Maximizing surface esthetics
by Laurence J. Walsh, PhD. DDSc
With the current strong levels of interest by patients in reducing the aging-related yellow shades within their teeth by bleaching, it is surprising that greater attention has not been directed to other means of reducing yellowness. This paper looks at the concept of "tooth lightening" using simple in-office and supporting at-home measures, as opposed to "tooth whitening" using peroxides.
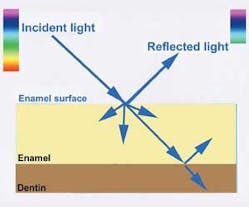
The concept is based on exploiting a number of well-established optical properties of teeth, enamel and water under visible light conditions. These are presented step-wise in Tables 1-3 and the accompanying Figures 1 and 2. The scientific foundations of the tooth lightening concept rest largely on altering the short wavelength (blue) scatter of enamel and reducing its transmission of yellow light, although there are minor accompanying changes such as reduced red absorption which also occur.
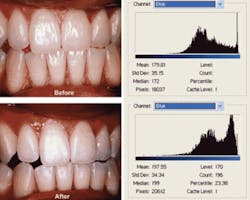
The clinical stages in tooth lightening are as follows. First, the reflection of light and the backscatter of the shorter wavelengths of light are enhanced by a gentle microabrasion procedure using 37% phosphoric acid etching for 20 seconds followed by gentle application of flour of pumice or graded abrasive pastes at low rotational speeds. The etching step enhances subsequent subsurface mineral changes. Patients then apply GC MI Paste Plus™ [Tooth Mousse Plus™]each night immediately before bed for at least two weeks. The reduced yellow transmission and increased backscatter of blue light from the enamel will cause a subtle reduction in yellow.
The procedure can precede in-office or at-home whitening treatments, to establish optimal enamel properties and esthetics, or can follow other cosmetic treatments. Two typical cases are shown in Figures 3 and 4. A variety of surface polishing agents can be used to maximize reflectivity without losing the natural surface contours.
Table 1Optics of Human Teeth
• The light that penetrates the surface of a tooth and enters it is refracted due to the fact that light travels faster in air, than in water or in solid apatite materials.
• Tooth color is determined by the paths of light inside the tooth, and attenuation of light along those paths.1
• Colors of natural teeth have a wider range (greater color space) than represented on existing shade guides;2,3 however, yellow is the base color which causes the greatest distress when patients are asked to rate their own tooth color. The human eye is more sensitive to green and yellow light than to blue or red — because of the numerical difference in cones (color photoreceptors).4
• Both reddish and yellowish colors of natural teeth tend to increase from the incisal to cervical area, whereas translucency decreases. The middle and incisal thirds are the most visible during speech and in normal function, and thus yellowness here attracts the greatest attention.5
• While a significant yellow fluorescence emission is excited from enamel under visible blue or ultraviolet lighting conditions, this makes little contribution to the perceived color of natural teeth under normal "white light" lighting conditions.1
• Attenuation of light within the tooth is caused by several different factors, but primarily by scattering and absorption. Scattering of light disperses it, without changing the wavelength. Scattering can be forward or backwards in direction.
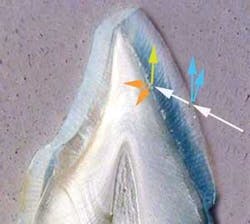
• Light is transmitted through enamel and dentin to the pulpal surface, with the light following the path of the enamel prisms and dentinal tubules. Enamel and dentin together collect and distribute light within the tooth.6
• Light bends when it moves through dentin, in other words, dentin is optically anisotropic. Moreover, light propagation in human dentin exhibits a strong directional dependence.
• It was originally thought that both enamel prisms and dentin tubules acted as optical fibers;6 however, it is now well established that the tubular structure is the predominant cause of scattering in dentin.7,8
• Multiple scattering events occur within the dentin tubules due to their cylindrical structure (and to a lesser extent by peritubular collagen fibers), and not by fiberoptic effects, as had been previously assumed.9-12
Table 2Optics of Human Enamel
• Absorption of light by human enamel is low. In enamel, the organic (protein) component, mostly aromatic amino acids, is responsible for most or all of the limited absorption which occurs.13
• Yellow and red light are highly transmitted by normal enamel, and thus can both reflect from the dentin-enamel junction and transmit back through enamel to the surface.14
• Scattering of light by enamel is high. This is critical, since while tooth color is determined mainly by dentin, enamel plays a significant role in modifying tooth color by scattering the shorter wavelengths in the visible blue range.1
• Reflectance of light from the enamel surface increases linearly from 400 nm (blue) through to 600 nm (red).1
• Shorter wavelengths of visible light (blue and violet) have a much higher scatter coefficient than longer wavelengths (yellows and reds). This is why visible blue and violet wavelengths in the non-dental environment cause dazzle effects in rain, fog and snow, and cause problems with glare.
• In enamel, it is the hydroxyapatite crystals themselves which contribute significantly to scattering, rather than the prism structure.7,8 For this reason, dissolution of crystallites or their incomplete formation will affect the scatter of light.
• The more porous the enamel, the less it scatters short (blue) wavelengths of light. The more the enamel scatters blue light, the lighter it appears.1
Table 3The Influence of Water Present in the Enamel
• Enamel contains 7-10% water by volume as one of its normal constituents, and this water affects its ability to both absorb and scatter light.
• For early carious lesions and other enamel conditions with increased subsurface water, longer wavelengths of yellow and red are preferentially reflected back to the surface. This radiance change is mainly determined by the lack of mineral and the increased water content in these lesions.7,8
• Even without the development of white spot lesions or altered enamel formation, microscopic subsurface water voids are common as enamel is never perfectly mineralized. These water rich areas can undergo subsurface remineralization by repeated topical application of CPP-ACP (Recaldent™) products such as GC MI Paste Plus.15,16
• Restoring mineral to these water rich areas should, therefore, change the scatter of short wavelengths of light and thereby alter the appearance and color of the enamel surface.
• Micropolishing the enamel surface makes tooth shade lighter and less yellow, and this effect is enhanced upon air-drying, which removes subsurface moisture.17
• This provides a rationale for micropolishing in combination with subsurface remineralization.
Editor's Note: This article was originally published in the March/April 2008 issue of Australasian Dental Practice.
About the Author:
Professor Laurence J. Walsh is the technology editor of Australasian Dental Practice magazine. He is also a noted commentator on and user of new technologies and is the Head of The University of Queensland School of Dentistry.
References
1. Bosch JJ, Coops JC. Tooth color and reflectance as related to light scattering and enamel hardness. J Dent Res. 1995; 74(1):374-80.
2. Schwabacher WB, Goodkind RJ. Three-dimensional color coordinates of natural teeth compared with three shade guides. J Prosthet Dent. 1990; 64(4):425-31.
3. Guan YH, Lath DL, Lilley TH, Willmot DR, Marlow I, Brook AH. The measurement of tooth whiteness by image analysis and spectrophotometry: a comparison. J Oral Rehabil. 2005; 32(1):7-15.
4. Kennedy D, Milkman RD. Selective light absorption by the lenses of lower vertebrates, and its influence on spectral sensitivity. Biol Bull 1956; 111(3):375-86.
5. Hasegawa A, Ikeda I, Kawaguchi S. Color and translucency of in vivo natural central incisors. J Prosthet Dent. 2000; 83(4):418-23.
6. Odor TM, Watson TF, Pitt Ford TR, McDonald F. Pattern of transmission of laser light in teeth. Int Endod J. 1996; 29(4):228-34.
7. Vaarkamp J, ten Bosch JJ, Verdonschot EH. Propagation of light through human dental enamel and dentine. Caries Res. 1995; 29(1):8-13.
8. Vaarkamp J, ten Bosch JJ, Verdonschot EH. Light propagation through teeth containing simulated caries lesions. Phys Med Biol. 1995; 40(8):1375-87.
9. Kienle A, Forster FK, Diebolder R, Hibst R. Light propagation in dentin: influence of microstructure on anisotropy. Phys Med Biol. 2003; 48(2):N7-14.
10. Kienle A, Forster FK, Hibst R. Anisotropy of light propagation in biological tissue. Opt Lett. 2004; 29(22):2617-9.
11. Kienle A, Michels R, Hibst R. Magnification - a new look at a long-known optical property of dentin. J Dent Res. 2006; 85(10):955-9.
12. Kienle A, Hibst R. Light guiding in biological tissue due to scattering. Phys Rev Lett. 2006; 97(1):181-4.
13. Spitzer D, Bosch JT. The absorption and scattering of light in bovine and human dental enamel. Calcif Tissue Res. 1975;17(2):129-37.
14. Odor TM, Chandler NP, Watson TF, Ford TR, McDonald F. Laser light transmission in teeth: a study of the patterns in different species. Int Endod J. 1999; 32(4):296-302.
15. Walsh LJ. Tooth Mousse: Anthology of applications. Singapore, GC Asia Dental, 2007.
16. Walsh LJ. White spots. Singapore, GC Asia Dental, 2007.
17. Kleber CJ, Putt MS, Nelson BJ. In vitro tooth whitening by a sodium bicarbonate/peroxide dentifrice. J Clin Dent. 1998; 9(1):16-21.