Hand Hygiene and Adverse Skin Reactions
It began on a Monday. Many bad things in life begin on a Monday. As usual, I washed my hands well and put on a pair of gloves. By mid-morning, I could start to feel my hands tingle. The sensation got worse as the day progressed. By late afternoon, my hands felt like they were on fire. What could be wrong? Last week, the office switched both handwashing soap and the type of gloves we used. The change was to improve the office “economy.” Could either or even both of the changes be causing my problem? Now what should I do?
The required personal protective equipment (PPE) is supposed to protect us, not make us ill or cause adverse reactions. This includes specialized clothing or equipment worn to protect against infectious materials or hazardous chemicals. As dental health care personnel (DHCP) we need to know what types of PPE are necessary for the varying procedures we are performing and how to use them correctly. It requires staff members to work together to make the selection and use of PPE both efficient and effective.
There are regulations and recommendations for PPE issued by OSHA and the CDC. OSHA creates workplace health and safety regulations called standards. These standards require that employers must 1) provide appropriate PPE for employees and 2) ensure that PPE is either disposable or if reusable is properly cleaned, laundered, repaired and stored. OSHA also specifies which PPE are indicated. The CDC recommends when, what and how to use PPE.
PPE - types and selection factors
There are five basic types of PPE used in healthcare settings. These are:
• Gloves - protect hands
• Lab coats/gowns/aprons - protect skin and/or clothing
• Masks and respirators - protect mouth/nose (respirators also protect the respiratory tract from airborne infectious agents)
• Safety glasses/spectacles/goggles - protect eyes
• Face shields - protect face, mouth, nose and eyes
A number of factors influence PPE selection. These include:
• Type of exposure anticipated (e.g., splash/spray versus touch)
• Allergies and sensitivities (to PPE construction materials)
• Design and features
• Durability (including shelf life)
• Sizing or fit (comfort)
• Cost effectiveness
Compliance concerning PPE is often dependent on personal preferences. However, increased comfort (better fit, ergonomics, allergies and body temperature regulation) usually translate into higher levels of compliance.
Being alert to adverse reactions
Even though PPE is used to protect, there are instances when wearing PPE becomes problematic. Adverse reactions may occur. It is important for DHCP to be able to identify symptoms associated with these reactions and then be able to respond accordingly.
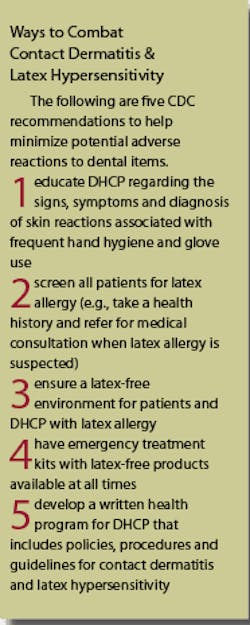
Intact skin is an efficient barrier to microbes and many chemicals. This ability can be lost if skin becomes damaged by exposure to chemicals present in PPE and during hand washing. The CDC in their Guidelines for Infection Control in Dental Health Care Settings - 2003 has offered advice on how to deal with adverse reactions (see sidebar).
There are three main types of adverse reactions to PPE and other dental items - irritant contact dermatitis, allergic contact dermatitis and immediate hypersensitivity.
There are many types of reactions in dentistry related to glove use. Most of these reactions, however, are cases of irritant contact dermatitis (ICD), which is a condition due to non-immunologic irritation from chemicals. ICD presents as dry, itchy, irritated areas of skin around the zone of contact with the offending agent. ICD compromises healthy skin and increases the chances of materials entering the blood stream.
ICD can become aggravated by: 1) failure to wash hands after removing gloves; 2) not rinsing thoroughly after handwashing; 3) not drying hands completely before donning gloves and 4) contact with irritating hand cleaners.
The best way for DHCP to deal with ICD is through proper hand hygiene. For example, thorough rinsing after handwashing reduces contact with chemicals present in gloves and handwashing agents. DHCP are tempted to change the glove type when problems arise. It is important to first determine if the new brand is actually different than what is currently being used as manufacturers sell the same glove under several different brand names.
Allergic contact dermatitis (ACD) occurs after contact with chemicals that serve as allergens. This stimulates a cell-mediated immune response. ACD unlike ICD involves an immunological response, which is often called “delayed hypersensitivity” or “type IV hypersensitivity.” A non-dental example of the the cause of ACD is the allergic oils present in poison ivy plants.
ACD reactions occur 48 to 72 hours after the second or subsequent contact with an allergen. ACD is confined mainly to the area of contact. It is characterized by an initial itching, redness and vesicles which are followed by dry skin, fissures and sores.
ACD is not always easy to diagnosis. ACD can be the result of contact with many types of chemicals used in glove manufacturing, bonding agents, antiseptics, disinfectants, sterilants, hand-care products, adhesive used in masks and other materials commonly present in dental offices. Some chemicals can penetrate glove materials, especially those used to make clinical use gloves.
In order to improve the situation, a correct diagnosis and identification of the allergen must be made. Testing may include skin patch tests, other skin tests or even blood screening. This is followed by treatment and avoidance of the identified allergen, as ACD can recur or become chronic following repeated allergen contact.
After a correct diagnosis is made, treatment must be delivered by a trained physician and should never be delayed. It is important to identify the causative allergen, such as latex, because this allergen may also be present in a variety of other products.
Immediate hypersensitivity, type I hyper-sensitivity, is another type of immunological reaction, which involves an antibody response. Latex can be one of the allergens involved with adverse responses. Immediate hypersensitivity can be serious, sometimes even life-threatening.
After an initial exposure to an allergen, special IgE antibodies are generated which react with mast cells and basophils. The affected person has now been “sensitized,” but initially there may be no symptoms. During subsequent exposures the offending allergen binds directly to mast cells with the release of powerfully active quick acting chemicals.
Reactions may be localized or systemic and include skin changes such as hives, redness, burning or itching. More common reactions include respiratory symptoms such as sneezing, watery and itchy eyes or asthma, which may result in difficult breathing, coughing or wheezing. Sometimes cardiovascular and gastrointestinal symptoms occur. In rare cases when allergens enter the bloodstream and contact sensitized basophils, anaphylaxis develops.
DHCP must be prepared to provide emergency medical care when someone experiences a rapid onset of a systemic allergen reaction involving either the cardiovascular or respiratory system. Procedures to summon immediate medical care must be in place.
Latex hypersensitivity
As discussed earlier, one important cause of immediate hypersensitivity is latex. You can be allergic to natural rubber latex allergens present in PPE. Glove manufacturers have attempted to reduce the amount of latex allergens present in their products, which are labeled as “low protein” products.
Once sensitized, wearing gloves is not always required for a reaction to occur. Cornstarch present on latex gloves can contain allergens. Cornstarch particles can become airborne during use, donning or removal and the allergens can then be inhaled. Powder-free gloves will reduce the airborne release of these proteins. In addition to gloves, latex allergens may be present in many other materials and equipment used in dental practices. Some examples include disposable prophy angles, rubber dams, masks and stoppers in anesthetic carpules.
Taking proper patient and DHCP medical histories with frequent reviews will help reduce reactions. If someone is truly latex hypersensitive, avoiding latex containing items, including gloves is essential.
Keeping hand healthy
Hands are among the greatest tools DHCP possess and intact skin is the best barrier against infectious microorganisms and some chemicals. When skin is irritated and inflamed, its natural barrier properties are compromised and allergens can more easily penetrate. Inflamed skin often contains high numbers of microorganisms and handwashing does not readily remove bacteria from irritated skin. For best protection, it is important to keep hands and skin healthy. The following are methods that could reduce the chances of irritated skin.
• Always rinse and dry hands thoroughly after handwashing.
• Avoid bare handed contact with sensitizers and irritants
• Be wary of chemicals that can permeate glove materials
• Wear chemical and puncture resistant utility gloves when handling hazardous chemicals
• Use hand creams that are compatible with antiseptic products and glove materials (petroleum and other oil-based ingredients can degrade some glove materials, such as latex)
• Use protective gloves at work and at home
Using alcohol hand rubs
In 2002, the CDC released a guideline on hand hygiene in which there were references to the use of alcohol-based hand rubs (preparations containing 60% to 95% alcohol). These products have been shown to be effective and may improve hand hygiene compliance. The CDC guideline states that alcohol-based hand rubs significantly reduce the number of microorganisms on skin, are fast acting and cause less skin irritation than antiseptic containing soaps or detergents.
Alcohol rubs are appropriate when hands are visibly clean. For routine handwashing or hand antisepsis apply the correct amount of product into the palm of one hand and rub hands together, covering all surfaces of the hands and fingers. The amount applied varies by manufacturer. Your hands should feel dry after 10-15 seconds of rubbing, allow the rub to dry completely prior to placement of gloves. Some alcohol-based hand rubs can be used for surgical hand asepsis. These have persistent - prolonged or extended antimicrobial activity that prevents or inhibits the proliferation or survival of microorganisms. The hands and forearms must first be washed with a non-antimicrobial soap and water and thoroughly dried. Then, a surgical hand rub is applied, rubbed in well and allowed to dry prior to gloving. Most alcohol-based hand rubs used in the United States contain 60% or greater percentages of ethyl alcohol or isopropyl alcohol. Since alcohol is a flammable liquid, proper use and storage of all alcohol-based hand rubs is essential.
Final thoughts
While the benefits of PPE and hand hygiene cannot be overstated, adverse reactions can develop as a result of exposure to chemicals and frequent and repeated handwashing. Although adverse skin reactions occur frequently among DHCP, fortunately true allergic responses are uncommon. It is important to have a correct diagnosis and treatment by an allergist or dermatologist.
Now back to my troubled hands. Thanks to working with a knowledgeable allergist, we were able to eliminate, one-by-one, the suspected offending culprits and make an accurate diagnosis. As it turned out, a change to a powder-free nitrile glove solved my problem. Thanks to these professionals I did not have to make a midlife career change after all. Oh, by the way, I quit working Mondays. It just seemed easier that way.
Hand hygiene
There is substantial evidence that hand hygiene reduces the incidence of infection. DHCP handwashing is a simple, elementary procedure that is essential to reduce patient post-treatment infections and occupationally acquired infections. Traditionally, hand hygiene was accomplished through basic handwashing, which suspends microorganisms and mechanically removes them by rinsing them with water, or kills microorganisms when a soap containing an antimicrobial ingredient is used.
Hand hygiene can be divided into three categories: routine handwashing, routine hand asepsis and surgical hand asepsis.
Routine Handwashing
Purpose: Remove soil/dirt and transient microorganisms
Procedure: Use a non-antimicrobial soap or detergent and water for 15 seconds1
Agents: Plain liquid soap dispensed using a hands-free device; avoid the use of soap bars
Advice: Use routine handwashing techniques when: 1) hands are visibly soiled or contaminated with materials such as blood or other body fluids; 2) before and after treating patients (before gloving and after removing gloves); 3) when touching barehanded objects known or likely to be contaminated with blood or saliva; 4) before replacing defective gloves and 5) before leaving the operatory or laboratory (e.g., before eating and after using the restroom)
Routine Hand Asepsis
Purpose: Remove or destroy transient microorganisms; may negatively affect resident flora
Procedure #1: Use an alcohol-based hand rub; add proper amount to dry hands and then rub hands until alcohol has evaporated (hands, fingers and forearms are dry); use products with known persistent activity2
Agents for Procedure #1: Most commonly contain 60% to 95% ethanol or isopropanol or combination of alcohols; emollient additives, gel medium and antimicrobial agent such as chlorhexidine, quaternary ammonium compounds, octenidine or triclosan
Procedure #2: Use a nonantimicrobial soap or detergent and water for 15 seconds1
Agents for Procedure #2: Examples of active agents include alcohols, chlorhexidine, chlorine, hexachlorophene, iodine, chloroxylenol (PCMX), quaternary ammonium compounds and triclosan
Advice: Use Procedure #1:1) when hands are not visibly soiled or contaminated with blood or other body fluids (routine decontamination of hands in clinic situations); 2) before and after treating patients (before gloving and after removing gloves); 3) when touching barehanded objects known or likely to be contaminated with blood or saliva; 4) before replacing defective gloves and 5) before leaving the operatory or laboratory (e.g., before eating and after using the restroom)
Surgical Hand Asepsis
Purpose: Remove or destroy transient microorganisms and reduce resident flora with proven persistent agent effect
Procedure #1: Use water and antimicrobial agent or detergent and scrub for 2 to 6 minutes - use agents capable of producing a persistent antimicrobial effect
Agents for Procedure #1: Examples of active agents include alcohols, chlorhexidine, chlorine, hexachlorophene, iodine, chloroxylenol (PCMX), quaternary ammonium compounds and triclosan
Procedure #2: Use a non-antimicrobial soap or detergent and water for 15 seconds and dry hands and forearms completely, follow with the use of a surgical alcohol-based hand rub; add proper amount to dry hands and then rub hands until alcohol has evaporated (hands, fingers and forearms are dry); use products with known persistent activity2
Agents for Procedure #2: Liquid soap dispensed using a hand-free device; avoid the use of soap bars; dry hands and forearms, then use products that contain 60% to 95% ethanol or isopropanol or combination of alcohols; emollient additives, gel medium and antimicrobial agent such as chlorhexidine, quaternary ammonium compounds, octenidine or triclosan
Advice: Used prior to placement of sterile surgeon’s gloves in preparation for surgical procedures
1 process involves vigorous, brief rubbing together of lathered hands and fingers, followed by an adequate rinse, then hands should be thoroughly dried
2 apply prescribed amount to the palm of one hand and rub together covering all surfaces of hands and fingers until skin surfaces are dry