Do you remember the lyrics from Howard Jones's hit song: "Bend your brain ... throw off your mental chains"? These lyrics have become a sort of mantra with me. I have been a hygienist since 1979. Through my many years of practice, one of the most difficult things I have had to face is the re-examination of many of the "truths" ingrained in me from my education and early years in dentistry.
As I speak with other hygienists, as well as dentists, it becomes clear to me that the strict and rigorous education we experienced often discouraged us from questioning things and exploring alternative avenues of patient care. As technology evolves, research in the areas of the periodontal disease process and the impact this chronic disease has on overall health should encourage us to examine what we are doing, why we are doing it, and whether we could be more effective.
During my years in hygiene school, I was not taught about different treatment options to offer my patients. The emphasis of my training was the removal of calculus and patient education.
My worth as a clinician was measured by how successful I was at scaling off calcified deposits. This is, of course, a key skill that must be mastered. It was considered to be such a critical skill that it allowed me little time to concentrate on anything else. My primary function was to robotically debride teeth and give the standard floss lecture. I remembered wishing that my patients were happier to see me. Let's face it, getting subgingival scaling and a lecture is not a pleasant experience. In fact, it is physically and emotionally painful. I believed what I was doing was in the best interest of my patients, just as I had been taught in school.
After 10 years as a clinician, I seriously wondered if I was really making a difference in my patients' lives. Was I helping them get healthier? Did their behavior change? Sadly, in many cases, my efforts were not having a lasting impact. I felt frustrated, but I did not see what I could do differently.
It was around this time that I was introduced to a new way of treating my patients. I started working for a doctor who told me he was going to bring in a trainer to teach me the hygiene protocol that he had in his practice. I soon met Peggy Sprague, one of the co-founders of the JP Institute. She taught me how to effectively communicate with my patients. She also showed me a revolutionary clinical protocol that allowed me to get the best clinical results I had ever achieved.
What Peggy and her partner, Jan Lazarus, had developed was a restructuring of the hygiene appointment to allow time for patient education. The information was presented in a very compassionate, nonthreatening way. The guilt that so often is a part of the standard flossing lecture was gone, because that speech was gone.
What Is Health?
At our office, we stopped blaming people for their periodontal condition and instead focused on the treatment they needed to allow their periodontium to heal. We offered them a treatment plan that was customized according to their level of bleeding and other health issues. In addition to bleeding levels, systemic conditions, medications, recession, attachment loss, restorative and occlusal factors, behavior modification needs, and family health history are also considered. These are the criteria we primarily use, rather than simply pocket depths and calculus levels. Of course, we look at pocket depths and calculus as well, but those are not the key determinants of how much treatment a patient would need.
Needless to say, this was quite contrary to what I had been taught in school and quite ahead of its time in 1988. In school, I was taught that if our patients would only floss, they would become healthy. How many patients have you seen who floss daily and still have bleeding gingival tissues?
The question we must ask ourselves is: What is health? Is a 3mm pocket that has bleeding acceptable? Now that we know much more about the systemic link and the fact that pathogenic bacteria is entering the blood stream through the open wound at the base of a bleeding pocket, can we really dismiss even a little bleeding and not be concerned? Should we not offer more to our patients to give them the opportunity to have perfect tissue without bleeding?
Open-ended therapy is provided until a patient achieves whatever healing their bodies are capable of achieving. We must consider not only the etiology present in the patients' mouths (i.e., bleeding, pockets, calculus), but also look at the other factors as mentioned above to determine approximately how many therapeutic appointments are indicated. Would the patient benefit from the use of locally applied antibiotics such as Arestin? The treatment plan is based on patient need, not insurance allowances. Not everyone fits into the "four quads of root planing" category. Some patients need less, some need more. The American Academy of Periodontology states: "A one-size-fits-all treatment plan for periodontal diseases does not exist."1 Why not give patients what they need?
Stubborn Attachment to Floss
Now, for more "brain bending," we should let go of our stubborn attachment to floss. Don't get me wrong. I wish everyone would floss daily. I do! Why can't they? Well, after all these years, I have come to the conclusion that not everyone is going to floss. Big surprise, huh! Even when patients floss daily, how far subgingivally can they get? Two millimeters, three? How deep are their pockets? Four, five, six millimeters or more?
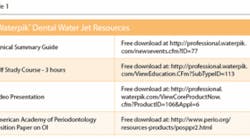
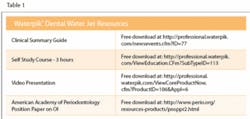
We need to give our patients other alternatives. The most effective and user-friendly alternative I have personally seen is the Waterpik® dental water jet. I never used to recommend them because my instructors in school told me that they were ineffective at plaque removal. To the contrary, as a working clinical hygienist, I have never seen tissue as healthy as when a patient uses a Waterpik dental water jet.
Let's put aside the evidence we see before our own eyes and look at the research:
• Reduction of bleeding and gingivitis: Newman et al. found that people in periodontal maintenance who added a dental water jet to routine oral hygiene were able to reduce gingivitis and bleeding better than subjects who only brushed and flossed.2
• Reduction of periodontal pathogens: Cobb et al., and Drisko et al. demonstrated the reduction of periodontal pathogens up to six millimeters.3,4
• Noncompliance with dental floss: Barnes et al. found that once-daily irrigation with water added to either a manual or power toothbrush was an effective alternative to dental floss for the reduction of bleeding, gingivitis, and plaque, and in some cases provided superior results for reducing bleeding and gingivitis.5
Additional studies also affirm the effectiveness of dental water jets, as well as studies suggesting benefits for people with diabetes, implants, and crown and bridge.6,7,8 All the research demonstrates that they are effective and safe.
Change is hard, but change is good. If we are still practicing the way we were 20, 10 or even five years ago, we have not been keeping up with the research and technology. If what we are doing is not working for our patients, we really should try something new.
Sometimes it may feel like we are experimenting, and we should be. If what we read and learn in classes makes scientific sense, and is safe, we should offer it to our patients and see what good results we can obtain. We need to make up our minds about the effectiveness of any treatment or adjunct based on our own experience rather than forming our opinions based on dogma only.
So, let's "bend our brains" and try something new. Not only is it good for our patients, it is good for us. Clinician who are stuck in a rut will lose their passion for what they do and will become less effective as health-care professionals.
About the Author
Liz Lundry, RDH, has been a practicing hygienist since 1979 when she graduated from Foothill College. She has worked in many general practices throughout California and currently works as a clinical hygienist in a boutique practice that offers state of the art cosmetic and laser dentistry. Liz has been laser certified since 2000. She is a senior consultant and laser trainer for The JP Institute. Liz began her association with The JP Institute in 1988. For more information about the Mastership courses provided by JP Institute, call (800) 946-4944, or visit www.jpconsultants.com. For more information about the Waterpik® dental water jet, visit www.waterpik.com.
References:
1. Guidelines for the Management of Patients with Periodontal Disease. J Periodontol 2006; 77:1-5. Free download at http://www.perio.org/resources-products/posppr2.html.
2. Newman MG et al. Effectiveness of adjunctive irrigation in early periodontitis: Multi-center evaluation. J Periodontol 1994; 65:224-229.
3. Cobb CM et al. Ultrastructural examination of human periodontal pockets following the use of an oral irrigation device in vivo. J Periodontol 1988; 59:155-163.
4. Drisko C et al. Comparison of dark-field microscopy and a flagella stain for monitoring the effect of a Water Pik on bacterial motility. J Periodontol 1987; 58:381-386.
5. Drisko C et al. Comparison of dark-field microscopy and a flagella stain for monitoring the effect of a Water Pik on bacterial motility. J Periodontol 1987; 58:381-386.
6. Al-Mubarak S et al. Comparative evaluation of adjunctive oral irrigation in diabetes. J Clin Periodontol 2002; 29:295-300.
7. Felo A et al. Effects of subgingival chlorhexidine irrigation on peri-implant maintenance. Am J Dent 1997; 10:107-110.
8. Krajewski J et al. Evaluation of a water pressure cleaning device as an adjunct to periodontal treatment. J Amer Soc Periodont 1964; 2:76-78.