Have you ever wished you could wave a magic wand to get patients to follow your recommendations? You’re banging your head, knowing deep down their oral and overall health would improve if they would just comply. And when it comes to recommendations on nutrition, compliance can be even more challenging. There is no question that nutrition is important to oral health as there is strong evidence regarding their bidirectional relationship.1
The real question is in the “how.” How do we help patients with their nutritional choices? How do we get them to want to change? And how do we get lasting results? Let’s explore the latest in behavioral change psychology and some practical applications to increase compliance while giving nutritional advice.
Barriers for the dental hygienist
It’s a fact that hygienists face difficulties when trying to improve patients’ dietary choices. In a recent survey, Hayes et al. identified time, patient compliance, patient knowledge, and personal counseling skills to be among the top perceived barriers for hygienists in providing adequate nutritional advice.2 In addition, there is a lack of standardization in US dental hygiene programs when it comes to nutritional education.3 As hygienists, we are expected to give dietary recommendations for oral health, yet there is limited guidance on how to accomplish it.
More about nutrition ... Oral health and nutrition: Do your patients understand the connection?
Within the dental industry, there is a push to move into a biopsychosocial model of care that looks at a patient from all aspects of their life. Adopting some principles from psychology into dental practice may help us look at patients from a comprehensive point of view, increasing hygienists’ confidence in delivering nutritional advice as well as improving patient compliance.
Behavioral science and the COM-B model
In 2022, a consensus statement was released by the International Association for Dental Research highlighting the importance of research and applications of behavioral science in oral health.4 Behavioral science is the study of people’s actions and habits. It draws from several disciplines while using a scientific method for evidence-based information and recommendations. Behavioral science research is used to develop and test theories, frameworks, and behavioral change techniques to disseminate information for use in a variety of settings, from public health policies to health-care settings.
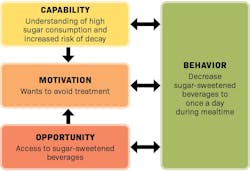
Research suggests that interventions based on theory are more effective.5 For dental hygienists, this means our oral hygiene instructions and recommendations should be based on behavioral change principles. One of the most recent behavioral change models is starting to gain traction within the dental community: COM-B.6-8 This model describes how three interrelated factors—capability (C), opportunity (O), and motivation (M)—are needed for a behavior (B) to happen.
There is emerging evidence and a push among researchers to use the COM-B model for improving dietary choices, tobacco cessation, periodontal health, and caries management.9-12 The COM-B model is a comprehensive and systematic approach to behavioral change. All three components work synergistically with one another. Applying this to an intervention requires identifying the target behavior as well as the components of the behavioral system that need to change for the desired outcome.
Yoy may also be interested in ... Are we sweet enough? Understanding the health effects of sugar
Capability encompasses both the person's physical and psychological capacity. Questions to think about when considering a patient’s capability would include: Are they physically able to perform a desired behavior (skills, dexterity, strength)? Do they have the knowledge required?
Opportunity focuses on the person’s environment both physically and socially. This would include thinking about the patient’s family and surrounding community as well as their physical access to resources needed for the behavioral change.
Motivation describes the person’s desire to have a particular behavior. Do they want to change? What’s their reason for change? What is their self-efficacy—i.e., the confidence they have in achieving the desired outcome?
Nutritional applications
While the COM-B model can be applied to any aspect of dental hygiene recommendations, we’ll focus on its nutritional relevance. Adapted from Atkins and Michie’s “Designing interventions to change eating behaviours,”13 this is the process we’d use to choose a target behavior for a hypothetical patient and find impactful, personalized solutions:
Case study: A 28-year-old male patient presents with two active carious lesions. The patient had treatment for decay within the last year. An initial nutritional assessment revealed that he drinks a sugar-sweetened beverage (SSB) on average four times a day.
Define the problem: The patient has high caries risk.
Select the target behavior: It is recommended that target behaviors be as specific as possible.13,14 As clinicians, think about the who, what, when, and where, working with the patient to identify a target behavior that is realistic and detailed. Small, realistic goals will have a higher likelihood of success and sustainability.13 For our scenario, we’ll select a target behavior of decreasing SSBs to one time a day with a meal.
Identify what needs to change: Having COM-B top of mind, the hygienist can tailor open-ended questions to reveal further details regarding the patient’s factors and categorize them based on their corresponding component (capability, opportunity, and motivation). Figure 1 shows examples of possible components related to this scenario.
Prioritize the intervention: Hygienists can then critically think about which components to focus on first, prioritizing the components with the most likelihood of effecting the target behavior. From there, behavioral change techniques (e.g., goal-setting, planning, self-monitoring) can aid in accomplishing the behavior change.14
In this example, let’s say the patient agrees to drinking his favorite soda at lunch instead of three to four sodas throughout the day. Instead of buying in bulk, he set a goal to purchase a limited amount of soda during his grocery visit—just enough for one soda a day. This would affect the opportunity component by changing his environment to better support his target behavior.
Applying the COM-B model is an effective, systematic way to gain a baseline understanding of how to accomplish successful interventions within our scope of practice. It can also assist the hygienist in recognizing the potential need for referral to an appropriate professional, such as a registered dietician nutritionist, when more in-depth evaluation/counseling is warranted.
Staying evidence-based
The key to compliance is not as simple as a swish and flick of a wand. But now we have more guidance to help us improve our patients’ nutritional choices. By understanding the foundations of COM-B, clinicians can use this knowledge as a starting point for recommendations. As an evidence-based profession, dental hygiene can use such research as a guide to start implementing behavioral science into dental practice. Now is the time for hygienists to start incorporating this paradigm shift into patient care, and in doing so, make a lasting impact on oral and overall health.
Author’s note: Want to delve further into this subject? COM-B is at the hub of an expanded system called the Behavior Change Wheel. For an in-depth guide to behavioral change interventions, see the book, The Behaviour Change Wheel, by Mitchie et al.15
Editor's note: This article appeared in the January/February 2024 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Oral health in America: a report of the surgeon general. U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health. 2000. https://www.nidcr.nih.gov/sites/default/files/2017-10/hck1ocv.%40www.surgeon.fullrpt.pdf
- Hayes MJ, Wallace JP, Coxon A. Attitudes and barriers to providing dietary advice: perceptions of dental hygienists and oral health therapists. Int J Dent Hyg. 2016;14(4):255-260. doi:10.1111/idh.12239
- Onofrietti SL, Gurenlian J. Didactic and clinical nutrition content in dental hygiene programs: directors’ perspective. J Dent Educ. 2023;87(4):497-504. doi:10.1002/jdd.13145
- McNeil DW, Randall CL, Baker S, et al. Consensus statement on future directions for the behavioral and social sciences in oral health. J Dent Res. 2022;101(6):619-622. doi:10.1177/00220345211068033
- Davis R, Campbell R, Hildon Z, Hobbs L, Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev. 2015;9(3):323-344. doi:10.1080/17437199.2014.941722
- Buchanan H, Newton JT, Baker SR, Asimakopoulou K. Adopting the COM-B model and TDF framework in oral and dental research: a narrative review. Community Dent Oral Epidemiol. 2021;49(5):385-393. doi:10.1111/cdoe.12677
- Asimakopoulou K, Newton JT. The contributions of behaviour change science towards dental public health practice: a new paradigm. Community Dent Oral Epidemiol. 2015;43(1):2-8. doi:10.1111/cdoe.12131
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi:10.1186/1748-5908-6-42
- Atkins L, Michie S. Changing eating behaviour: what can we learn from behavioural science? Nutrition Bulletin. 2013;38(1):30-35. doi:10.1111/nbu.12004
- Mersha AG, Gould GS, Bovill M, Eftekhari P. Barriers and facilitators of adherence to nicotine replacement therapy: a systematic review and analysis using the capability, opportunity, motivation, and behaviour (COM-B) model. Int J Environ Res Public Health. 2020;17(23):8895. doi:10.3390/ijerph17238895
- Chan CCK, Chan AKY, Chu CH, Tsang YC. Theory-based behavioral change interventions to improve periodontal health. Front Oral Health. 2023;4:1067092. doi:10.3389/froh.2023.1067092
- Abreu-Placeres N, Newton JT, Pitts N, et al. Understanding dentists’ caries management: the COM-B ICCMS questionnaire. Community Dent Oral Epidemiol. 2018;46(6):545-554. doi:10.1111/cdoe.12388
- Atkins L, Michie S. Designing interventions to change eating behaviours. Proc Nutr Soc. 2015;74(2):164-170. doi:10.1017/S0029665115000075
- Newton JT, Asimakopoulou K. Minimally invasive dentistry: enhancing oral health related behaviour through behaviour change techniques. Brit Dent J. 2017;223(3):147-150. doi:10.1038/sj.bdj.2017.659
- Mitchie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. Silverback Publishing; 2014.
Over the last 12 years, Whitney Crist, RDH, CNC, CPT, CEAS, has become a noteworthy leader within the dental hygiene community. As a speaker, clinician, and adjunct faculty educator, she enjoys sharing her knowledge and passion for hygiene. She aids dental professionals in achieving pain-free work through her business endeavor, Dentistry Rebalanced. As a certified ergonomic assessment specialist, personal trainer, nutritional coach, and Essentrics instructor, Whitney brings a comprehensive approach to her mission. Contact her at [email protected].