Calming the stressed-out grinder
by Sonya L. Prater, RDH, BS, FACE
It’s one of the worst sounds ever — like fingernails on a chalkboard. Popping or clicking while you’re chewing, teeth worn down to nubs, and pain in the jaw are all signs and symptoms of bruxism.
The dental field has become so complex (in some respect) that sometimes it’s just easier to do the same old stuff we’ve been doing for years and overlook the new forms of treatment. Bruxism is not a new “disease,” but it plagues so many people and is left untreated most of the time.
About two years ago, I realized there were more options out there for treating bruxism. For years, I thought there must be a solution for TMJ issues, and I didn’t believe eliminating stress was the cure. If so, there would never be a cure. It has been exciting for me to be exposed to different forms of treatment. Relief for bruxism is available.
The most interesting thing about bruxism or “grinding” is that few people think they are victims. Most of the time, patients will present a list of symptoms, and I see the the evidence in the mouth. But nine times out of 10, they say, “I don’t grind my teeth.” That is like saying, “I don’t have dreams.” We are asleep when those events occur, and we are unaware that it is happening. The truth is that most who grind at night will do the same in the daytime.
What does bruxism mean? The term is of Greek origin and is simply defined as “gnashing of teeth” — characterized by grinding and often accompanied by clenching. Clenching will often occur while awake. Grinding usually occurs during sleep, even during catnaps.
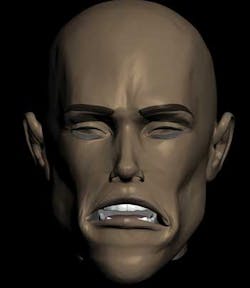
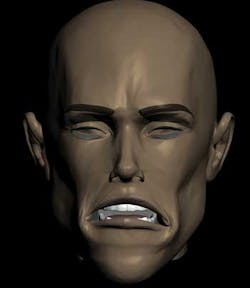
Figure 1 (above): An example of heavy wear.
Many times this condition will be accompanied by symptoms, but not always. I encounter patients on a daily basis who have all the signs but little to no symptoms — at least for now. Convincing them that they are grinding their teeth is often pointless. If their spouses have never mentioned it, and they believe their teeth have always been “flat” or “short nubs,” then you will have very little success in convincing them to pursue treatment for what seems to be a nonexistent problem. Unless there is pain or a potential cosmetic concern related to the issue, and you can convince them that you can get rid of the pain or improve esthetics, there is often little interest in treatment.
Signs/symptoms
Bruxism or grinding involves three major components: teeth, muscles, and joints. With teeth, the obvious signs are displayed in the wear of teeth — a flattened appearance and abfractions (see Figures 1, 2). Abfractions are notched-out areas at the CEJ. This happens when the tooth has flexed so much during the grinding process that the root surface begins to break down and form a scooped-out appearance. It is a mechanical failure of the tooth structure.
Figure 3: A display of the TMJ without any muscle covering. Imagine manually manipulating the jaw to allow the teeth to slide against each other. That is what the muscles have power to do, which in turn causes grinding.
Conditions that can develop from grinding/clenching can encompass sensitivity, fractures, mobility, and possibly root canal therapy. If your job for several hours every day was to take a sledge hammer and beat the side of a very structurally sound, brick building, what would happen? Eventually it would weaken, causing the bricks to break or fracture, in turn lessening the stability of the structure and leading to the eventual need for repair. Constantly pounding teeth or sliding them back and forth is not what they were originally designed to do. Yes, they manage the pressure of chewing, tearing, and biting into food. But when they encounter forces beyond their functional capacity, teeth will always lose and begin to break down, likely requiring restoration in the future.
Figure 4: An example of someone who has a deep overbite and is considered “overclosed.” This person has a partial that does not adequately open up her bite.
Muscle deterioration can require treatment outside of the dental field. Neuromuscular massage therapy is a good way to restore muscles back to health. What happens in the grinding/clenching process is that the muscles begin to shorten and tighten up.
As a practitioner, unless you practice ergonomic dentistry, head, neck, and shoulder muscles tighten up on a daily basis. How many of us allow our muscles to relax and be restored to their resting length on a regular basis?
Clenching and grinding for your head and neck muscles is like working out for hours on end. If you were to work your left bicep muscles every day, leaving your right arm muscles at constant rest, there would be an imbalance in everything you do. For example, your right arm would have to work harder when picking up a box as opposed to your left arm, thus straining other muscles on that side of the body. This would cause the normal physiological balance of the human body to break down. Muscles tend to “heal” or normalize fairly quickly with proper treatment.
I get a kick out of hearing patients tell me they have “TMJ.” I always want to answer back with excitement, “So do I!” Or better yet, when they tell me they don’t have TMJ. Instead, I gently educate them on what “TMJ” actually is (see Figure 3). We have now introduced the term TMD (also seen as TMJD) — temporomandibular disorder (or temporomandibular joint disorder) to alleviate some confusion.
The breakdown of the jaw joints can be a serious problem. If left untreated for many years, permanent damage can result, untreatable even through surgery. These joints allow the jaw to open and close on an articulator disc (made up of fibrous cartilage) that is positioned between the two bones that form the joint — the temporal bone and the mandible. During the grinding process, muscles are pulling the jaw in a direction that continues to stress the components of the joint. If the articulator disc is consistently forced from its natural position, over time it can cause permanent damage to either the discs or the ligaments that hold it in place and be quite painful.
Causes of bruxism/bite problems
The main issues related to bite problems are:
- The mandible being in the wrong position when the teeth come together
- An imbalance of how the teeth meet when they do come together
- Chewing interferences
- A worn, torn, or compressed joint.
These issues can arise due to several reasons.
Growth and development — Some issues just happen as children or during growth. Infected tonsils, adenoids, allergies, and early dental treatment are just a few causes that can lead to adult TMD.
Missing teeth — Missing teeth change the way patients bite and chew. A second molar extracted on the right side will lead a patient to favoring the left side when chewing. The alteration of the once normal chewing/biting pattern forces the teeth to find a “new” pattern, which in turn can cause a grinding issue. The main culprit is that the teeth shift from a functionally neutral position, and an imbalance is created.
Malaligned teeth — Malaligned teeth can be due to unsuccessful orthodontics in positioning the mandible and/or crowding when the teeth first erupt, tooth movement, or when teeth supererupt from lack of an opposing tooth. If there is any interference when the muscles and joints are trying to position the teeth in a position that feels right, it can trigger the act of grinding. The idea is that the tooth/teeth that are in the way will be forced out of the way by grinding them down, so the teeth no longer pose an interference. The teeth dominate, and the muscles accommodate.
Airway issues — If someone has a deep overbite, they are considered to be “overclosed” (see Figure 4). When teeth are “overclosed,” there is not much room for the tongue to lie in the floor of the mouth and it closes up much of the airway. This can cause grinding. The teeth then try to find a position that helps to open the airway. Airway issues are not always related to grinding, but it is a factor that should be considered.
Restorative work — Patients often call back a few days after receiving a new filling or crown, stating that “it feels too high.” If this is left uncorrected, it can lead to grinding. The teeth know what position they want to be in, and if the position is altered, the muscles and joints will work hard to get them back into the previous position, resulting in bruxism. Unfortunately, more teeth, muscles, and joints will be affected when this happens.
Treatment options
The three main schools of thought are centric occlusion (CO), centric relation (CR), and neuromuscular dentistry (NM). Sometimes the CO/CR relationship is considered a combined theory.
Centric occlusion is defined as an interocclusal position of the maxillary to mandibular teeth. The maxillary cusps have a certain occlusal relationship with the mandibular cusps. Centric relation is defined as the position of the condyles in relation to the glenoid fossa when the jaw closes.
Forms of treatment for centric relation and centric occlusion usually include manual manipulation of the mandible to get the teeth to fit in what is considered their proper position, or for the jaw to be in its proper relationship. Bite adjustments (selective grinding) or orthodontics is generally the recommendation in order to accomplish such relationships. Several forms of mouthguards can also be used, ranging from ones that protect teeth against further wear to those that actually position teeth in such a way that only certain ones touch.
Neuromuscular dentistry is much more complex, and the muscles, teeth, and jaw all are involved. In this school of thought, everything works together in the musculoskeletal system in order to create balance. If left unbalanced, it can throw off everything, the bite included.
Forms of treatment can include minimally invasive options to extreme makeovers. Technologically advanced scans are used to determine where the correction needs to take place. Bite equilibration, orthopedic jaw positioning devices/orthotics, and full-mouth reconstruction (rebuilding a proper bite with crowns so that teeth fit together properly in a healthy jaw relationship) are all forms of treatment used in NM dentistry. NM dentistry actually measures the problem and a computer visualizes how to properly address the problem.
With NM dentistry, the dental profession itself is not the “cure all” for all aspects of treatment. NM dentists have a referral system with NM massage therapists, as well as chiropractors, who all work together for the common goal of thoroughly treating a patient. Because of its complexity and the extensive education required, this type of dentistry is practiced by very few dentists, but the trend is for the profession to move in the direction of NM dentistry.
When patients tells you they experiencing pain or discomfort due to the symptoms discussed in this article, the patient should be referred to someone who can help, if the primary office declines to treat. We have a responsibility to treat and not to ignore.
Don’t be the hygienist who has treated a patient for 30 years, and the patient is now considered disabled because of frequent migraines, popping/clicking with every bite, and can now open the mouth only halfway during the appointment. There is relief from bruxism! Give these patients hope and a better quality of life. Don’t let bruxism stress out the grinder; instead, stress that there is treatment for the grinding!
Sonya Prater, RDH, BS, FACE, is practicing full time in Savannah, GA, in a very progressive dental office, Beyond Exceptional Dentistry. The practice specializes in highly complex and reconstructive TMD cases. She is also a faculty member/instructor for The Niche Practice Seminars, the hygiene consultant for KOMET USA, and seizes every opportunity to further her education in as many areas as possible.