The AMSA nerve block: Pair with the PSA nerve block for hemimaxillary anesthesia
By Laura Webb
The anterior middle superior alveolar (AMSA) nerve block was discovered by Friedman and Hochman during the development of a computer-controlled local anesthetic delivery (CCLAD) device in 1997.1,2 The AMSA block has been important to esthetic dentistry because its palatal approach eliminates anesthesia to the soft tissues of the upper lip and face, which facilitates accurate assessment of smile and lip lines during esthetic procedures.1,3,4
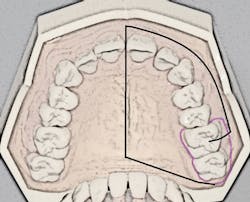
The porous palatal tissue and bone allow penetration of the anesthetic to the dental plexus of the ASA and MSA nerves (on one side), which provide innervation to pulps of the premolars through incisors and, sometimes, the mesiobuccal root of the first permanent molar. The same-side hard palate and palatal gingiva are also anesthesized (see Figure 1).
Globally, dental hygienists have found the AMSA block a very useful and safe injection for nonsurgical periodontal therapy (NSPT) procedures, and it continues to increase in popularity because it provides profound anesthesia to the pulps, periodontium, and gingival tissues for areas usually covered by four individual injections:
- Anterior superior alveolar (ASA)/infraorbital (IO)
- Middle superior alveolar (MSA), if needed
- Greater palatine (GP)
- Nasopalatine (NP) nerve block
A 2014-15 survey conducted by the author revealed that 35% of dental hygiene education programs surveyed in the United States (43 states represented) required clinical competency for the AMSA block. It is expected that this number will increase.
Until the AMSA block was introduced, only the technique-sensitive V2 maxillary nerve block injection was available for providing widespread maxillary anesthesia with fewer than four injections. Many hygienists have avoided the V2 injection because of the technique issues associated with the palatal approach and the high aspiration rate associated with the high-tuberosity approach.
Recall that the posterior superior alveolar (PSA) nerve block, with its 95% success rate, anesthetizes the molar teeth and associated buccal soft tissues. The ability to anesthetize an entire maxillary quadrant (hemimaxilla) during NSPT with the AMSA and the user-friendly PSA block combination (see Figure 1) results in a reduction of the total number of injections (two versus four to five) and also a reduction of total volume of anesthetic (1.25 to two cartridges versus two to three cartridges). Patients appreciate the reduced number of penetrations as well as the lack of numbness of the lip and face.
The main disadvantage of the AMSA-PSA combination is the slow administration time required (three to four minutes) for the AMSA block1,5 (see Table 1).
AMSA technique
General techniques1-6 for palatal injections, including the use of topical anesthetic, pressure anesthesia, pre-puncture technique, and provision of an anesthetic pathway are commonly used. But advancement and deposition should be at a much slower rate.
- Needle selection: A 27-gauge short needle is most commonly recommended, but a 30-gauge extra-short needle has also been suggested for use for this injection due to the short advancement to the palatal bone at the injection site (apices of maxillary premolars).1,4 Many experts suggest that the AMSA is more easily, reliably, and comfortably performed by a computer-controlled local anesthetic delivery (CCLAD) device, which precisely regulates pressure and volume ratio of anesthetic solution delivered.1-6 However, other clinicians feel that this injection can be successfully administered with use of a conventional aspirating dental syringe. Hygienists who have participated in the author’s local anesthesia courses have subsequently experimented with the AMSA in their offices and reported that they had excellent success and were very comfortable using a conventional aspirating syringe.
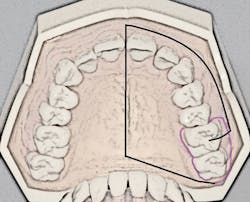
- Insertion site: The insertion site is located midportion of the anterior palate, approximately halfway along an imaginary line connecting the median palatal raphe (tissue overlying the palatal suture) and the palatal free gingival margin between the premolars1,3,4 (see Figure 2).
- Topical anesthetic: Although the use of topical anesthetic may be controversial for palatal injections due to the keratinized nature of the hard palatal tissue, the author suggests that taking the time to let the topical anesthetic do its job is worth the wait.
- Pressure anesthesia: Place a cotton swab (avoid the use of a mirror handle as it can be very uncomfortable for the patient) with very firm pressure next to the insertion site to increase patient comfort and maintain the pressure during the entire process of advancement and deposition and briefly after deposition.
- Pre-puncture technique: With the bevel facing the tissue, at the insertion site, bow the needle slightly, and express a few drops of anesthetic on top of the tissue, just prior to penetration.
- Anesthetic pathway and deposition: Straighten the needle, position the angle at 45-degrees to the tissue, penetrate, and advance very slowly, depositing drops of agent ahead of the needle, creating an “anesthetic pathway” for a more comfortable injection. After initial blanching, it is also recommended to pause for several seconds to facilitate the anesthetic pathway. Advance until bone is gently contacted (4-7 mm). Often, the depth of penetration will be only the length of the needle bevel. Deposit, after negative aspiration, 1.4-1.8 mL of anesthetic over a minimum of three minutes (0.5 mL/minute).1,3,4 Observe for light blanching as this is an indication that tissues are reaching their saturation point. Pausing every 1-2 mm during advancement and slowing anesthetic flow when blanching is observed during deposition allows the agent to diffuse through tissues and helps to deter excessive blanching, which can result in postoperative pain or necrosis.4
Special considerations:
- When pairing the AMSA and PSA blocks to achieve quadrant anesthesia, the PSA should be given first and debridement should begin from the molars toward the central incisor.
- Failure of anesthesia is most often related to inadequate depth or volume of anesthetic.
- Additional anesthesia may be needed for centrals and laterals due to overlapping fibers of the contralateral ASA nerve.1,3,4
- Some experts recommend reducing the dose of 4% anesthetics to 0.9 mL over a three-minute period. However, at least one study has shown that this may not be necessary (Malamed, 2013; Stenver, 2011; Pharmacovigilance Working Party of the European Union).4
- Thin palatal tissues may not accommodate the anesthetic solution well. Basset et al. discuss the importance of selecting a penetration site with adequate tissue thickness so that the agent is accommodated and diffuses efficiently. Select an adjacent site if necessary.4
- Excessive blanching (usually associated with use of 1:50,000 epinephrine) may result in ulcerative lesions that are often associated with palatal injections. This has occurred more often with use of a conventional syringe.
- Hand fatigue may be avoided with use of a smaller, lighter, “petite” style syringe or the CCLAD.
Efficacy
In the past, there have been some conflicting studies regarding the depth and duration of pulpal anesthesia as well as the adequacy of hemo stasis for NSPT even with the use of the CCLAD.6 However, more recent studies as well as recent reports from hygienists, have shown that - with proper technique - profound anesthesia, adequate hemostasis, and appropriate duration of anesthesia are readily achieved.1,4,5 The AMSA is an important addition to the dental hygienist’s repertoire of injections for NSPT. Alone, it provides reliable, profound, intermediate-duration local anesthesia to a wide area of the maxilla usually requiring several injections. Paired with the PSA, the entire maxilla on one side may be anesthetized with only two injections. Reducing the number of penetrations saves time and improves patient comfort and acceptance. The reduction in total volume of anesthetic facilitates the provision of safe doses of anesthetic and vasoconstrictor. The added benefit of not anesthetizing the lip and face also improves patient acceptance. Complications associated with AMSA injection are rare and are related to those common to conventional palatal injections. As with all injections, following proper technique protocols is key to safe and reliable administration. RDH
References:
1. Malamed S. 2013 Handbook of Local Anesthesia 6th ed; Elsevier.
2. Perry D, Loomer P. Maximizing pain control: the AMSA injection can provide anesthesia with fewer injections and less pain. Dimensions of Dental Hygiene Apr/May 2003; 1 (2): 28-29, 32,33.
3. Logothetis D. 2017 Local Anesthesia for the Dental Hygienist, 2nd ed; Elsevier.
4. Bassett K, DiMarco A, Naughton D. 2015 Local Anesthesia for Dental Professionals, 2nd ed; Pearson.
5. Patel JJ, Asif K, Aspalli S, Gururaja Rao TR. New anesthetic technique in periodontal procedures. J Indian Soc Periodontol 2012;16:253-5.
6. Logothetis D, Fehrenbach M. Local anesthesia options during dental hygiene care. RDH June 2014; 34(6).
LAURA J. WEBB, RDH, MS, CDA, is an experienced clinician, educator, and speaker who founded LJW Education Services (ljweduserv.com). She provides educational methodology courses and accreditation consulting services for allied dental education programs and CE courses for clinicians. Laura frequently speaks on the topics of local anesthesia and nonsurgical periodontal instrumentation. She was the recipient of the 2012 ADHA Alfred C. Fones Award. Laura can be contacted at [email protected]