In conversations with dental professionals about oral cancer screening, I often ask if they share information about the human papillomavirus (HPV) with their patients. The responses vary from “absolutely,” “sometimes,” and “I’ll never discuss HPV.” The most common response is “I want to, but I don’t feel confident.”
After learning about HPV-associated oropharyngeal cancer 16 years ago, I recognized it was my professional and ethical responsibility to share this information, but I lacked a strong knowledge of HPV and the confidence. Similarly, in a study published in the Journal of the American Dental Association, “The researchers found knowledge among oral health care professionals and students about the prevalence of HPV infection, modes of transmission, oral screening procedures, and the association between HPV infection and oropharyngeal cancer varied across studies.”1
Start somewhere
I wanted a comfortable way to share this critical information and had to start somewhere. My dad was a veterinarian, and he used the phrase, “what we know now” when sharing information with his clients. That became my intro to sharing about HPV, and it still is, when performing the oral cancer screening.
Here’s an example: “What we know now is that it’s not just tobacco and alcohol contributing to oral cancer. Now, the most common sexually [or intimately] transmitted infection, HPV, is the main cause of throat cancers.” If you are looking for a comfortable way to start sharing about HPV, use this or create something that feels comfortable to you. Start somewhere.
What we know now
According to the American Cancer Society, in 2024, approximately 58,450 Americans will be diagnosed with oral or oropharyngeal cancer. That’s approximately 160 diagnosed every day, and almost seven every hour. Approximately 33 Americans will die every day.2
The continual increase in these numbers is due to oral HPV infections, with HPV type 16 responsible for the majority of oropharyngeal cancers. Almost every American will be infected with HPV at some point in their lifetime. Oral transmission is through intimate skin-to-skin contact such as oral sex and deep kissing. Most cases of HPV will clear the body on their own; however, for some people, the virus lingers in the throat for years and can eventually cause cells in the lining of the throat to mutate and become cancerous.3
Persistent HPV infection
Should dental professionals be testing for oral HPV infections to help identify persistent infections, knowing that it is the lingering infections that can go on to cause cancer? Who should be tested, and what should be done if a test comes back positive for a high-risk HPV type?
This article looks at three oral HPV tests currently available. In researching the tests, I looked at six key points of each test: Who do they recommend be tested, how is the test performed, considerations for a positive HPV test and a negative HPV test, what HPV types are tested, and the sensitivity and specificity of each test.
FidaLab
How is the test performed? Gargle for 30 seconds with Scope mouthwash provided, expectorate into tube, and ship to FidaLab.
Considerations for a positive test: Dentist should perform a visual oral cancer screening to rule out the presence of any potential precancerous lesions and retest in six months to determine whether the HPV infection persists or has cleared.
Considerations for a negative test: No increased risk of developing oral cancer. Recommend annual visual oral cancer screening through the dentist and have annual oral HPV screening.
HPV types tested: HPV 16 and 18
Sensitivity: Detects 10 copies of HPV per reaction
Specificity: Detects HPV 16 and HPV 18, the main HPV types associated with oral cancer; no cross reactivity against other HPV types
OmniPathology throat HPV swab test
How is the test performed? Rub the provided swab over the palatine tonsils and oropharyngeal wall with a rotating, painting movement. Place swab in the provided vial. Ship vial in provided bag to OmniPathology. Results are typically received in 24 to 48 hours via email.
Considerations for a positive test: Perform a comprehensive exam and oral cancer screening. Retest in six to 12 months. If patient tests positive again, refer to ENT for further investigation. If retest is negative, test again in one year.
Considerations for a negative test: If the patient is high risk (multiple sex partners, immunocompromised, smoking, etc.) retest in six to 12 months. If the patient is not high risk, retest every year or every other year.
HPV types tested: 14 high risk genotypes, including HPV 16 and 18
Sensitivity: 95%
Specificity: 100%
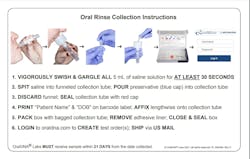
OraRisk HPV salivary test by OralDNA Labs
How is the test performed? Vigorously swish and gargle with saline solution for 30 seconds, expectorate the solution into the funneled collection tube, secure cap on the collection tube, and send sample to OralDNA Labs, shipping included. Email notification is sent to the clinician.
Considerations for a positive test: Test again in 12 to 18 months. If retest is positive, refer to an oral surgeon or ENT for further evaluation, and more frequent visits for oral cancer screening. Repeat HPV testing as necessary to determine if HPV infection is persisting or resolved.
Considerations for a negative test: If sexually active with more than one partner, retest in one year. After consecutive negative tests for two to three years, consider testing every three to five years.
HPV types tested: 24 high-risk types including HPV 16 and 18; 21 low-risk types including HPV 6 and 11; and seven unknown-risk HPV types.
Sensitivity: 5 to 10 viral copies per ml
Specificity: 100%
Who should be tested?
The three companies had similar recommendations on who should be tested: anyone who is sexually active or has multiple oral sex partners, someone who engages in oral sex, has a partner who recently tested positive for genital HPV, has high-risk factors such as smoking or is immunocompromised, or someone experiencing signs and symptoms of oropharyngeal cancer. For the specifics of each company’s recommendations on testing, please visit their website or reach out to them directly.
We are not winning the battle against oral and oropharyngeal cancer. Many cases are misdiagnosed as infections at the time of initial presentation, or given other benign diagnoses, and signs and symptoms are often ignored.
Patients who have tested positive for a high-risk oral HPV infection in the past or have been identified as having a persistent high-risk HPV infection would be more likely not to dismiss persistent signs and symptoms, and neither would their dental or medical professional. An immediate referral to the appropriate specialist for further investigation would be indicated.
Start somewhere. Have a team meeting and review your oral cancer screening protocols. Are providers calibrated in a comprehensive screening, and is an oral HPV test something to thoughtfully implement into your protocol?
Editor's note: This article appeared in the April/May 2024 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Casey SM, Paiva T, Perkins RB, Villa A, Murray EJ. Could oral health care professionals help increase human papillomavirus vaccination rates by engaging patients in discussions? J Am Dent Assoc. 2023;154(1):10-23.e17. doi:10.1016/j.adaj.2022.09.014
- Help us end cancer as we know it, for everyone. About oral cavity and oropharyngeal cancer. American Cancer Society. https://www.cancer.org/cancer/types/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html
- Oropharyngeal cancer. MD Anderson. https://www.mdanderson.org/cancer-types/throat-cancer/oropharyngeal-cancer.html
Susan Cotten, BSDH, RDH, OMT, is the owner of Oral Cancer Consulting and developed the “Cotten Method” of screening, a system that increases confidence in oral cancer screening and aids in reducing liability. Cotten is a speaker and provides hands-on oral cancer screening workshops. She is the dental lead for the Alliance for HPV Free Colorado, an RDH advisory board member for the Oral Cancer Foundation, and a 2018 Sunstar/RDH Award of Distinction recipient. Contact Susan at [email protected] or visit oralcancerconsulting.com.