Oral cancer is a soft-tissue condition, and it"s something we can prevent. With an armamentarium that includes loupes, light, fluorescence, and the BrushTest, treating a dysplasia is easier than keeping up with cancer treatments and all that they encompass. Minimal intervention in detection of soft tissue issues is best for the patient. It turns out that we can take more professional responsibility in preventing oral cancer.
by Shirley Gutkowski, RDH, BSDH, FACE
Sometimes people get trapped into thinking that minimal intervention is all about teeth or enamel. It's not. Take oral cancer, for instance. It's a soft-tissue disease — well, condition. It's also something we can prevent. When oral health-care providers read a statement like that, they usually go into autopilot thinking. Ways of convincing patients to stop smoking, how to get a straight answer about excessive drinking, and what to do if they do both, fly through the head as preventive measures for oral cancer. Not so, mes amis.
It turns out that we can take more professional responsibility in preventing oral cancer. In the news over the last couple of years, the use of chemiluminescence and fluorescence have been all the talk. Before doing that, though, a traditional palpation and visual screening examination are necessary. The one component of the traditional exam that is often missing is telling the patient/client what you are doing. It seems that oral health-care professionals are very squeamish about all aspects of oral cancer. Hurdles include things like finding it. And it's never a good day when we find cancer.
Patients, on the other hand, expect us to look for cancer and if we find something, they expect we'll do something about it such as refer them to an oral surgeon. So, we need to tell patients that we are performing an oral cancer exam. On occasion, patients will call the office and say they don't want an oral cancer exam. While perplexing, they may cancel their appointment because they think the exam costs extra. This is most often a communication problem that originates with the practitioner. Don't blame your patients. The fastest growing population segment with oral cancer is people under 40 with no traditional risk factors, and the treatment isn't much better than the disease (Oral Cancer Prevention International).
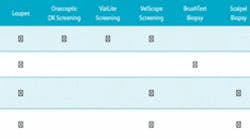
After the traditional exam, one of the screening light systems may be beneficial. The chemiluminescent light from ViziLite or the reuseable Orascoptic DK can help illuminate problems that aren't already easily visible with the use of loupes and a headlight. The VelScope may be helpful in cases where the tumor already has an ample blood supply.
Cancer starts as an aggregation of mutated cells in the epithelium less than half a millimeter under the surface. This aggregation of cells is called a dysplasia; it can be seen with the naked eye and seen well when wearing loupes. The dysplasia can look white, red, or mixed. A large study of thousands of mouths tells us that 10 percent of patients will have some kind of spot with unknown etiology. In terms of a typical dental hygiene day of eight to 10 patients, nearly once a day someone will present with some kind of small, common spot. Four percent of those common spots in the study were found to be dysplasia.
The dysplasia is easy to remove because it's in the epithelial layer before it gets into the basal layer where the blood supply is. Once removed, the cancer has been averted or prevented. The best test for this is the BrushTest (OralCDx). Many states allow dental hygienists to do the BrushTest as part of their scope of practice as directed by the dentist or even as part of the practice's standing orders. Simple twisting of the brush with pressure and swabbing the sample onto a slide — like we all did in school — and preparing it and sending it off to the lab is all that's necessary to sample.
So once per day, the studies tell us, a patient with a common oral spot will present to a hygiene appointment. If it's one of the 4 percent of spots that is dysplasia, it can be removed from that thin epithelial layer. These numbers can really help when speaking to patients, too — telling them they have a common oral spot that you see every day, and that your practice brush tests every common oral spot; explaining that if the cells are abnormal, a 4 percent chance (same as abnormal results of the 50 million PAP smears in the United States), the spot can be removed with little trauma. Left alone, there's a small chance that the cells could continue to change, and the change isn't good.
The same can be said for masses that turn up under the light systems. While a positive VelScope may mean a referral for a scalpel biopsy because of the nature of the finding, a positive ViziLite or DK finding likely warrants a BrushTest. ViziLite Plus comes with a proprietary dye called TBlue, which highlights abnormal cells raising the cancer concern. A BrushTest will be unaffected by the dye, so there's no worry there.
Once the slides are scanned by a computer and reviewed by a pathologist, a report is sent to the dentist. One of the new aspects to the report is a personal phone call from the company dentist when the report is not totally straightforward.
The discussion on early cancer detection cannot be complete without a mention of HPV. Human papillomavirus (HPV) is a sexually transmitted disease. It is the known cause of cervical cancer, and less known for causing anal cancer, and now oral cancer. If you think it's hard talking to patients about cellular changes that may be cancer, how do you talk to a 14-year-old kid about oral sex and the unwanted consequences of which include disfiguring oral surgery? HPV in oral cancer manifests in different locations than traditional oral cancer. What makes it so difficult is that it is often in the crypts of the tonsils, on the posterior third of the tongue, and most commonly in the throat. Discussions are ongoing about offering the HPV vaccine to all early adolescents, not just girls
Minimal intervention in detection of soft tissue issues is easy and best for the patient. The armamentarium of loupes, light, advanced tissue lighting or fluorescence, and the BrushTest is the best for your patients. Treating a dysplasia is so much easier than keeping up with cancer treatments and everything that goes along with that.
About the Author
Shirley Gutkowski, RDH, BSDH, FACE, is a practicing dental hygienist from Sun Prairie, Wis. The Purple Guide: Developing Your Clinical Dental Hygiene Career by Gutkowski and Nieves is available at www.rdhpurpleguide.com. An international speaker and award-winning writer, Gutkowski can be reached at [email protected].