Dental Implant Assessment
by Lynne Slim, RDH, MSDH
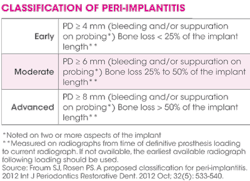
Consider this scenario -- Your dental hygiene patient enters the treatment operatory for a routine visit. She mentions that she has noticed bleeding from the area around her implant at the maxillary left lateral site. You take a periapical radiograph of the area. Upon probing, you note a 9 mm pocket. Bleeding on probing was also noted 15 seconds following removal of the probe, and the radiograph depicted bone loss › 50% of the implant length. The doctor (a general dentist) made the diagnosis of advanced peri-implantitis, and referred the patient to a periodontist, which was the right thing to do.
Before writing this column, I watched an American Academy of Periodontology DVD from the 99th Annual Meeting (Sept 28-Oct 1, 2013) and paid close attention to a lecture given to dental hygienists by Paul S. Rosen, DDS, MS, periodontist, on regenerative therapy. Part of his lecture included some comments on peri-implant disease (peri-mucositis and peri-implantitis) and I agreed with what he had to say. Peri-implantitis is always accompanied by bone loss, unlike peri-mucositis, which is a lot like gingivitis.
------------------------------------------------------------------------
Other articles by Lynne Slim:
------------------------------------------------------------------------
Sometimes as a clinician I'm sure I get sloppy, especially if I don't have adequate time or am distracted. We all get into a rut from time to time, especially when faced with the daily grind of a full schedule of adult recare patients. When presented with patients who have one or more dental implants, I pause and instrument around them differently, but sometimes, when pressed for time (and who among us isn't pressed for time as an RDH?), it is very difficult to perform a complete assessment. With these observations in mind, I've dedicated this column to those of you who want to take your implant assessment skills up a notch.
According to Dr. Rosen and all other periodontists I wrote to before beginning this column, early recognition of inflammation around a dental implant and good record- keeping are key to early identification of peri-implant disease. Peri-implantitis, once started, gallops at a rapid pace, according to Dr. Rosen, and needs to be assessed by a periodontist immediately.
Wingrove, in her new book on peri-implant therapy, emphasizes that RDHs play a key role as first responders in their ability to recognize potential dental implant complications.1 As problem-sleuths, RDHs can be on the lookout for implant complications such as mechanical and biological issues.
The most common mechanical consideration with implants is screw loosening in older screw-retained implants from the 1980s and 1990s. It was on the early external hex implants that screw loosening was a problem. The newer screw design systems have been improved and the internal hex connections have reduced the likelihood of the problem even more. Most of these cases can be mitigated by replacing the screws with a newer screw, which is designed to deform when torqued so they can "lock in." This makes them nonreusable but reduces the risk of loosening.
Biologically, peri-implant health occurs when there is no mobility, and ‹ 2 mm of radiographic bone loss from the initial surgery with no pain on function or history of exudate.2 From my reading about implant crown margins, it appears to me that little is known about the effect of implant crown margin positioning on surrounding peri-implant tissues; however, in some studies sulcular bleeding scores decreased as the location of a crown margin went from sub- to a supragingival position.3 In addition, cement-retained crowns revealed a higher degree of sulcular bleeding than screw-retained crowns. So, to all of us periodontal health sleuths, explore carefully around those subgingival implant crown margins!
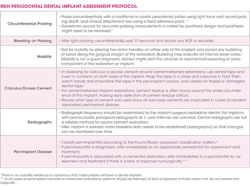
I've created a dental implant assessment tool (see above) for RDHs to copy/paste and use in everyday busy dental practices. It's my recommendation to you, my readers, as we begin another New Year.
Flap entry by a periodontist is often required to remove excess cement because these resin cements act like subgingival calculus/foreign bodies (see Figure 1).
LYNNE SLIM, RDH, BSDH, MSDH, is an awardwinning writer who has published extensively in dental/dental hygiene journals. Lynne is the CEO of Perio C Dent, a dental practice management company that specializes in the incorporation of conservative periodontal therapy into the hygiene department of dental practices. Lynne is also the owner and moderator of the periotherapist yahoo group: www.yahoogroups.com/group/periotherapist. Lynne speaks on the topic of conservative periodontal therapy and other dental
hygiene-related topics. She can be reached at [email protected] or www.periocdent.com.
References:
1. Wingrove S. (2013) Peri-implant therapy for the dental hygienist: clinical guide to maintenance and disease complications. John Wiley & Sons, Inc.
2. http://endoexperience.com/documents/Biofilm_Related_to_Dental_Implants8.pdf
3. http://www.landalatandlakarna.se/documents/Master%20studie.pdf
4. Froum SJ, Rosen PS. A proposed classification for peri-implantitis. 2012 Int J Periodontics Restorative Dent. Oct 2012; 32(5): 533-540.
Past RDH Issues