What's Depth Got To Do With the Great Barrier Leak?
As a former SCUBA diver, I always wanted to visit the Great Barrier Reef. Perhaps I will someday. For now, my exploring is limited to the depths of periodontal pockets and the repair of leaks.
"So… how many leaks do I have today?" That was the main question on my patient Ron's mind as I set down my probe and my assistant, Sudy, began to count his bleeding points. Sudy and I both exploded with laughter. We had never thought of bleeding on probing as springing leaks, but there it was! Little did Ron know just how close to the truth his comment was.
How many times have you removed your curette from below the gingival margin to have it followed by a tiny clear tag of tissue? This clear little tissue tag is the epithelial lining of the sulcus or pocket — a lot like the lining of a Doughboy pool. It acts as a barrier between the world above and below. Ever wonder why it is clear? Because there is no blood supply in the epithelial lining. The blood supply is in the underlying connective tissue that, in health, is protected by the great barrier like epithelial lining.
A frequent question posed by dental professionals is, "Do antithrombolytic drugs such as aspirin increase bleeding on probing scores?" The answer is, "In health, no. In the presence of inflammation, yes." Hopefully this article will provide a clear understanding of bleeding on probing, with or without antithrombolytic drugs, by explaining some of the variables of probing and processes affecting the epithelial lining in the absence and presence of inflammation.
In the 1940s, J. Ovanin of Michigan set the pattern of diagnosing periodontal disease on the basis of pockets. He did his master's thesis on whether or not there was collagen unraveling at the apex of junctional epithelium, where the connective tissue's attachment to the root begins. He correlated this with the depth of the attachment. He never saw it at 3 mm, but he did see it at 4 mm.
From this came the idea that up to 3 mm is OK, but 4 mm and above is not good. Just because collagen is breaking down more rapidly at the junctional epithelium doesn't mean it isn't also repairing more rapidly. In this case, there would still be homeostasis.
While the literature indicates that increased probing depths are usually related to loss of clinical attachment, they may not reflect periodontal disease or disease progression.
By Orban's definition, a gingival sulcus is a crevice without disease, even if it is 10 mm deep. Ramfjord would call this deepened sulcus an "anatomical defect." A gingival pocket, on the other hand, is a crevice with disease, even if it is only 2 mm deep.
When characteristics pertaining to deep and shallow sites are compared, deep sites tend to have more bleeding on probing, elevated bacterial levels, reduced ability of oral hygiene to alter subgingival microflora, less effective root instrumentation, and a greater percentage of pockets that experience disease progression in treated and untreated sites.
According to Greenstein, however, individual deep sites are not good predictors of disease progression.
When we probe, we're looking at a historical record of what took place before the patient visited us. How fast did it occur? Several studies have looked at the rate of detachment and concluded that untreated periodontal disease loses attachment at the rate of 0.5 mm per year. The probe only provides a historical record of detachment when measured in the absence of inflammation. It is most important to remember that the almighty probe does lie.
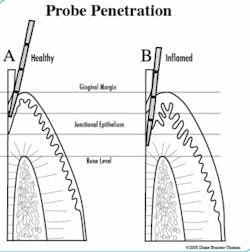
That's right, it lies. According to a recent review by Greenstein, the literature has established that when probing healthy periodontium, the probe tip will usually stop within the junctional epithelium, 0.2 mm to 0.4 mm coronal to the connective tissue insertion into the root. In inflamed pockets, the probe tip will penetrate to extend beyond the apical end of the junctional epithelium 0.3 mm or more into the connective tissue. Robinson and Vitek showed the mean probe penetration with inflammation to be 1.25 mm apical to the connective tissue attachment.
Consider that there are several variables that can affect probe depth penetration: the size of the probe, probe force, rotation of the tooth, and angulation. Self-calibration creates another variable representing a 1 mm standard deviation. This means that if you measure 4 mm, the depth may really be 3 mm, 5 mm, or 4 mm. As you can see, interoperator calibration might also play a role. Regardless, the most important variable of probe penetration is probably the presence or absence of inflammation.
The probe score is a historical record modified by the amount of inflammation present.
If you do a periodontal evaluation on a patient, then put him or her on systemic antibiotics (a tetracycline type, for example) for one week, then rescore at the end of that week, you will find that previously deeper pockets (like 7 to 8 mm) will have decreased by 2 to 4 mm.
Probe scores are meaningless unless you have a baseline from the first probe with inflammation, and where you probe without inflammation, to give you a guesstimate of the length of the junctional epithelium. For example, you may probe 8 mm with inflammation and 4 mm without inflammation. The junctional epithelium, then, is probably about 4 mm. Junctional epithelium generally varies from 0.5 to 8 mm.
We tend to get upset if a pocket probes 7 mm, but we must realize this is temporary inflammation. Get the inflammation down. The patient hasn't really lost all that attachment, you're just probing beyond the bottom of the pocket and penetrating into the connective tissue. Probe scores reflect where the probe stops, not where the pocket is. Reduce the inflammation and probe a second time.
Some use bacteriologic testing or microscopic evaluation of the presence of motile bacteria or white blood cells to determine the presence of infection or assess risk. Others rely on the "old standard" bleeding on probing scores to determine if disease is present now, and recognize that bleeding on probing is not a good indicator of future destruction. This isn't to say there is no bacteriological risk, but if the tissue does not bleed when probed, chances are the sulcular epithelium is sufficiently intact. If the tissue does bleed when probed, you penetrated through the epithelial attachment into the underlying connective tissue, which is vascular. That's why it bleeds. It may or may not be previously ulcerated.
Think about the sulcular epithelium in a healthy periodontium. The sulcular epithelium consists of very busy epithelial cells, stuck together with an intercellular substance we'll call "cell glue." This cell glue is made of protein polysaccharides, which are long chains of protein and sugars. The cell glue is manufactured in the cytoplasm of each cell, and exported across the cell membrane to create the bonding from cell to cell and from the basal cells to the underlying connective tissue. If the epithelial cells do not manufacture cell glue, they cannot stick together. If they cannot stick together, they cannot stop the probe from penetrating into the connective tissue.
It is the availability of nutrients and the health of the cytoplasm of the cells that determine the ability of the epithelial cells to manufacture the intercellular proteins, hyaluronic acid, and chondroitin sulfate. The biochemical process by which nutrients are moved from the blood supply, across the cell membrane, and into the cytoplasm of the cell is called "active transport." Active transport will not work without protein polysaccharides between the cells. If the cells do not have the nutrients, the protein of the cytoplasm will become denaturized. This is called hyaline degeneration, and once it occurs, it prevents the normal function of cytoplasm and, ultimately, the cell dies.
This is important to understand because to make matters worse, certain bacteria have the capacity to deliver the enzymes hyaluronidase and chondroitin sulfatase, which break down the intercellular proteins of the cell glue between epithelial cells. Bacteria have been identified in the gingiva, within the intercellular spaces of the epithelial tissue, in the connective tissue, and lying on the crest of the alveolar bone. These enzymes effectively break down the intercellular material. Therefore, the bacteria can interfere with the active transport of nutrients.
So, if there is a high microbial mass, there is an increased likelihood of shedding epithelial cells due to the destruction of intercellular material and interference with active transport, and the integrity of the epithelial lining is lost. The epithelial cells can no longer stick together, so the probe penetrates the epithelial barrier and the connective tissue. Clinically, we see bleeding on probing.
So what about the patients on antithrombolytics such as aspirin?
In the Journal of Periodontology, 2002, Schrodi, Recio, Fiorellini, Howell, Goodson, and Karimbux published a study which resulted in a moderate, yet statistically significant increase in bleeding on probing found in patients with greater than or equal to 20% bleeding sites during their initial visit, prior to aspirin exposure (325 mg) for seven days. However, there was no significant difference between the placebo group and those on 81 mg aspirin for seven days. In addition, the tendency to bleed on probing was not significant in the groups, which exhibited less than 20% bleeding sites during the visit prior to exposure.
It is therefore apparent that if the patient had inflammation to start with, the aspirin increased bleeding. It bleeds more because the probe penetrates the epithelium into the vascular connective tissue, and because the anti thrombolytic activity of the aspriin increases clotting time. If the epithelial lining was healthy and intact to start with, the aspirin did not increase the bleeding, primarily because the probe did not penetrate the barrier of the epithelial lining of the sulcus.
As inflammation is reduced, the great barrier leaks are repaired, and we find ourselves in the shallows of periodontal health. It may not be as exciting as SCUBA diving, but at least there aren't any sharks in that paradise!
About the Author
Diane Brucato-Thomas, RDH, EF, BS, founder of the Hawaii Institute for Wellness in Dentistry, was a periodontal therapist for nearly three decades, and also served as Clinical Specialist for DentalView, Inc.; Anesthesia Examiner for the WREB; Recorder for Hawaii BDE; Advanced Clinical Instructor at Northern Arizona University. Diane is active in ADHA and American Academy of Dental Hygiene, and holds membership in American Association of Dental Examiners and Western Society of Periodontology. Diane was twice awarded "HDHA Outstanding Member" and was first recipient of the "Rosie Wall Community Spirit Grant." She was also among the first recipients of the Sunstar GUM / RDH Magazine Healthy Gums, Healthy Life Award of Distinction. A speaker and published author, her writings have appeared in the Journal of Practical Hygiene, Chicken Soup for Soul: A Fourth Course and Love is the Best Medicine: for Dental Patients and Dental Teams, for which her short story shared Grand Prize.