Investigating the incisive block: Procedure minimizes soft tissue discomfort
BY Laura J. Webb, RDH, MS, CDA
The incisive block is a mandibular injection of importance to dental hygienists. Often, we prefer not to provide a mandibular block (inferior alveolar block, Gow-Gates block). For example, if the patient does not require anesthesia for molar teeth, the incisive block is a good alternative. It provides very good anesthesia to the teeth anterior to the mental foramen on one side without the discomfort of anesthesia to the tongue.
This is particularly useful when we wish to complete the mandible in one visit, and for at least one side, molar anesthesia is not indicated. As you recall, bilateral mandibular blocks should not be provided during nonsurgical periodontal procedures because of patient discomfort and function.1-6 Also, due to nerve fiber crossover, when anesthesia of the anterior teeth fails after a mandibular block, this injection can be useful when provided on the contralateral side.1-3
----------------------------------------------------
Other articles from DentistryIQ
- Local anesthesia options during dental hygiene care: Answers to common questions about pain control in the hygiene operatory
- Dental anesthesia may interrupt development of wisdom teeth in children
- Local Confidence: Regain that confident feeling about anesthesia
----------------------------------------------------
Lingual anesthesia is not achieved with the incisive block. However, adequate lingual anesthesia for the purposes of nonsurgical periodontal therapy may be easily provided with a supplemental technique (described later below).
General Anatomical Considerations
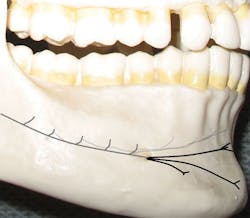
The inferior alveolar nerve, which travels through the mandibular canal, bifurcates just posterior to the mental foramen (see Figures 1, 2) to become the incisive nerve (continues to the midline through the mandibular canal) and the mental nerve (exits at the foramen and courses outside the bone toward the midline). When we provide a mandibular block, both nerves are anesthetized.
The incisive and mental nerves should not be confused. The incisive nerve innervates the pulps of the teeth anterior to the mental foramen, usually the premolars through the centrals on one side. The mental nerve innervates the skin of the chin, lower lip, and facial soft tissues anterior to the mental foramen on one side.
The difference in the provision of the incisive and mental blocks is that during provision of the incisive block, gentle pressure is applied over the foramen to direct anesthetic into the foramen toward the incisive nerve. Due to the location of the mental nerve, when providing the incisive block, both the mental and incisive nerves are anesthetized. For this reason, the incisive block is sometimes referred to as the incisive-mental block.
Figure 1: Abbreviated illustration of pathway: Incisive nerve (grays), mental nerve (black)
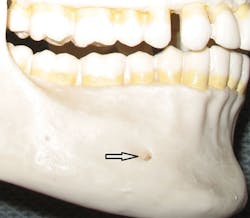
Figure 2: Mental foramen
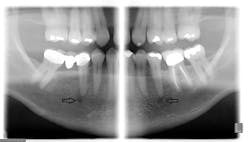
Since only the soft tissues are anesthetized by the mental block, the incisive block is preferred for nonsurgical periodontal therapy procedures. The mental foramen, which opens anteriorly and superiorly, is usually located near the apex of the second premolar (see Figure 2), although studies indicate that it can be located from the distal of the canine to the first molar.3-5 It is advisable to check the radiographs and palpate the area prior to procedures to determine its location. The foramen appears as a round or oval radiolucency on radiographs (see Figures 3, 4) and may be palpable as a concavity or rough elevation.2
General Technique1-6
1. The clinician should be positioned at the 8-9 o'clock position (facing the patient) for a horizontal approach to providing the injection. This is preferred over the vertical approach (from 11-1 o'clock), because it enables the clinician to keep the syringe below the patient's line of sight.
2. Check the radiographs for the location of the mental foramen and gently palpate for the depression with finger or cotton-tipped applicator. Note: Pressure on the mental nerve can be uncomfortable.
3. Apply topical anesthetic for one minute to the insertion site, anterior to the mental foramen.
4. A 25-gauge short needle is recommended due to the aspiration rate of 5.7%, but a 27-gauge short is commonly used.
5. Make the tissue taut for atraumatic penetration (sensitive tissues and close proximity of bone) by retracting the lower lip and the buccal mucosa outward. The use of gauze may be helpful to control the tissue.
6. With the bevel oriented toward the bone, insert the needle at the depth of the mucobuccal fold usually at the canine or first premolar. Resting the syringe barrel on the finger providing retraction assists in stabilization (see Figure 5).
7. Advance, slowly, toward the foramen (see Figure 6), approximately 5-6 mm; aspirate in two planes. Avoid contact with bone.
8. After negative aspiration, slowly deposit 0.6mL-0.9mL (⅓ to ½ cartridge) of anesthetic for a minimum of 30 seconds outside the foramen. Minimize ballooning. To avoid trauma to the nerves and blood vessels, entering the mental foramen is not recommended.
9. Some experts recommend that gentle finger pressure be applied over the injection site during deposition to maximize the amount of anesthetic entering the foramen.1
10. Immediately post-injection, gentle finger pressure should be applied at the injection site intraorally/extraorally for two minutes by the clinician or patient. Repositioning the patient to a semi-supine or upright position may assist in better diffusion of the anesthetic.
11. Wait at least three minutes before beginning procedures. The sensation of numbness to skin and soft tissue (mental nerve) will be almost immediate. Complete anesthesia to the incisive nerve and associated tissues follows.
Figure 3: Panoramic radiograph of right and left mental foramina. (Courtesy of Bruce Dow, DDS)
Figure 4: Periapical radiograph of left mental foramen. (Courtesy of University of South Dakota Dental Hygiene Program)
Special Considerations
Careful attention to proper technique assists in avoiding patient discomfort which is often related to: inadequate topical, inadvertent contact with bone, or rapid deposition. The success rate for the incisive block is very high. Inadequate anesthesia, though rare, is usually related to deposition too far from target, inadequate volume of anesthetic, inadequate duration of pressure, or, in rarer cases, to an unusually small foramen.1,2,4 A 2010 study demonstrated that 4% articaine 1:100,000 epinephrine can provide a higher success rate, longer duration, and more profound anesthesia for teeth associated with the incisive block than 2% lidocaine 1:100,000 epinephrine.7
Figure 5: Insertion and stabilization
Figure 6: Angulation and target
Lingual Anesthesia
As previously mentioned, the incisive block does not provide lingual anesthesia. For the purposes of nonsurgical periodontal procedures, adequate lingual anesthesia can easily be accomplished in limited areas by providing interpapillary infiltrations at the mesial and distal aspects of the teeth of interest.
Using a 27-gauge short needle, penetrate the interdental papilla from the facial and slowly advance the needle toward the lingual, while depositing the anesthetic. The infiltrations should be atraumatic because the facial tissues will already be anesthetized by the incisive block.1,6 An added benefit of this technique is that it provides additional hemostasis if an anesthetic with vasoconstrictor is used.
The incisive block can be very useful when indicated, because it provides very good anesthesia to the area anterior to the mental foramen while minimizing soft tissue discomfort during and after procedures. An additional advantage is that less volume of anesthetic is required than with mandibular block techniques, even when we provide additional papillary infiltrations to obtain lingual anesthesia. RDH
References
1. Malamed S. 2013 Handbook of Local Anesthesia 6th ed. Elsevier.
2. Bassett K, DiMarco A, Naughton D. 2010 Local Anesthesia for Dental Professionals. Pearson.
3. Fehrenbach M. The horizontal incisive block underutilized but ultimately useful. Journal of the California Dental Hygienists' Association, Summer 2011.
4. Logothetis D. 2012 Local Anesthesia for the Dental Hygienist. Elsevier.
5. Logothetis D, Fehrenbach M. Local anesthesia options during dental hygiene care. RDH June 2014; 34(6).
6. Darby L, Walsh M. 2010 Dental Hygiene Theory and Practice, 3rd ed. Saunders.
7. Batista da Silva C, Berto LA, Volpato MC, Ramacciato JC, Motta RH, Ranali J, Groppo FC. Anesthetic efficacy of articaine and lidocaine for incisive/mental nerve block. J Endod. 2010 Mar;36(3):438-41.
LAURA J. WEBB, RDH, MS, CDA, is an experienced clinician, educator, and speaker who founded LJW Education Services (ljweduserv.com). She provides educational methodology courses and accreditation consulting services for allied dental education programs and CE courses for clinicians. Laura frequently speaks on the topics of local anesthesia and nonsurgical periodontal instrumentation. She was the recipient of the 2012 ADHA Alfred C. Fones Award.