Instrumentation techniques and exercise such as yoga can minimize occupational injuries
By Aubreé M. Chismark, RDH, MS, and Diane Millar, RDH, MA
Imagine working as a dental hygienist and never being concerned about work-related hand or arm pain. Certainly with all the available literature on neutral ergonomic hand, wrist, and arm positions, preventive scaling techniques, and healthy stretching exercises, practicing pain free should be simple, right? This is wishful thinking. Having available literature and knowledge is only beneficial if it's implemented routinely. How can a different result be expected if knowledge isn't translated into action?
Unfortunately, evidence shows that work-related musculoskeletal disorders (MSD) are recognized as a considerable problem for the dental hygiene profession, with a majority of the professionals reporting musculoskeletal pain.1 While practicing, a dental hygienist must have a conscious awareness of instrument grasp, pinch force, finger rest positions, fulcrum pivoting, intraoral and extraoral fulcrum rest positions, and neutral hand, wrist, and arm positions in order to employ productive and preventive techniques while scaling.
---------------------------------------------------------------
See related articles
---------------------------------------------------------------
The dominant hand must work as a unit with the instrument in order to enhance precision and stability. Orchestrating these skills can be a challenge depending on learned techniques in dental hygiene school. The risk factors associated with carpal tunnel syndrome and other hand disorders include repetitive hand motions, forceful pinching or gripping, sustained awkward wrist postures, and vibration.2 Attention must be given to these fundamentals since dental hygienists are predisposed to hand, wrist, and arm injuries.
Musculoskeletal disorders (MSD) have been reported among registered dental hygienists and dental hygiene students (DHS), adversely impacting their daily performance and career longevity. RDHs and DHS have reported pain in the following areas -- neck,1,3-5 shoulder,1,3-5 lower back,1,3,4 forearm,1 wrist/hand,3 and upper back.3 RDHs working in a general dental office reported pain more frequently in the shoulder region, and those working in a periodontal office reported forearm pain. Hand scaling caused neck pain among RDHs, and the use of ultrasonic scalers caused shoulder, upper back, or lower back pain for longer than two days.1 RDHs who reported wearing loupes were less likely to report shoulder and wrist/hand pain, and less likely to have neck or upper back pain for more than two days.1
Dental hygiene students who do not exercise regularly have reported a higher incidence of low back pain, and working on a computer increases shoulder and upper back pain.4 Consequently, the daily lives of DHS have been affected by musculoskeletal pain, causing them to seek medical treatment.4 RDHs with pain were less likely to seek treatment if ergonomics were reinforced in the clinic during their dental hygiene education.3 In view of that, reinforcing ergonomics and incorporating the use of loupes and reinforced instrumentation into the dental hygiene curriculum may benefit the career longevity of RDHs.
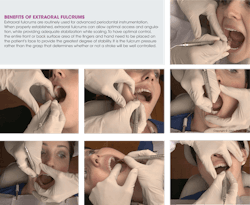
Reinforced fulcrums for optimum scaling efficacy and injury prevention -- Dental hygiene instrumentation techniques have dramatically improved throughout the years to prevent MSD. New and innovative techniques using protective reinforced instrumentation techniques require scaling teeth with two hands instead of one to ensure optimum performance and to promote occupational health and career longevity. These techniques allow the nondominant hand to assist the dominant hand and instrument for more stability, lateral pressure, and precision.6
Using the index finger to press on the long terminal shank with the nondominant hand while using extraoral fulcrums helps the operator to adapt the instruments and attain more lateral pressure. As the dominant hand adapts and angulates the blade of an instrument to tooth surfaces, the nondominant hand provides additional pressure in the same direction to which the dominant hand's fingers are directing pressure. This helps operator protection during strenuous and extensive instrumentation processes by engaging the large muscle groups over the small muscle groups in the hand and wrist.
If a clinician experiences pain, the utilization of reinforced instrumentation techniques helps to decrease hand, wrist, and arm pain. The definition of "reinforce" is to strengthen with some added piece of support.7 The increase in strength while using reinforced fulcrums and rests occurs from the use of both hands. The thumbs are also beneficial to incorporate while using reinforced instrumentation. When the nondominant thumb bridges over to the dominant thumb of the working hand, both hands have the opportunity to work together as a unit. When both hands work in unison, the larger muscle groups of both arms can also work in unison.8
Intraoral and extraoral fulcrum techniques combined for stability and precision -- Intraoral fulcrum techniques are established by placing the pad of the fulcrum finger on a tooth surface adjacent or close to the tooth being instrumented. This technique has been the standard school of thought in the dental hygiene profession for many years. All dental hygiene schools introduce intraoral fulcrums before teaching extraoral fulcrums, which requires stabilization of the clinician's dominant hand against the patient's cheeks, jaws, and chin. Extraoral fulcrums require the front or back of the fingers to be used as hand rests to provide support, rather than the tips or pads of the fingers as with intraoral fulcrums. Using both intraoral and extraoral fulcrum hand rests simultaneously will increase stabilization of the hand and arm, as well as precision while scaling, versus using just one or the other.
Strategies for injury prevention to the hands and arms while scaling -- The following recommendations are worth considering to help prevent pain and injury to a clinician's hands and arms, and to enhance scaling efficacy with biomechanical and ergonomic principles:
- Establish a modified pen grasp where the thumb and finger oppose one another and the instrument handle is visible between the fingers.
- All fingers should work together as a unit while scaling.
- Use large diameter handles and light instruments to reduce excessive pinch force.
- Consider using 11.5 mm diameter silicone (LM-Dental) or resin handles in conjunction with power scaling for every patient appointment to prevent injury.
- Always establish a neutral hand, wrist, and arm position while scaling.
- Orient the instrument with the tooth surface to be instrumented, taking into consideration the angulation of all teeth.
- Keep the instrument parallel to the long axis of the surface of the tooth. This will encourage a neutral hand, wrist, and arm posture.
- Use intraoral and extraoral fulcrums to enhance a neutral position of the hand, wrist, and arm.
- Avoid flexion and extension of the hand as much as possible while scaling.
- Avoid sustained awkward wrist postures to prevent carpal tunnel syndrome.
- Practice palm up fulcrums as often as possible, and avoid palm down fulcrums that increase strain on the hand and wrist.
- Establish a "built-up" fulcrum, keeping fingers together as a unit while scaling.
- Keep the ring finger straight, with the tip of the finger supporting the weight of the hand when using intraoral fulcrums.
- Pivot on the fulcrum finger to support the hand as it turns to allow for hand repositioning.
- Use advanced reinforced fulcrums using intraoral and extraoral rests to gain access to root surfaces and to prevent hand stress and strain.
- Incorporate the nondominant hand by pressing on the instrument for more lateral pressure, power, and precision.
- Implement thumb-to-thumb reinforcement for more stability and precision, and to engage the use of the larger muscle groups in both arms while scaling.
- Consider bringing the elbow out and over the patient at times to keep wrist in alignment with the long axis of the forearm.
- Keep the dominant hand neutral to prevent radial and ulnar deviation while scaling.
- Use fulcrum pressure equal to the pressure of the instrument blade against the root surface being scaled.
- Increase fulcrum pressure if slipping or lack of lateral pressure occurs.
- Implement pull strokes instead of side-to-side rocking strokes in order to enhance instrument placement to the epithelial attachment and reduce repetitive motions.
- Use sharp instruments to minimize lateral pressure and number of strokes.
- Consider using XP sharpen-free technology instruments (American Eagle Instruments) to reduce lateral pressure while scaling.
- Make every stroke count to reduce repetitive motion injuries.
- Implement intermittent rests between strokes to prevent pain and injury.
- Listen to your body and take mini-breaks to avoid prolonged, static postures.
- Stretch hands, arms, and upper body routinely to prevent pain and injury.
Adverse effects of MSD and the use of complementary and alternative medicine (CAM)
MSD are frequently reported by practicing RDHs due to the physical demands placed on the body caused by poor ergonomics, repetitive motion, pinch force, and grasp.2 RDHs who reported MSD reduced the number of hours they worked,3 took time off from work, called in sick,1,3 considered changing careers,1,3 and even left clinical practice.1 CAM therapies including massage, herbal supplements, chiropractic care, yoga, and acupuncture are being used by RDHs to reduce musculoskeletal pain.3 RDHs are more likely to use a combination of CAM and conventional therapies to manage their MSD, although RDHs who use CAM therapies alone are less likely to temporarily quit work, experience improvement in musculoskeletal pain, and report higher career satisfaction.3
Using CAM therapies has increased job happiness and security and overall health and well-being, contributed to career longevity, and enabled RDHs to work the number of hours they prefer.3 RDHs with MSD feel that CAM therapies are acceptable methods of pain management that should be covered by medical insurance, and they would use CAM as an alternative method to conventional medicine.3 CAM therapies have a positive effect on RDHs' overall health and career satisfaction,3 and should be considered for use early on.
Yoga and pain reduction
Yoga is a CAM therapy that unites the body, mind, and spirit using breathing methods and a series of standing and seated postures. It is a mindful type of practice where individuals focus their breath and attention on proper alignment in order to gain the full benefits of each pose. There are many types of yoga styles, including but not limited to Hatha, Vinyasa, Kundalini, and Iyengar. Yoga targets a number of muscle groups, leading to improved posture and spinal alignment.9 Yoga has been shown to reduce pain,9,10,11,13 the need for medication,10 and to improve function9-13 among the general population. Pain reduction has been reported when individuals practiced yoga at least once a week for a minimum of 12 consecutive weeks.10-12 Yoga has also been shown to reduce stress and bring a sense of peace and well-being to the mind.9 Since yoga has been shown to reduce pain among the general population, serious consideration should be taken to incorporate yoga into the dental hygiene curriculum to prevent pain while in school and later in the career.
MSD have been reported among RDHs and DHS, causing a negative impact on their daily lives, and eventually leading to reduced work hours, calling in sick, or leaving the profession. Reinforced instrumentation techniques should be introduced during school and used throughout a dental hygiene career in order to reduce hand, wrist, and arm pain. Ultimately, ergonomics should be reinforced in the clinical setting, and CAM education, such as yoga, should be incorporated into the dental hygiene curriculum to prevent MSD from occurring. Incorporating change is not always easy for clinicians to accept or adapt to, although action must be taken in order to get a different result so as to increase career satisfaction and longevity of the dental hygiene profession.
Aubreé M. Chismark, RDH, MS, is an assistant professor in the dental hygiene department at West Coast University in Anaheim, Calif., and is a member of the CDHA Journal Advisory Board. She is registered yoga teacher with the Yoga Alliance (200- hours) and is currently working toward her 500-hour certification. Her research interests include ergonomics and the use of complementary and alternative medicine to reduce chronic musculoskeletal pain. She can be contacted at: [email protected].
Diane Millar, RDH, MA, graduated from the West Los Angeles College dental hygiene program in 1981. Her career in dental hygiene has embraced working in private practice and teaching advanced instrumentation techniques at The University of Southern California, Cerritos College, and currently at West Coast University. She is a national speaker and is also the published author of "Reinforced Periodontal Instrumentation and Ergonomics for the Dental Care Provider." Diane is a CE Provider for the CA Dental Board and conducts seminars and hands-on workshops to help dental professionals learn how to practice more efficiently and ergonomically safe to ensure career longevity. She can be contacted at [email protected].
References
1. Hayes MJ, Taylor JA, Smith DR. Predictors of work-related musculoskeletal disorders among dental hygienists. Int J Dent Hygiene. 2012;10:265-269.
2. Dong H, Barr A, Loomer P, Rempel D. The effects of finger rest positions on hand and muscle load and pinch force in simulated dental hygiene work. J Dent Hyg [Internet]. 2005 [cited 2014 Feb 10]; 69(4): 453-460. Available from http://www.adha.org. Registration required for access.
3. Chismark A, Asher G, Stein M, Tavoc T, Curran A. Use of complementary and alternative medicine for work-related pain correlates with career satisfaction among dental hygienists. J Dent Hyg [Internet]. 2011 [cited 2014 Feb 10]; 85(4):273-284. Available from http://www.adha.org. Registration required for access.
4. Hayes MJ, Smith DR, Cockrell D. Prevalence and correlates of musculoskeletal disorders among Australian dental hygiene students. Int J Dent Hygiene. 2009; 7:176-181.
5. Morse T, Bruneau H, Michalak-Turcotte C, et al. Musculoskeletal disorders of the neck and shoulder in dental hygienists and dental hygiene students. J Dent Hyg [Internet]. 2007 [cited 2014 Feb 10]; 81(1):e16. Available from http://www.adha.org. Registration required for access.
6. Millar D. Reinforced periodontal instrumentation and ergonomics for the dental care provider. 1st ed. Baltimore, MD. Lippincott, Williams, & Wilkins. 2007. pp. 1-38.
7. Reinforce. Dictionary.com, Random House Publishing [Internet]. 2014 Jan [cited 2014 Jan 3]. Available from http://dictionaryreference.com/browse.Reinforce.
8. Millar D. Reinforced periodontal instrumentation and ergonomics: the best practice to ensure optimal performance and career longevity. Journal of the California Dental Hygienists' Association. 2009; 24(3):10-17.
9. Sarosky S, Stilp S, Akuthota V. Yoga and Pilates in the management of low back pain. Curr Rev Musculoskeletal Med [Internet]. 2007 [cited 2014 Feb 10]; 1:39-47. Available from http://link.springer.com/article/10.1007/s12178-007-9004-1/fulltext.html.
10. Saper RB, Boah AR, Keosaian J, et al. Comparing once- versus twice-weekly yoga classes for chronic low back pain in predominantly low income minorities: a randomized dosing trial. Evidence-Based Complementary and Alternative Medicine [Internet]. 2013 [cited 2014 Feb 10]. Available from www.hindawi.com/journals/ecam/2013/658030/.
11. Sherman KJ, Cherkin DC, Wellman RD, et al. A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Archives of Internal Medicine [Internet]. 2011 [cited 2014 Feb 10]. Available from: http://archinte.jamanetwork.com/article.aspx?articleid=1106098.
12. Tilbrook HE, Cox H, Hewitt CE, et al. Yoga for chronic low back pain. Ann Intern Med [Internet]. 2011 [cited 2014 Feb 10];155(9):569-578. Available from http://annals.org/issue.aspx?journalid=90&issueID=20366&direction=P.
13. Williams K, Abildso C, Steinberg L, et al. Evaluation of the effectiveness and efficacy of Iyengar yoga therapy on chronic low back pain. Spine. 2009; 34(19):2066-2076.
14. Payne L, Usatine R. Yoga Rx: a step-by-step program to promote health, wellness, and healings for common ailments. 1st ed. New York, NY. Broadway Books. 2002. pp.146-148.
15. Yoga Poses. Yoga Journal.com [Internet]. 2014 [cited 2014 Feb 19]. Available from http://www.yogajournal.com/poses/finder/browse_index.
Past RDH Issues