By Cynthia Biron Leiseca, RDH, EMT, MA
Want to reduce the workload on your hands during instrumentation? This article reviews current basic techniques and presents new techniques that provide the best leverage and require the least effort and workload on your hands. Some very simple changes to your instrumentation techniques could make major improvements in how your hands feel at the end of a working day.
As dental hygienists, we have repeatedly heard that incorrect patient-operator positioning while performing periodontal instrumentation often leads to cumulative trauma disorders (CTDs). To compensate for the lack of control from incorrect positioning, clinicians not only strain their necks, backs, shoulders, and arms, they also overwork the hands during instrumentation.1 Even the greatest hand skills are compromised when the clinician has to compensate for incorrect patient-operator positioning.
(Review "patient-operator positioning" in the Nield-Gehrig textbook, "Periodontal Instrumentation and Advanced Root Instrumentation," and self-assess your positioning to make corrections before adding new techniques to your instrumentation methods.)
------------------------------------------------------------------------------
See related articles
- A periodontist's protocols to avoid dental implant complications: Part 2 -- establishing an implant maintenance protocol
- Creating the Ultimate Patient Experience Through Technology
- Treating implant gingivitis
------------------------------------------------------------------------------
Many dental hygienists have taken great measures to prevent injury. They purchase loupes to improve positioning, new operator stools, perfectly fitted gloves, new instruments, and they even increase their use of ultrasonic instrumentation. Yet, they still experience pain and may be diagnosed with CTDs such as carpal tunnel syndrome, ulnar nerve entrapment, de Quervain's disease, tenosynovitis, tendinitis, and others.2,3,4
Here is a link to a slideshow of CTDs and physical injuries in dental health-care providers: http://www.slideshare.net/jhpdc/ergonomics-for-dental-hygienists-1178564.
The loupes help with positioning, but they can reduce your tactile sense in subgingival instrumentation.5,6 Tactile sensitivity makes you more astute at determining the need for additional instrumentation strokes. Clinicians who lack fine tactile sense end up making excessive strokes, increasing the workload on the hands. During subgingival instrumentation, clinicians need to focus less on seeing and more on feeling the roots. In their mind's eye, they need to visualize the anatomy of the roots of the teeth as they perform the debridement.26
Ultrasonic instrumentation helps remove tenacious calculus and biofilm, but it presents its own set of problems: hand vibration injuries, hearing impairment, aerosol production, and the fact that it cannot and should not be used on every patient.7,8,9,10 Evidence shows that the best treatment outcome for periodontal patients comes from a combination of hand and ultrasonic instrumentation.11,12 It is also easier on the hands of the clinician to alternate their instrumentation methods by using a combination of hand and ultrasonic techniques.13, 25,26
Predisposing factors to hand injuries
The first place to look when assessing hand or instrumentation problems is at the hands themselves. Physical conditions can be a predisposing factor to hand pain and injury, especially when the hands are placed under the demands of performing periodontal instrumentation.
Joint hypermobility -- The most overlooked predisposing condition is benign joint hypermobility syndrome (BJHS), which may occur in one or more joints of the hands and is a predisposing factor to carpal tunnel syndrome.14,15,16 When there is hypermobility of the joints, the muscles of the hand and arm will be overworked to compensate for the laxity of the joints. With BJHS, it is difficult to apply lateral pressure during the working stroke and then to control the stroke and relax the hand between working strokes.16
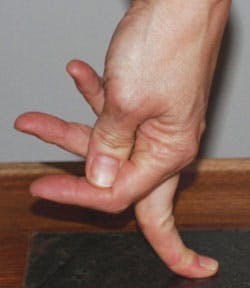
Clinicians who do not self-assess their hands might not even know they have BJHS as it is not a pronounced disfigurement. It can be seen when you press the fingertips against a tabletop and notice the fingers are not straight, as under pressure, one or more fingers are bent at the knuckles. BJHS may be the reason why they struggled when learning the techniques and have pain during and after performing periodontal instrumentation (see Figure 1).
A physician should evaluate a dental clinician who notices joint weakness or hypermobility. The physician may refer the hygienist to an orthopedic hand specialist. Physical or occupational therapy may be prescribed, as well as joint stabilizing devices that can be worn under surgical gloves.16
Osteoarthritis or rheumatoid arthritis -- Various types of arthritis can occur, and the condition may require the hygienist to reduce work hours or leave dental hygiene altogether. An orthopedic hand specialist and/or a rheumatologist can diagnose the type and severity of arthritis and will recommend treatment and exercises.17,18,19 Instrumentation techniques that reduce workload on the hands can make a difference in whether the dental hygienist with arthritis can continue in clinical practice.
Hand weakness -- Hand weakness is determined most accurately through testing by an orthopedic hand specialist who use devices such as dynamometers to test hand strength.20 Hand weakness is more common to female clinicians with small hands, but not to male clinicians with small hands.21 Although anyone could have weak hands, women with small hands are more likely to have weak hands that may be contributing to problems they have with pain associated with periodontal instrumentation. Hand strengthening is beneficial for all clinicians but mandatory for those with weak hands.22, 23
Fingernail length -- Research shows that long fingernails reduce pinch force and hand strength in performing psychomotor tasks. "Long fingernails limit flexion of the finger joints, particularly the metacarpophalangeal joints. Lack of finger flexion will limit excursion of long flexors and extensors in patients. It is recommended that patients cut their fingernails to a length of 0.5 cm to achieve optimal functional outcomes." 24
Leverage is key
Leverage is the key to lightening the workload on the hands, and leverage is dependent on proper equipment and specific instrumentation techniques. Using leverage instead of brute strength and force will prevent overworking the hands. Leverage is maximized with appropriate techniques.25
Proper armamentarium includes an array of periodontal instruments that have large handles (size 10). The instruments must be very sharp to be efficient in latching on to deposits, and this in itself prevents overworking the hands. The hygienist must have a supportive operator stool and a patient chair that goes low enough to allow the clinician to work with the forearms parallel to the floor. A clinician who has to reach up to work on the patient will lose leverage and the ability to control fine hand function in instrumentation.1
Loss of leverage causes:25,26
- Unnecessary tightening of the hands (excessive pinch force)
- Excessive lateral pressure
- Pulling instead of lifting deposits off the teeth
- Unnecessary number of strokes for deposit removal
- Fatigue, pain, injury
Avoid using individual fingers or the thumb to perform instrumentation strokes. Instead use your whole hand as a unit and your arm as a continuum.1 While reviewing a proper grasp may seem too fundamental to the advanced clinician, it is most often the first aspect of instrumentation to be found in error during an observation of instrumentation of experienced clinicians.26
Thumb pulling during the working stroke results in injury due to overuse of the thumb.27,28 It also causes other instrumentation errors such as lack of toe third adaptation of the working end of the instrument to the tooth.25,26
At Boot Camps for Dental Hygiene Educators,26 a simulation lab is used for teaching instrumentation to students who are from area dental hygiene programs. Educators who are attendees in the "boot camp" take part in educator evaluation activities to calibrate on evaluating student clinical performance of periodontal instrumentation. During the evaluation activities, attendees observed students who were activating the instrumentation working stroke by using a thumb pulling motion. Students using a thumb pulling activation tended to lift the toe third off the tooth, which resulted in their using some of the middle third of the blade during the working stroke. Not using the toe third of the blade was less effective and required the students to apply additional lateral pressure to remove the synthetic calculus deposits from the teeth of typodonts.25, 26
To remediate "thumb pulling activation," students were reminded to use the whole hand as a unit without independent digital effort. They were given a technique reminder to perform a "roll-check" to make sure the toe third was locked onto the tooth just prior to initiating the working stroke. Roll-check means that, after the exploratory stroke and placement of the instrument blade under the deposit, roll the instrument handle/toe toward the tooth to make sure the toe third is on the tooth before you activate the working stroke.26
Many experienced clinicians who attended other instrumentation Boot Camps for Dental Hygiene Clinicians (noneducators) were not completely on the toe third of the blade during their working strokes. They too, overworked their hands by compensating with additional lateral pressure. So many clinician attendees were looking for sophisticated techniques to overcome their struggles. The answer was something as simple as not really using the toe third of the blade during the working stroke!25,26
Protect your wrist
The old expression "wrist rock" is one that has left our current teaching vocabulary. Bending and flexing the wrist for each and every stroke often causes injury. The wrist must remain in a neutral position as the hand and arm move as a continuum during instrumentation.1,26,28,29,30 During instrumentation, the whole hand and arm move just as they do when one is turning a door knob.1
While extraoral fulcrums are most effective for access to maxillary third molars, they are least effective for leverage and reduced workload on the hand everywhere else in the mouth. This has been clearly demonstrated in a study conducted at the School of Dentistry, University of California at San Francisco by Dr. Hui Dong et al. In the study, muscle activity and thumb pinch force were measured by electromyography and pressure sensor to compare extraoral fulcrums, intraoral single finger rest, and intraoral two-finger rests. Both intraoral fulcrums (finger rests) significantly reduce muscle activity and thumb pinch in comparison to the extraoral fulcrum that had no finger rests.31
To lift deposits from a root surface, the fulcrum (finger rest) placement should be in a more apical position to help with the leverage of lifting the deposit off the tooth. A more coronal fulcrum (finger rest) placement tends to make clinicians pull to remove deposits, while a more apical fulcrum placement facilitates leverage for lifting deposits off the teeth as opposed to trying to pull deposits off the teeth.
Whenever possible, assist with the index finger or thumb of the nondominant hand by pressing against the shank of the instrument to control the instrument tip. A lifting working stroke will place the least effort and workload on the hands.25,26,32 Whenever the index finger or thumb of the nondominant hand can be used to stabilize the shank of the instrument, there is increased leverage and additional precision for control of the toe third on the tooth (see Figure 2).
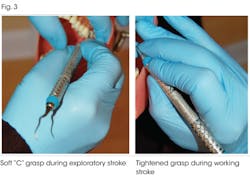
Having the most deft hand skills in periodontal instrumentation cannot spare the overworked dental hygienist. Too many patients per day and per week with not enough rest periods between patients will overwork the hands. Even the rest periods between working strokes are important. At the end of the working stroke, the hand should be relaxed, evidenced by a grasp with soft "C" of the thumb and index finger. The soft "C" grasp remains during the exploratory stroke and only changes in shape for the working stroke (after the "roll check" at the "lock on toe third" step)1,26 (see Figure 3).
When you are working on patients it is difficult to be modifying your instrumentation technique. Work on only one change per week. Otherwise you will slow yourself down so much you will get behind schedule and become overly stressed.
Have someone videotape you often to evaluate your progress in reducing your workload to your hands during instrumentation. You can be your own best teacher. Team up with other hygienists for peer reviews. Be open to feedback so that you can work smarter and be free of hand pain and fatigue.
There is no doubt you are a dedicated hygienist, or you would not be reading this article and open to new ideas that could help you last in our profession. Your patients must be pleased with your dedication and excellent care.
The techniques described in this article are to help you prevent injury to yourself while being just as effective as you always have been at giving quality care to your patients.
Self-assessment of hand pain
To determine what is causing your hand pain, start by assessing your hands and joints for arthritis and/or joint mobility. See your physician if you suspect you have physical hand problems.
Also, have someone videotape you (even using a cell phone will do) while you are performing instrumentation. Look at the video and run through the following checklist as you assess your performance:
- Proper patient-operator positioning.
- "Pen grasp" with all fingers together so hand can function as a unit.
- Watch to see if you have a soft "C" grasp during the exploratory stroke and working "C" grasp only during the working stroke.
- Whole hand and arm as a unit during activation of working stroke. No thumb or index finger pulling.
- Fulcrum (finger rests) in more apical placement whenever possible to get the most leverage to lift rather than pull off subgingival deposits.
- Relaxed hand during exploratory stroke evidenced by soft "C" thumb and index finger.
Cynthia Biron Leiseca, RDH, EMT, MA, is president of DH Methods of Education, Inc. She is the leader of Boot Camps for Dental Hygiene Educators (www.DHmethEd.com)
References
1. Nield-Gehrig JS. Periodontal instrumentation and advanced periodontal instrumentation. 7th ed. Lippincott, Williams & Wilkins, Baltimore 2013.
2.Hayes MJ, Smith DR, Cockrell D. An international review of musculoskeletal disorders in the dental hygiene profession. Int Dent J. 2010 Oct; 60(5):343-52.
3. Morse T, Bruneau H, Michalak-Turcotte C, Sanders M, Warren N, Dussetschleger J, Diva U, Croteau M, Cherniack M. Musculoskeletal disorders of the neck and shoulder in dental hygienists and dental hygiene students. J Dent Hyg. 2007 Winter; 81(1):10. Epub 2007 Jan 1.
4. Hayes MJ, Taylor JA, Smith DR. Predictors of work-related musculoskeletal disorders among dental hygienists. Int J Dent Hyg. 2012 Nov;10(4):265-9. doi: 10.1111/j.1601-5037.2011.00536.x. Epub 2011 Nov 14.
5. Hayes M, Osmotherly P, Taylor J, Smith D, Ho A. The effect of wearing loupes on upper extremity musculoskeletal disorders among dental hygienists. Int J Dent Hyg. 2013 Jul 26. doi: 10.1111/idh.12048.
6. Jennifer R, Thomas FD. Dental hygienists' opinions about loupes in education. J Dent Hyg. 2007 Fall; 81(4):82. Epub 2007 Oct 1.
7. Wilson JD, Darby ML, Tolle SL, Sever JC Jr. Effects of occupational ultrasonic noise exposure on hearing of dental hygienists: a pilot study. J Dent Hyg. 2002 Fall; 76(4):262-9.
8. Cherniack M, Brammer AJ, Nilsson T, Lundstrom R, Meyer JD, Morse T, Neely G, Peterson D, Toppila E, Warren N, Atwood-Sanders M, Michalak-Turcotte C, Abbas U, Bruneau H, Croteau M, Fu RW. Nerve conduction and sensorineural function in dental hygienists using high frequency ultrasound handpieces. Am J Ind Med. 2006 May; 49(5):313-26.
9. Trenter SC, Walmsley AD. Ultrasonic dental scaler: associated hazards. J Clin Periodontol. 2003 Feb;30(2):95-101.
10. Necking LE, Fridén J, Lundborg G. Reduced muscle strength in abduction of the index finger: an important clinical sign in hand-arm vibration syndrome. Scand J Plast Reconstr Surg Hand Surg. 2003; 37(6):365-70.
11. Khosravi M, Bahrami ZS, Atabaki MS, Shokrgozar MA, Shokri F. Comparative effectiveness of hand and ultrasonic instrumentations in root surface planing in vitro. J Clin Periodontol. 2004 Mar; 31(3):160-5.
12. Ioannou I, Dimitriadis N, Papadimitriou K, Sakellari D, Vouros I, Konstantinidis A. Hand instrumentation versus ultrasonic debridement in the treatment of chronic periodontitis: a randomized clinical and microbiological trial. J Clin Periodontol. 2009 Feb; 36(2):132-41. doi: 10.1111/j.1600-051X.2008.01347.x.
13. Simmer-Beck M, Branson BG. An evidence-based review of ergonomic features of dental hygiene instruments. Work. 2010; 35(4):477-85. doi: 10.3233/WOR-2010-0984.
14. Juul-Kristensen B1, Røgind H, Jensen DV, Remvig L. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology (Oxford). 2007 Dec; 46(12):1835-41. Epub 2007 Nov 15.
15. Aktas I, Ofluoglu D, Albay T. The relationship between benign joint hypermobility syndrome and carpal tunnel syndrome. Clin Rheumatol. 2008 Oct;27(10):1283-7. doi: 10.1007/s10067-008-0909-x. Epub 2008 Jun 5.
16. Smith TO, Bacon H, Jerman E, Easton V, Armon K, Poland F, Macgregor AJ. Physiotherapy and occupational therapy interventions for people with benign joint hypermobility syndrome: a systematic review of clinical trials. Disabil Rehabil. 2013 Jul 26.
17. Bagis S, Sahin G, Yapici Y, Cimen OB, Erdogan C. The effect of hand osteoarthritis on grip and pinch strength and hand function in postmenopausal women. Clin Rheumatol. 2003 Dec; 22(6):420-4. Epub 2003 Nov 5.
18. Brorsson S, Hilliges M, Sollerman C, Nilsdotter A. A six-week hand exercise programme improves strength and hand function in patients with rheumatoid arthritis. J Rehabil Med. 2009 Apr; 41(5):338-42. doi: 10.2340/16501977-0334.
19. Haugen IK, Ostergaard M, Eshed I, McQueen FM, Bird P, Gandjbakhch F, Foltz V, Genant H, Peterfy C, Lillegraven S, Haavardsholm EA, Bøyesen P, Conaghan PG. J Rheumatol. Iterative development and reliability of the OMERACT hand osteoarthritis MRI scoring system. 2014 Feb; 41(2):386-91. doi: 10.3899/jrheum.131086. Epub 2013 Dec 1.
20. Stark T, Walker B, Phillips JK, Fejer R, Beck R Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. . PM R. 2011 May; 3(5):472-9. doi: 10.1016/j.pmrj.2010.10.025.
21. Ruiz-Ruiz J, Mesa JL, Gutierrez A, Catillo MJ. Hand size influences optimal grip span in women but not in men. J Hand Surg Am. 2002 Sep; 27(5):897-901.
22. Ranganathan VK, Siemionow V, Sahgal V, Liu JZ, Yue GH. Skilled finger movement exercise improves hand function. J Gerontol A Biol Sci Med Sci. 2001 Aug; 56(8):M518-22.
23. Shim JK, Hsu J, Karol S, Hurley BF. Strength training increases training-specific multifinger coordination in humans. Motor Control. 2008 Oct; 12(4):311-29.
24. Jansen CW, Patterson R, Viegas SF. Effects of fingernail length on finger and hand performance. J Hand Ther. 2000 Jul-Sep;13(3):211-7.
25. Leiseca CB. Precision in periodontal instrumentation. 2nd Ed. 2010: Chapters 1-3 http://www.dhmethed.com/category/BAV2.html.
26. Leiseca CB et al. Boot Camp for Dental Hygiene Educators Boston 2010, Jacksonville 2011-2012, Amelia Island 2013-2014 http://www.dhmethed.com/category/EC5.html.
27. Johanson ME, Valero-Cuevas FJ, Hentz VR. Activation patterns of the thumb muscles during stable and unstable pinch tasks. J Hand Surg Am. 2001 Jul; 26(4):698-705.
28. Gehrmann S, Tang J, Kaufmann RA, Goitz RJ, Windolf J, Li ZM. Variability of precision pinch movements caused by carpal tunnel syndrome. J Hand Surg Am. 2008 Sep; 33(7):1069-75. doi: 10.1016/j.jhsa.2008.02.030.
29. Visser B, de Looze MP, Veeger DH, Douwes M, Groenesteijn L, de Korte E, van Dieën JH. The effects of precision demands during a low intensity pinching task on muscle activation and load sharing of the fingers. J Electromyogr Kinesiol. 2003 Apr; 13(2):149-57.
30. Dumont CE, Popovic MR, Keller T, Sheikh R. Dynamic force-sharing in multi-digit task. Clin Biomech (Bristol, Avon). 2006 Feb; 21(2):138-46. Epub 2005 Oct 12.
31. Dong H, Barr A, Loomer P, Rempel D. The effects of finger rest positions on hand muscle load and pinch force in simulated dental hygiene work. J Dent Educ. 2005 Apr; 69(4):453-60. School of Dentistry, University of California-San Francisco, CA, USA.
32. Leiseca CB. A focus on fulcrums 2008 Chapter 3-5 http://www.dhmethed.com/category/BAV2.html.
Past RDH Issues