BY NOEL BRANDON KELSCH, RDHAP
Nancy Writebol has been described as unassuming and humble. She worked as a medical missionary. She's like many other people I know - willing to make sacrifices in order to give care. For 14 years she and her husband have left the comforts of home and put their lives at risk to serve others, ministering to orphans and vulnerable children in Africa. Last year their journey of service took them to Monrovia, Liberia.
They were quickly faced with life-changing circumstances - the Ebola outbreak in March 2014. They turned down the opportunity to evacuate when Ebola struck. Congressman Robert Pittenger stated, "They could have chosen the easy route. Instead they chose a higher calling of sacrificial love and service."1
The hospital where they were working became the Monrovia Ebola Consolidated Case Management Center. Nancy volunteered as part of a crisis team. Her role included disinfecting doctors and nurses working with Ebola patients. It is reported that she followed the standards developed by the Centers for Disease Control and Infection (CDC), the World Health Organization (WHO), Liberia Ministry, and other global health authorities.
Within just a few short months, Nancy was diagnosed with the Ebola virus on July 25, 2014. It's not clear at this point how she contracted the disease. Nancy was transported back to the United States using a specially designed transportation system that was developed to contain the disease. Nancy and Dr. Kent Brantly, who also contracted the illness, were later discharged from the hospital, and the CDC reported that the virus is no longer present in their blood. Both survivors are no longer at risk of transmitting the disease. It is believed that the experimental medication that they were given had a major impact.
The CDC has well-established protocols in place to ensure the safe transport and care of U.S. citizens who contract infectious diseases back to the United States. Patients were evacuated in similar ways during the SARS outbreak. The CDC has also implemented screening of travelers and isolation precautions on all flights from infected countries. On July 31, the CDC elevated their warning to U.S. citizens, encouraging them to defer unnecessary travel to Guinea, Liberia, and Sierra Leone due to concerns that travelers may not have access to health-care facilities and personnel should they need them in one of these countries.2 It is important to stay updated on these warnings because they can change daily as the disease spreads from country to country.
What is Ebola?
Ebola is a virus that once contracted leads to viral hemorrhagic fever disease. Symptoms appear anywhere from two to 21 days after contracting the virus. Commonly the symptoms appear in eight to 10 days from exposure. The CDC lists symptoms as fever, headache, joint and muscle aches, weakness, diarrhea, vomiting, stomach pain, lack of appetite, and abnormal bleeding. Patients have also experienced rash, red eyes, hiccups, cough, sore throat, chest pain, difficulty breathing, difficulty swallowing, and bleeding inside and outside of the body. Patients that are asymptomatic are not contagious. In order to get the virus, one must have direct contact with an individual who has symptoms. It is a severe, often fatal disease, with a fatality rate of up to 90%, according to WHO.
How is it transmitted?
The transmission of Ebola is very specific, including direct contact with the blood or bodily fluids of an infected symptomatic person, or through exposure to objects (such as needles) that have been contaminated with infected secretions. It is not a respiratory nor foodborne disease.2 Outbreaks are occurring primarily in remote villages in Central and West Africa near tropical rainforests. The virus is transmitted to people from wild animals (with fruit bats being considered a natural host), or through direct contact with someone who has the disease.
Exposure to Ebola can occur in health-care settings where staff members do not wear appropriate protective equipment such as masks, gowns, and gloves, or where there is a lapse in standard precautions.3 One of the major issues with this disease is that the natural reservoir host of Ebola, and the manner in which transmission of the virus to humans occurs, still remains unknown. This makes risk assessment in endemic areas difficult. With the exception of several laboratory contamination cases (one in England and two in Russia), all cases of human illness or death have occurred in Africa. No case has been reported in the U.S.3
The specific number of cases is still being investigated. The CDC states, "There are ongoing outbreaks across Guinea, northern Liberia, and now eastern Sierra Leone. The number of patients is constantly evolving due to the ongoing investigation."
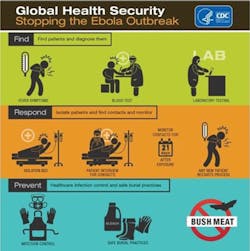
The CDC is on the highest alert (stage 1). This is the largest Ebola outbreak in history. All American health-care workers, including those in dentistry, need to be on the alert for the signs and symptoms of this disease with patients who have traveled within 21 days to where the outbreak is occurring. Patients meeting the criteria should be isolated pending diagnostic testing.5
| Protective Equipment in Developing Countries |
New research from John Hopkins Bloomberg School of Public Health is something all humanitarian projects should reflect on before developing plans to help others. In order to help others, we must first protect ourselves as well as those we are serving. We can do more harm than good if we do not heed that caution. The study showed that basic personal protective equipment that is essential in the prevention of the spread of bloodborne diseases is not available in many of these settings. As we know from experiences in the United States, these situations are not limited to developing nations, and good intentions can lead to doing more harm than good (see www.rdhmag.com/articles/print/volume-33/issue-12/columns/infection-control-and-volunteer-dental-settings.html, or search for "Kelsch Infection Control in Volunteer Settings"). The standard of care in infection control should not change because the setting changes. Cross contamination in these settings could spread the diseases we are trying so hard to eradicate. The current area where the Ebola outbreak occurred was found to have a lack of personal protective supplies. The Journal of Tropical Medicine and International Health revealed that between 2008 and 2013 in Liberia 56% of hospitals had protective eyewear for its doctors and nurses, while 63% had sterile gloves. In Sierra Leone, just 30% of hospitals had protective eyewear, while 70% had sterile gloves. Overall, only 29% of hospitals always had eye protection, 64% always had sterilizing equipment, and 75% always had sterile gloves. The percentage range varied among countries. For example, in Afghanistan, only one-quarter of hospitals had sterile gloves. This is an area where more harm than good could be occurring. In Africa, it is estimated by the World Health Organization that 5% of the population is HIV positive. Serving these clients without proper personal protective equipment is not in the best interest of the patient or the caregiver. These statistics and events are heartbreaking for many and do impact lives. They are also a great opportunity for the future. No outreach program should be conducted without infection control guidelines being adhered to. You should only see as many patients as supplies allow. Every program must have an infection control expert to guide them. Everyone deserves the highest standards of care. |
What do health-care workers need to know?
At this point there are only experimental drugs used for the treatment of Ebola, and no vaccine is available for prevention of the disease. Standard precautions in infection control are a must. Things we take for granted need to happen with every patient, every time! Proper cleaning and disposal of instruments, such as needles and syringes, are also important. If instruments are not disposable, they must be sterilized before being used again. Without adequate sterilization of the instruments, virus transmission can continue and amplify an outbreak.3 If a volunteer program is unable to meet those simple requirements, they should not see patients. The volunteer program could cause more harm than good.
Other than the two Americans who contracted the disease in Africa and were transported to the U.S., there are no cases of Ebola in the United States. Currently the CDC is recommending that people restrict voluntary travel to any country with active Ebola cases.
Resources for treating patients with Ebola and precautions in the medical setting can be found at www.cdc.gov/vhf/ebola/hcp/patient-management-us-hospitals.html. A review of the CDC resources for protecting health-care workers can benefit us all. A great resource in this area is www.cdc.gov/HAI/prevent/ppe.html.
Diagnosis and isolation
Diagnosing Ebola in an individual who has been infected for only a few days is difficult, because the early symptoms, such as red eyes and a skin rash, are nonspecific to Ebola virus infection and are seen often in patients with commonly occurring diseases.4
However, if a person has early symptoms of Ebola and there is reason to believe that Ebola should be considered, the patient should be isolated and public health professionals notified. Samples from the patient can then be collected and tested to confirm infection.3 It is vital to talk to your patients about travel outside the U.S., and to make sure they have no symptoms of any diseases before treating them in the dental setting. RDH
References
1. http://images.sim.org/pdfs/NancyWritebolbio.pdf Accessed 8.6.14
2. http://www.cdc.gov/vhf/ebola/outbreaks/guinea/qa.html Accessed 8.6.14
3. http://www.cdc.gov/vhf/ebola/transmission/index.html Accessed 8.5.14
4. http://www.cdc.gov/vhf/ebola/diagnosis/index.html Accessed 8.6.14
5. http://www.cdc.gov/media/DPK/2014/dpk-ebola-outbreak.html
NOEL BRANDON KELSCH, RDHAP, is a syndicated columnist, writer, speaker, and cartoonist. She serves on the editorial review committee for the Organization for Safety, Asepsis and Prevention newsletter and has received many national awards. Kelsch owns her dental hygiene practice that focuses on access to care for all and helps facilitate the Simi Valley Free Dental Clinic. She has devoted much of her 35 years in dentistry to educating people about the devastating effects of methamphetamines and drug use. She is a past president of the California Dental Hygienists' Association.