By Nancy W. Burkhart, BSDH, EdD
Your patient is William, a 79-year-old male who is the father of an established patient. He is visiting the family in the United States while on a trip from France. The family became concerned when the father called attention to a large, rough enlargement behind his maxillary central teeth.
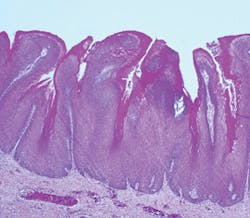
William is a diabetic patient, but his diabetes is controlled through diet. Additionally, he is a former cigarette smoker with a history of smoking for over 30 years. William stopped smoking 10 years ago with no tobacco consumption since quitting. After examining William, you notice that the palatal area of Nos. 8 and 9 exhibits a lighter colored growth of tissue that is exophytic, somewhat papillary, and measures approximately 5 mm by 6 mm in width. Upon questioning the patient, you learn that he noticed the growth about a month ago. He attributed it to a burn from some hot coffee that he had consumed a few days prior (see Figure 1).
----------------------------------------------------------
Other articles by Burkhart:
- Health literacy and the oral cancer exam
- Is it an oral cancer exam or screening?
- Damage caused by lip sucking
----------------------------------------------------------
An appointment was scheduled for William to see an oral surgeon and another digital image was taken two weeks after the first image and just prior to removal of the growth. Figure 2 reveals how the lesion had increased in size.
The diagnosis was verrucous carcinoma.
Epidemiology: Verrucous carcinoma is found more often in individuals with a history of smoking, and this type of cancer appears to affect males more often in the age range of 55 or older who have used spit tobacco, pan, bidis, or smoked cigarettes for many years. Alkan (2010) in a study of 12 cases of verrucous carcinoma reported a ratio of 1.4:1 male to female occurrences. SEER data indicate that the estimated new cases of oral cancer in 2014 to be 42,440, with oral cancer in 2.5% of all new cancer cases.
According to the American Cancer Society, less than 5% of all oral cancers are of the verrucous type. Verrucous carcinoma is associated with spit tobacco, and there are large numbers of tobacco users making the increase of verrucous carcinoma very likely.
Etiology: Tobacco products such as smokeless tobacco and snuff are the most common etiology of verrucous carcinoma because of the carcinogenic properties in these products. N-nitrosamines, volatile aldehydes, and polycyclic aromatic hydrocarbons are considered cancer promoting, and they are in direct contact with the tissues of tobacco users. The products not only cause oral cancer, but other types of cancer such as esophageal and pancreatic cancers.
The term "snuff dippers' cancer" has been attached to this particular type of oral cancer since the lesion is usually found in the area where tobacco is placed. Other tobacco products such as bidis, areca quid, and paan products used mostly in Asia are known to be a contributing factor of leukoplakias in general. Alcohol is also a risk factor for verrucous carcinoma and all oral cancers as well. Human papillomavirus (HPV) of various types is a contributing suspect in some oral cancers, as are other lifestyle factors that add further risk for malignancy.
Verrucous carcinoma is a progressive type of lesion, developing from a smooth appearance to clinically varying appearances of white, cauliflower-like and papillary forms. Verrucous hyperplasia and verrucous keratosis may be clinically indistinguishable from verrucous carcinoma at various stages (Alkan et al., 2010). They may coexist and be both clinically or microscopically undifferentiated in varying stages.
Kallarakkal et al., 2013, make the point that sometimes the pathologist may not covey to the clinician the serious nature of verrucous hyperplasia due to the absence of overt features that would indicate dysplasia. The lesion may progress with time and ultimately be diagnosed as verrucous carcinoma. Murrah and Batsakis (1994) suggested four stages of development in this progression to verrucous carcinoma: 1. Hyperkeratosis without epithelial dysplasia, 2. Verrucous hyperplasia, 3. Verrucous carcinoma, and 4. Conventional squamous cell carcinoma.
Additionally, squamous cell carcinoma may be identified sometimes within the lesions of verrucous carcinoma. The primary areas affected are the buccal mucosa, vestibular mucosa, gingiva, and alveolar mucosa.
Method of transmission: Verrucous carcinoma is thought to be a low grade variant of squamous cell carcinoma. This type of cancer is not thought to be contagious, but a variety of human papillomaviruses (HPV) have been localized within the lesions. Both HPV 16 and 18 are considered high risk. A recent study by Beltiol et al. (2012) found that the prevalence of HPV 18 was found in 100% of a group of patients who had been diagnosed with verrucous leukoplakia. Two groups of patients were studied, one group with verrucous lesions and one group with no lesions.
Reports by Beltiol et al. found HPV 18 in all patients within the verrucous group. Koilocytosis, indicative of HPV and also of dysplasia, depict epithelial cells with a so-called "halo." Koilocytes were found in this group of patients indicating a viral component, (viral proteins E5 and E6) or triggers. The demographics also included that 80% were married men, smokers, alcohol users with an average age of 59.75 years.
More recent studies by Samman, et al. (July 2014) found no conclusive human papillomavirus involvement in a study group of 78 patients with oral verrucous carcinoma. They analyzed oral verucous lesions for HPV subtype genomes.
Clinical characteristics: Early lesions may be more subtle, appearing as flat white-light pink lesions and described as simply "leukoplakia" when viewed clinically. Clinical descriptions may include terms such as sessile, smooth, and spreading over an extended area of tissue. Some fissuring and ulceration may occur at times. As the lesions increase in size, descriptors such as exophytic, verrucous-like with keratosis, or warty may be used to note the lesion. Leukoplakia may be considered a more serious type of lesion when progression is observed and may ultimately be further classified as verrucous carcinoma. A biopsy is always needed for confirmation.
Pathogenesis: Verrucous carcinoma is thought to be a verrucous variant of squamous cell carcinoma. As lesions progress over time, they become verrucous carcinoma. The entity "verrucous hyperplasia" was designated as a precursor to verrucous carcinoma, squamous cell carcinoma, and papillary squamous carcinoma. Van der Waal (2008) suggests that verrucous hyperplasia and perhaps verrucous carcinoma are probably underdiagnosed histopathologically, and may be reported as benign verrucous or papillary proliferations without signs of epithelial dysplasia or invasive growth.
Treatment and prognosis: Verrucous carcinoma has a low incidence of bone invasion and low rates of cervical node metastasis, but the recurrence rate is high. The recommended treatment is surgery with a goal of clear margins. Sciubba and Helman (2013) state that, when dealing with verrucous lesions, laser ablation (sometimes used as a treatment) eliminates the possibility of identifying any invasive squamous cell carcinoma when viewed microscopically.
Squamous cell carcinoma may also be found in some combinations with verrucous lesions, and this finding makes the prognosis less favorable. Other treatments may involve photodynamic therapy, cryotherapy, and radiation therapy. Surgery is the preferred treatment in verrucous carcinoma, and combinations of these therapies are sometimes used. Researchers and clinicians caution that thorough follow-up and monitoring of the patient is necessary for optimal treatment.
Additional thoughts: Proliferative verrucous leukoplakia (PVL) tends to be slightly more common in women in the sixth decade with long-term leukoplakia-type lesions. Lesions progress from a smooth leukoplakia-type appearance to a more classic verrucous appearance. Van der Waal, 2008, states that the diagnosis of proliferative verrucous leukoplakia lies in the awareness of the clinician and the pathologist, stating that innocent-looking oral verrucous leukoplakia may, even in the absence of dysplasia, progress to verrucous carcinoma or squamous cell carcinoma in time. As mentioned previously, Beltiol and colleagues identified HPV in 100% of patients with proliferative verrucous leukoplakia that is an unusual form of oral leukoplakia. The early clinical manifestation of proliferative verrucous leukoplakia is not warty or verrucous; the clinical appearance is described more as a typical leukoplakia.
For more information on PVL, see: Burkhart NW. Proliferative verrucous leukoplakia. RDH. 2010; 30(4): 66-69.
As always, keep asking good questions. and always listen to your patients!
NANCY W. BURKHART, BSDH, EdD, is an adjunct associate professor in the department of periodontics, Baylor College of Dentistry and the Texas A & M Health Science Center, Dallas. Dr. Burkhart is founder and cohost of the International Oral Lichen Planus Support Group (http://bcdwp.web.tamhsc.edu/iolpdallas/) and coauthor of General and Oral Pathology for the Dental Hygienist. She was a 2006 Crest/ADHA award winner. She is a 2012 Mentor of Distinction through Philips Oral Healthcare and PennWell Corp. Her website for seminars on mucosal diseases, oral cancer, and oral pathology topics is www.nancywburkhart.com.
References:
Alkan A, Bulut E, Gunhan O, Ozden B. Oral verrucous carcinoma: A study of 12 cases. Eur J Dent. 2010; 4: 202-207.
Beltiol JC, Kignel S, Tristao W, et al. HPV 18 prevalence in oral mucosa diagnosed with verrucous leukoplakia: cytological and molecular analysis. J Clin Pathol 2012; 65(8):769–70.
Chung CH, Yang YH, Wang TY, Shieh TY, Warnakulasuriya S. Oral precancerous disorders associated with areca quid chewing, smoking and alcohol drinking in southern Taiwan. J Oral Pathol Med 0205;34:460-466.
Delong L & Burkhart NW. General and Oral Pathology for the Dental Hygienist. 2nd Ed. Lippincott Williams & Wilkins. Baltimore, 2013.
Hansen LS. Olson JA, Silverman S. Proliferative verrucous leukoplakia: a long-term study of thirty patients. Oral Surg Oral Med Oral Path 1985:60:285-298.
Kallarakkal TG, Ramanathan A, Zain RB. Verrucous papillary lesions: Dilemmas in diagnosis and terminology. Int J Dent. 2013:298249.
Murrah VA, Batsakis JG. Proliferative verrucous hyperplasia. Ann Otol Rhinol Laryngol. 1994; 103;660-663.
Samman M, Wood H, Conway C, et al. Next-generation sequencing analysis for detecting human papillomavirus in oral verrucous carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:1;117-125.
Sciubba JJ, Helman JI. Current management strategies for verrucous hyperkeratosis and verrucous carcinoma. 2013. Oral Maxillofacial Surg N Am 25:77-82.
The National Cancer Institute.
http://seer.cancer.gov/statfacts/html/oralcav.html
van der Waal I. Oral proliferative verrucous leukoplakia revisited. Oral Oncology 2008:44:719-721.
Past RDH Issues