-44.
11. NASA.gov. What wavelength goes with what color? http://science-edu.larc.nasa.gov/EDDOCS/Wavelengths_for_Colors.html. Accessed October 30, 2014.
12. Shakibaie F, George R, Walsh LJ. Applications of laser induced fluorescence in dentistry. International J of Dental Clinics. 2011;3(3):38-44.
13. Diniz MB, Rodrigues JA, Lussi A. Traditional and Novel Caries Detection Methods. In: Contemporary Approach to Dental Caries. Rijeka, Croatia: Intech;2012:chap 6.
14. Graye M, Markowitz K, Strickland M, Guzy G, Burke M, Houpt M. In vitro evaluation of the Spectra early caries detection system. J Clin Dent. 2012;23:1-6.
15. Karlsson L, Tranœus S. Supplementary methods for detection and quantification of dental caries. J Laser Dent. 2008:16(1):6-14.
16. Goel A, Chawla HS, Gauba K, Goyal A. Comparison of validity of DIAGNOdent with conventional methods for detection of occlusal caries in primary molars using the histological gold standard: An in vivo study. J Indian Soc Pedod Prev Dent. 2009;27(4):227-234.
17. Amaechi BT. Emerging technologies for diagnosis of dental caries: The road so far. Am Inst of Physics. 2009:105(5):1-8.
18. Kurtzman GM. Caries visualization with fluorescent technology. Dentistry Today. December 9, 2010. http://www.dentistrytoday.com/diagnosis/4232-caries-visualization-with-fluorescent-technology. Accessed November 30, 2014.
19. Tassery H, Levallois B, Terrer E, et al. Use of new minimum intervention dentistry technologies in caries management. Aust Dent J. 2013;58(Suppl1):40-59.
20. Rechmann P, Rechmann BM, Featherstone JD. Caries detection using light-based diagnostic tools. Compend Contin Educ Dent. 2012;33(8):582-593.
21. Rodrigues JA, Huq I, Neuhaus KW, Lussi A. Light-emitting diode and laser fluorescence-based devices in detecting occlusal caries. J Biomed Opt. 2011;16(10):1-5.
22. Prabhakar NK, Kumar NK, Kala M. A review of modern noninvasive methods for caries diagnosis. AOSR. 2011;1(3):168-177.
23. Abrams S. Harnessing light and energy for the early detection of dental caries. Oral Health Group. December 1, 2009. http://thecanarysystem.com/pdfs/Detection/Harnessing-Light-Energy-for-Early-Caries-Detection-of-Caries.pdf. Accessed November 9, 2014.
24. Karlsson L. Caries Detection methods based on changes in optical properties between healthy and carious tissue. Int J Dent. 2010;2010, Article ID 270729: 1-9.