The expert advice: Dental patient compliance hinges on effective communication strategies
By Diana Macri, RDH, BSDH, MSEd, AADH
Compliance: from the Latin word complire, meaning to fill up and hence to complete an action, transaction, or process and to fulfill a promise. The acting in accordance with, or the yielding to a desire, request, condition, direction.
Most dental hygienists would agree that motivating patients to adopt good oral health behaviors-often referred to as compliance-is the most challenging aspect of practice. This critical component of patient care is not unique to dentistry and dental hygiene. In 2010, the costs of health care in the United States exceeded $2.7 trillion with "between $100 and $300 billion of avoidable health-care costs [attributable] to nonadherence in the US annually."1 Nonadherence (a term used in the medical literature, which is synonymous with noncompliance) is associated with progression of disease and, subsequently, poor health outcomes resulting in an additional burden of billions per year in avoidable health-care costs. Patient compliance is a multifaceted issue that is influenced by many factors. As oral health researchers continue to provide scientific evidence to further the connection between oral and systemic health, it has never been more important for dental hygienists, as disease prevention specialists, to adopt techniques that can improve communication and patient compliance.
The current situation
The effect of patient demographics (for example, sex, age, socioeconomic status) on compliance is small and noncompliance is widespread. This is due to many reasons, including patient self-determination, depression, health literacy, lack of support, and resources.2,3 Traditional dental health education approaches, the main focus of which is improving oral health knowledge, have not been effective in improving the nation's oral health. Consider these statistics:
1. Dental caries remains the most prevalent chronic disease in both children and adults, even though it is largely preventable.
- 42% of children ages two to 11 have had dental caries in their primary teeth.4
- 21% of children six to 11 have had dental caries in their permanent teeth.4
- 59% of adolescents 12 to 19 have had dental caries in their permanent teeth.4
- 92% of adults 20 to 64 have had dental caries in their permanent teeth.4
- 18% of seniors 65 and older have untreated decay.4
2. In the United States, 47.2% of adults have mild, moderate, or severe periodontitis.5
3. Only 64% of Americans have visited a dental office in the past year.6
Generic recommendations such as "brush your teeth twice a day for two minutes and limit your intake of sugar" have had limited success in changing oral health practices and improving overall systemic health. Why don't Americans place a higher value on their oral health? What can dental hygienists do to improve the public's opinion of oral health?
What you say and what your patients hear
Health literacy refers to the degree to which an individual has the capacity to obtain and understand basic health information and services to make appropriate health decisions. The average American adult reads at an 8th to 9th grade reading level,7 yet health-care materials are written at a 10th grade reading level. Thirty-six percent of adults have basic or below-basic health literacy skills.7 This means that for one-third of the population, health information is too hard to understand, and many people struggle to properly complete the insurance, medical history, and consent forms that are standard in all dental offices. Add to that the HIPAA privacy policies and individual office policy forms, and it's easy to see why confusion abounds.
In their study evaluating the health literacy of parents in the United States, Yin et al.8 found that 28.7% of the parents had below-basic/basic health literacy; 68.4% were unable to enter names and birth dates correctly on a health insurance form; and 46.4% could not properly perform at least one of two medication-related tasks. The annual health-care costs of poor health literacy are estimated at $106 to $238 billion dollars.9 More importantly, poor oral health literacy has been linked to poor overall health outcomes and, with the increasing body of evidence, many are advocating for a simplification of the delivery of health care and nutrition information. The American Dental Association provides guidance to dental professionals with its "Health Literacy in Action Plan," which is available for download from the ADA website.
It's easy, then, to understand why clear, positive communication between a dental hygienist and the patient is so important. Communication is the process whereby one sends a message to another to impart information and ideas. Even more, it is about understanding the emotions and and intentions behind the message. Words are the basis for this process, but a great deal of communication occurs nonverbally. Facial expression, eye contact, gestures, posture, gait, and touch can all be used to great effect. Touching a person's shoulder or upper arm, for example, increases a person's willingness to comply with requests.10 Touching also improves college students' class performance and can be a highly effective teaching tool.11
In order for communication to be effective, the sender and the receiver share responsibilities. Much empathy and concern can be expressed by maintaining direct eye contact and listening attentively to a patient's concerns. Those who wish to learn more about the fascinating world of body language should read "The Nonverbal Advantage: Secrets and Science of Body Language at Work," written by Carol Kinsey Gorman, PhD. It's an excellent quick read that discusses the seemingly endless ways in which we unknowingly communicate with our bodies.
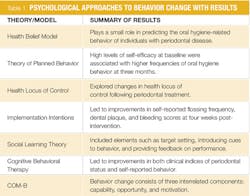
Psychological approaches to behavior change
Psychological models of behavior change provide a foundation from which to understand behaviors. In their systematic review, Newton and Asimakopoulou12 identified 19 studies that tested psychological models and their effect on oral hygiene-related behaviors. Their findings are summarized in Table 1. All of the models used several variables that increased the likelihood of participants' adopting positive oral hygiene behaviors. The most important of these are the perceived benefits of a behavior and a person's self-efficacy. Additionally, models that used goal setting, planning, and monitoring of behavior were more effective than those using different interventions. The authors noted the poor quality of studies and high risk of bias. Clearly, this is a field in desperate need of further study.
Two approaches that merit deeper discussion are cognitive behavioral therapy and motivational interviewing.
Cognitive behavioral therapy (CBT)-CBT is a technique that focuses on adjusting thought patterns which cause negative emotions and, consequently, behavior. It first emerged in the 1960s and differs from other therapeutic techniques most notably in its simplicity. CBT doesn't aim to explore a person's upbringing and development the way that psychoanalysis does; rather, CBT implies that distress is caused by irrational beliefs, and notes that it's within a person's power to recognize those beliefs and change them. Maya Angelou was on to it when she said, "Do the best you can until you know better. Then when you know better, do better."
CBT has received a lot of attention, and its success in treating a variety of mental disorders (including anxiety and depression) is well documented.13,14 There is also evidence that it improves medication compliance, which is, no doubt, what has prompted some oral health researchers to apply its principles to the broader topic of patient compliance in oral health.
Motivational interviewing (MI)-MI is an evidence-based, client-centered, personalized counselling approach based on the transtheoretical model of behavior change. Miller and Rollnick15 state that "for a person to change, they must feel both confident in their ability to change and believe the change is important to them." MI sees behavior change as a partnership between the patient and the dental hygienist . . . a partnership that respects autonomy, enabling the patient to feel engaged, understood, and empowered.
Rather than the dental hygienist assuming the role of "expert," MI places the patient in that role, letting him or her decide how to integrate information and make the final decision as to whether the behavior is relevant and important for him or her to adopt. During MI, the dental hygienist's goal is to resolve ambivalence toward change in the patient and tap into his or her already-existing motivation by eliciting "change-talk" and using reflective listening, affirmation, and summations. Ambivalence is the term used to describe patients whose actions do not match their desires. A patient who states he or she wants to prevent periodontal disease yet does not floss or brush regularly is displaying ambivalence.16
MI allows the patient to exercise autonomy and encourages shared decision making. In contrast to the old model of paternalism-where the dental hygienist may have dictated recommendations to the patient-shared decision making is a process where a health-care provider and the patient arrive at decisions regarding the patient's care together.17,18 MI has become the standard of care in medicine, and dentistry is slowly catching on. Table 2 below discusses the four components of MI.
Studies have shown an improvement in MI when the clinician follows up the initial conversation to maintain contact, problem solve, reinforce commitment, and provide support. Ideally this would be done in a face-to-face meeting at the dental office, but a conversation over the telephone is sufficient and has been shown to increase the effectiveness of MI.
Patient compliance begins with a good understanding of the human psyche and the motivations behind our behavior. While most dental hygiene programs require that students complete an introductory psychology and sociology class as part of their degree completion, the content offered is barely enough to make a dental hygienist proficient in any of the techniques mentioned here. However, lifelong learning is a responsibility dental hygienists take when they assume the role of professional.
While the dental literature is lacking in content regarding effective behavior modification techniques that oral health professionals can implement, the medical literature offers a great deal of information and sources. The Journal for Patient Compliance offers easy-to-understand, readily accessible, peer-reviewed articles on all aspects of compliance. Behavior Modification is another peer-reviewed journal devoted exclusively to the topic of changing behaviors in psychiatric, clinical, educational, and rehabilitative settings.
Evidence-based decision making requires dental hygienists to stay current with the most recent evidence and master skills that improve patients' health outcomes. Continuing to use outdated and ineffective practices endangers patient health, minimizes the practice of dental hygiene, and contributes to the poor health of Americans. Exploring new paths can be frightening.
However, dental hygienists in the past two decades have done much to expand the body of research regarding dental hygiene. There is no single practice that has a greater, longer-lasting impact on oral health than practicing proper oral hygiene. If we can find the most effective way of communicating with our patients, there is no doubt that the incidence of oral disease in this country would drop drastically. That is our greatest responsibility. RDH
When communicating with your patients, there are factors that enhance and inhibit effective communication. Learn the difference.
Factors that enhance communication:
- Stop! Devote 100% of your focus on your patient. Orient your shoulders and legs toward the patient, arms in a relaxed position and uncrossed, sitting on the edge of your seat, maintaining eye contact.
- Show interest; listen!
- Provide feedback: paraphrase, summarize, praise.
- Pay attention to your patient's body language.
- Clarity: Make your message simple, brief, and direct. Enunciate clearly, keep your words simple, repeat the most important part of the message.
- Humor: Laughter stimulates endorphin release and reduces anxiety.
- Use aids such as models, radiographs, and printed materials with engaging pictures.
- Respect cultural differences.
Factors that inhibit communication:
- Offering false reassurance; a critical component of dental hygiene professional practice is veracity and informed consent
- Being defensive; patients often neglect to take responsibility for poor oral health
- Interrupting and/or making judgments
- Showing disapproval
- Changing the subject
- Using difficult words/concepts
- Speaking too fast
Diana Macri, RDH, BSDH, MSEd, AADH, is an assistant professor at Hostos Community College in New York City. She can be contacted at [email protected]
References
1. Iuga AO, McGuire MJ. Adherence and health care costs. Risk Management and Healthcare Policy. 2014;7:35-44. doi:10.2147/RMHP.S19801.
2. DiMatteo MR. Variations in patients' adherence to medical recommendations: A quantitative review of 50 years of research. Med Care. 2004;42(3):200-209.
3. Rozier RG, Horowitz AM, Podschun G. Dentist-patient communication techniques used in the United States: The results of a national survey. Journal of the American Dental Association. 2011;142(5):518-530.
4. United States, National Health and Nutrition Examination Survey, 1999-2004. http://www.nidcr.nih.gov/DataStatistics/FindDataByTopic/DentalCaries/DentalCariesChildren2to11.htm#Table1
5. Eke PI, et al. Prevalence of periodontitis in adults in the United States: 2009 and 2010. Journal of Dental Research. 2012;91(10):914-920.
6. One Third of Americans Haven't Visited Dentist in Past Year. http://www.gallup.com/poll/168716/one-third-americans-haven-visited-dentist-past-year.aspx
7. Baer Justin, et al. Basic Reading Skills and the Literacy of America's Least Literate Adults: Results from the 2003 National Assessment of Adult Literacy (NAAL) Supplemental Studies. NCES 2009-481. National Center for Education Statistics. 2009.
8. Yin HS, et al. The health literacy of parents in the United States: A nationally representative study. Pediatrics. 2009;124(S3):S289-S298.
9. Vernon JA, Trujillo A, Rosenbaum S, DeBuono B. Low health literacy: Implications for national health policy. Available at: http:// npsf.org/askme3/pdfs/CaseReport10 07.pdf. Accessed January 29, 2016.
10. Haans A, de Bruijn R, IJsselsteijn W. A virtual Midas touch? Touch, compliance, and confederate bias in mediated communication. Journal of Nonverbal Behavior. 2014;38(3):301-311.
11. Steward A, Lupfer M. Touching as teaching: The effect of touch on students' perceptions and performance. Journal of Applied Social Psychology. 1987;17(9):800-809.
12. Newton J, Asimakopoulou K. Managing oral hygiene as a risk factor for periodontal disease: A systematic review of psychological approaches to behavior change for improved plaque control in periodontal management. Journal of clinical periodontology. 2015;42(S16):S36-S46.
13. Tolin DF. Is cognitive-behavioral therapy more effective than other therapies? Meta-analytic review. Clinical Psychology Review. 2010.
14. Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632.
15. Miller W, Rollnick S. Motivational Interviewing: Helping People Change. New York: Guilford Press; 2013.
16. Mitchell SH, Overman P, Forrest JL. Critical thinking in patient centered care. Journal of Evidence Based Dental Practice. 2014;14:235-239.
17. Elwyn G, Frosch D, Thomson R, et al. Shared decision making: A model for clinical practice. Journal of General Internal Medicine. 2012;27(10):1361-1367. doi:10.1007/s11606-012-2077-6.
18. The SHARE Approach. September 2015. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/professionals/education/curriculum-tools/shareddecisionmaking/index.html. Accessed January 23, 2016.