By Nancy W. Burkhart, BSDH, EdD
Neoplasia refers to an uncontrolled growth of tissue or cells not under physiologic control that may be either malignant or benign. A tumor is a swelling or an enlargement. The classification of neoplasia and tumors sometimes overlaps. The differentiation is very subtle in some instances clinically and only discerned by microscopic examination.
Figure 1: Clinical view of peripheral ossifying fibroma
Courtesy of Drs. Jordan McHone and David Klingman
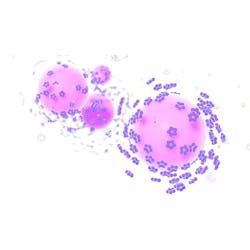
Figure 2: Pyogenic granuloma:
Courtesy of Drs. Michael Poth and David Klingman
Such is the case with the peripheral ossifying fibroma. The peripheral ossifying fibroma consists of disbursed segments of calcified material that is probably from the periodontal ligament or periosteum. The etiology and the treatment modality is very different when compared to the pyogenic granuloma.
The two represent very distinct histological characteristics but at times may display very similar clinical appearances while in certain stages of development. The pyogenic granuloma (PG) may become more fibrotic as the lesion ages, making it clinically resemble the peripheral ossifying fibroma (POF). The pyogenic granuloma often appears red and ulcerative and bleeds. The same can be true for the POF because they can become traumatized and may bleed.
The clinical differentiation is often puzzling to the dental practitioner, and the definitive diagnosis is not realized until the tissue is viewed under the microscope or, perhaps in the case of the pyogenic granuloma, when the tissue begins to recede on its own. In many cases, the PG may become somewhat fibrotic and decrease in size.
PERIPHERAL OSSIFYING FIBROMAS
These fibromas are seen in soft tissues of the gingiva. The incisor-cuspid area is often favored, extending into the interdental papilla areas of the maxillary arch. The growths present as either sessile or pedunculated. They tend to occur on the gingiva, predominately in young adults and women. Histological examination reveals cellular fibroblasts and connective tissue strands with islands of calcified material and cementoid-like material (odontogenic).
Bharathi et al., in a recent article, presented descriptions of four cases of gingival overgrowth. The authors state that the cementoid material found in a POF may be due to the presence of epithelial cell rests of Malassez promoting odontogenic epithelium (see Figures 1, 2). Ashok et al. (2016) make the point that some authors believe that the cells ultimately lead to the formation of bone by metaplasia.
Others believe that the POF is a continuation or extension of the pyogenic granuloma and that it merely represents a matured form of the PG. The peripheral odontogenic fibroma is classified in a separate category by the World Health Organization and is considered a tumor. Also, the demographics include populations across a wide age range.
PYOGENIC GRANULOMA
The pyogenic granuloma is a solitary growth that is inflammatory in nature and produces exuberant tissue responses to trauma or local irritation. At one time, the PG was thought to be related to an infection, and to be caused by pyogenic organisms. The growth does have numerous blood vessels and inflammatory cells present. However, there are no "pus" producing characteristics. It is a common reactive type of lesion. Some other names for this lesion when found in pregnant women are pregnancy granuloma, pregnancy tumor, or pregnancy epulis, and epulis gravidarum.
The lesion is often noted during pregnancy because of the high increase in certain hormones present during this time, since the rate of growth is accelerated during pregnancy. Although some names of these growths use the word "tumor," they are not tumors. The PG is a reaction to foreign body material such as calculus, food debris, or possibly an overhanging dental restoration.
Since these growths occur in exposed areas, they are often traumatized, highly vascular, and the surface area may present with bleeding or bright redness. The increase in capillaries and hyperplastic tissue cause the red color and increased size. The young pyogenic granulomas are usually very vascular and red, but the granuloma may become more fibrotic and more flesh-colored with age. When pyogenic granulomas occur during pregnancy, they tend to shrink or diminish altogether after common hormonal changes decrease. The PG is found on the gingiva in over 75% of cases, measuring anywhere from a few millimeters to a centimeter or more. The PG may also be found on the tongue, lips, and buccal mucosa. The anterior maxillary region is the most favored location.
TREATMENT
The PG associated with pregnancy will usually diminish after hormones normalize, and all irritation-producing causes are removed. Surgical excision is needed for any PG lesions that do not subside or those suspected of being another type of enlargement.
The treatment is more aggressive with regard to the POF type of lesions when compared to the pyogenic granuloma. The removal of these is problematic since all components of the periodontal ligament and surrounding space must be removed. Sometimes defects in bone may result due to the amount of tissue removed. Removal down to the periosteum is standard practice to prevent recurrence (Neville et al. 2016). If any fragments remain, the occurrence rate is high. Reports of using the diode lasers are mentioned by some authors and said to produce less bleeding with better healing.
Differential diagnosis: Most gingival enlargements and infections may exhibit similar characteristics and must be considered in a differential diagnosis as well. Most localized gingival overgrowths are categorized into the following types of lesions seen clinically:
- Neoplasms/tumors
- Infections
- Fibromas (irritation fibroma)-most common fibroma
- Peripheral ossifying fibromas
- Pyogenic granulomas
- Peripheral giant cell granulomas
- Giant cell fibroma
- Peripheral odontogenic fibromas
As always, continue to listen to your patients and always ask good questions. RDH
References
1. Ashok S, Gupta AA, Ashok KP, Mhaske SA. Peripheral ossifying fibroma: A rare case affecting maxillary region. Indian J Dent. 2016 Sept; 7(3), 141-143. http://doi.org/10.4103/0975-962X.186701.
2. Baiju CS, Rohatgi S. Peripheral odontogenic fibroma: A case report and review. Journal of Indian Society of Periodontology. 2011; 15(3):273-275. doi:10.4103/0972-124X.85674.
3. Bharathi DR, Sangamithra S, Arun KV, Kamar TSS. Isolated lesions of the gingiva: A case series and review. Contemp Clin Dent. 2016 Apr-Jun; 7(2): 246-249.doi: 10.4103/0976-237X.183053.
4. Buchner A, Merrell PW, Carpenter WM. Relative frequency of central odontogenic tumors: A study of 1,088 cases from Northern California and comparison to studies from other parts of the world. J Oral Maxillofac Surg. 2006; 64:1343-52. [PubMed].
5. DeLong L, Burkhart NW. General and Oral Pathology for the Dental Hygienist. 2nd ed. Lippincott Wolters Kluwer, Williams & Wilkins. Baltimore 2013.
6. Neville BW, Damm DD, Allen CM, Chi AC. Oral and maxillofacial pathology 4th ed. Philadelphia: Elsevier; 2016.; pp.678, 483.
NANCY W. BURKHART, BSDH, EdD, is an adjunct associate professor in the department of periodontics/stomatology, College of Dentistry, the Texas A&M Health Science Center, Dallas, Texas. Dr. Burkhart is founder and cohost of the International Oral Lichen Planus Support Group (dentistry.tamhsc.edu/olp) and coauthor of General and Oral Pathology for the Dental Hygienist. She was awarded a 2016 American Academy of Oral Medicine Affiliate Fellowship from the AAOM. She was a 2006 Crest/ADHA award winner. She is a 2012 Mentor of Distinction through Philips Oral Healthcare and PennWell Corp. Nancy can be contacted at [email protected].