The role of H. pylori is a factor in discussions about systemic disease
BY Natasha Spisak-Terroade, RDH, BS
A new fad diet undertaken by a relative brought Helicobacter pylori (H. pylori) to my attention. I always take note of new dietary trends because it's only a matter of time before I see a patient who is a diehard adherent. There are often oral manifestations to contend with, usually in the form of bleeding gums due to vitamin deficiency.
Yet this was a diet of a different sort. The intent is to cultivate an internal alkaline environment to wipe out a particular acid-loving bacteria thought to cause all sorts of internal imbalances, particularly in the gut and gallbladder. The culprit? H. pylori.
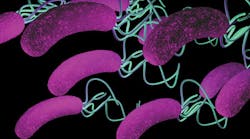
The mention of H. pylori brought me back to a darkened classroom with slides of various oral bacteria parading before a giant projector screen. Helicobacter pylori was thought to be a leading agent in periodontal disease. A gram-negative spiral rod bacterium, this vilified germ is capable of motility as it lashes about with its long appendages, plunging the depths of periodontal pockets and wreaking havoc on bone and tissue alike.
------------------------------------------------
Other articles to read
- Peri-implant diseases: Lack of consensus on treatment, but some research exists
- Oral bacterium possibly associated with systemic disease found in Alabama schoolchildren
- Enough talk about the oral-systemic link: It's time to bridge the gap between dentistry and medicine
------------------------------------------------
Yet, outside the classroom and in clinical practice, people are more than just their mouths. While the oral/systemic debate rages on, I had to investigate for myself to see if the oral presence of H. pylori was, in fact, contributing to health issues below the neck in my patients.
The information I sought was not only vast, but also widespread. Studies on the systemic effect of H. pylori are being conducted at home and abroad, with the United States, United Kingdom, Japan, and India publishing recent findings. In 2001, the World Health Organization classified H. pylori as a carcinogen.
In that respect, there is little doubt that H. pylori can be harmful. A February 2014 study reported, "Numerous studies have shown that H. pylori is the major cause of stomach inflammation, and is recognized as a key factor in the development of upper gastrointestinal tract pathologies including peptic ulcer disease, gastric cancer, extragastric intestinal malignancies, and gastric mucosal-associated lymphoid tissue lymphoma."1
The same study reported that there is a possibility that the mouth may act as a reservoir for H. pylori, causing a reinfection of the GI tract. The most common treatment for a GI infection of this bacterium is a triple antibiotic course, consisting of bismuth, tinidazole, and either doxycycline or amoxicillin. However, while this effectively kills H. pylori in the stomach, it has no effect on the population in the mouth. This may allow for reinfection as the bacteria once again migrate into the digestive tract. It is highly possible that keeping the mouth healthy with good hygiene may reduce the risk of GI infection in patients with a history of ulcers.
How is it healthy for the mouth?
Let's back up a minute. There is no doubt that H. pylori is unhealthy in the stomach and intestines, but what about the mouth? Since its discovery in 1981, it has been established that H. pylori is generally seen in modest quantities in a large portion of the population. In fact, it is believed to be a basic part of the general flora of oral bacteria.
However, it is now known that when the presence of H. pylori becomes excessive, it can cause periodontal disease. A study in India was published in 2001 in which 178 people (mostly males) were selected for their poor oral hygiene; 97% of them were infected with H. pylori. A control group was assembled of individuals selected for their good oral hygiene practices. Among them, only 23% were found to have H. pylori present.2
Of course, most dental offices don't have high-powered microscopes that will allow us to look at the kind of bacteria that make up the plaque biofilm in our patients' mouths. However, it is safe to assume that there is a good chance any given patient with periodontal pockets 5 mm in depth or deeper have oral H. pylori present in significant numbers. Even further, we can reason that studies such as the one conducted in India, where people with healthy mouths have a presence of H. pylori, health may not always be a matter of numbers but of strain.
There are two strains of H. pylori. There is the vacuolating toxin gene strain, or VacA, and the cytotoxin-associated gene strain, or CagA. Of the two, the latter is much more virulent. None of the studies researched mentioned whether a particular strain was looked for in the oral screenings. It is possible that healthy mouths with an H. pylori presence were of the weaker strain. However, both strains are known to stimulate both the local and systemic inflammatory responses.3
Most oral infections of H. pylori occur early in life, commonly transmitted from parent to child by the sharing of spoons as the parent feeds the baby. Once transmitted to children, the bacteria pass on to their classmates in a similar fashion. This bacterium thrives in the pockets around teeth and in an acidic environment, adding to the inflammation common in decay-prone patients.
Oddly enough, my research took me to Urology Journal, where a study was done on H. pylori's role in causing infections of the urinary tract. One possible method of transmission is the spread of oral H. pylori to the genitals via oral sex, especially putting women at risk as the vagina has the ideal acidic requirements for H. pylori to thrive.4 While AIDS and other serious issues surround the practice of oral sex, they are hardly the only concerns. Urinary infections are treatable but certainly unpleasant and lead to the need for antibiotics, of which the United States is already using to excess.
Even more disturbing was the discovery of a strong correlation between H. pylori and oral cancer. H. pylori is difficult to test for by culture, but easy to diagnose by looking for antibodies in a blood sample. Such antibodies were found in 64% of a population of patients with squamous cell carcinoma of the head and neck, according to one study.1
Naturally, a correlation doesn't necessarily mean there is causation, and there are patients with cancer who test negative for H. pylori antibodies. However, cancer is yet to be fully understood in its etiology. If reducing H. pylori can reduce a person's risk, there is no downside.
The systemic connection
Where does all this information leave the hygienist? While the studies are not always conclusive, they are highly suggestive. The World Health Organization considers H. pylori to be detrimental to people's health, and that alone is enough to warrant a discussion with patients.
If the bacteria in our mouths had no systemic effect, there would be no need to give a prophylactic antibiotic to patients with joint replacements. My experience has often been surprise when I explain to hip or knee replacement patients that antibiotics are required to protect them from possible infection. All too many people see their mouths as unrelated to the rest of their bodies. Teaching patients the importance of oral health and how it reflects on their overall well-being is not an option; it's our job.
It's also true that most people are less than forthcoming when it comes to filling out their health history forms. Many will say, "I had no idea you needed to know that" when asked questions pertaining to surgeries, diabetes, heart conditions, pacemakers, and even pregnancies. It's not hard to see that America is undereducated when it comes to the impact that oral bacteria can have on general health.
How to approach the subject depends on the patient. A basic explanation of how bacteria can move from the mouth through the bloodstream when patients have inflamed and bleeding gums should be preliminary to patient education. However, in reviewing the medical history form, certain patients with chronic conditions should have the oral/systemic connection stressed. Patients with gastric ulcers, respiratory diseases, compromised immune systems, and conditions such as cardiovascular disease or diabetes should all have instruction in proper home care while stressing oral bacteria's role in exacerbating their condition.
Deep scaling and root planing should be performed whenever indicated, and, in some cases, a local antibiotic such as Arestin or Atridox can be used as well.
Another very effective natural alternative is the use of mastic gum. Made from the resin of Pistacia lentiscus, a tree native to the Mediterranean, this natural remedy has antibacterial properties that have been shown to kill H. pylori. Mastic gum is often used as an ingredient in oral rinses and toothpaste.
Taking care of one's teeth has been listed among the "100 things to do to live to 100." After seeing the link between oral and systemic health as indicated by so many studies, there is little doubt that dental care is a necessity to human thriving. Hygienists spend more time with patients than any other dental professional and, thus, we are in a position to impact our patients' health drastically by presenting them with the insights gleaned from all this research. RDH
Natasha Spisak-Terroade, RDH, BS, is a hygienist in New York City's Midtown at a large multidoctor practice. Her bachelor's degree had a dual focus on bioscience and communications. Natasha's interests lie in patient education and compliance, utilizing both scientific understanding and strong communication skills to educate and encourage her patient base.
References
1. Shin K, et al. An association between Helicobacter pylori and upper respiratory tract disease: Fact or fiction? World J Gastroenterol. 2014 Feb 14; 20(6):1470-1484.
2. Periodontal disease is linked to heart attacks and strokes. Life enhancement.com. January 2001. http://www.life-enhancement.com/magazine/article/522-periodontal-disease-is-linked-to-heart-attacks-and-strokes.
3. Al-Marhoon MS. Is there a role for Helicobacter pylori infection in urological diseases? Urol J. 2008 Summer; 5(3):139-43.
4. Eslick GD. Oral-genital transmission of Helicobacter pylori: fact or fiction? http://www.gastrohep.com/freespeech/freespeech.asp?id=25.
5. Sayed AA, et al. Oral cavity as an extragastric reservoir of Helicobacter pylori, ISRN Gastroenterology, vol. 2014, Article ID 261369, 16 pages, 2014. doi:10.1155/2014/261369.
6. Bürgers R, et al. Helicobacter pylori in human oral cavity and stomach. Eur J Oral Sci. 2008 Aug;116(4):297-304. doi: 10.1111/j.1600-0722.2008.00543.x.