Demystifying root canals: Educate your patients about restorative dentistry in just a few minutes
By Jannette Whisenhunt
I was lucky to start out as a dental assistant and work for some wonderful dentists, which allowed me to watch and assist with fillings, buildups, and crowns for three years. I became familiar with the "restorative side" of dentistry, but I know this is not the case for all dental hygienists. New hygienists sometimes struggle with answering patients' questions about restorative dentistry because it is covered minimally in school. Most of this knowledge can be picked up once you start working, depending on the time you have to watch dental procedures in the office. Many patients with restorative needs are transferred from the hygiene side of the practice, so hygienists often have the opportunity to help patients make correct decisions about what they need done.
Since restorative procedures can seem foreign to new hygienists, I want to use the next few months of columns to explain the basics of educating patients about common dental procedures on their treatment plans-and how to do so in only a few minutes since we don't always have time for long explanations. This month, I will focus on answering the question: "What is a root canal, and will the tooth turn darker?"
OK, let's try to explain this procedure to our patient: A root canal is needed when the soft tissue inside the tooth (pulp) gets infected and causes pain and pressure. The infection usually occurs due to decay or trauma to the tooth. The pulp contains the blood vessels and nerves-it's what keeps the tooth "alive" and gives it the capacity for sensation. The infection in the pulp causes pressure to be released at the end of the root and can cause an abscess, which can often be seen as a dark circle at the end of the root on an x-ray. The tooth can also be sensitive to heat, cold, and pressure during chewing and can become extremely painful, sometimes causing the jaw to swell.
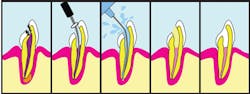
Some general dentists do root canals, but many are performed by endodontists (a dental specialist). During a root canal, the pulp is taken out of the inside of the tooth, but the tooth can be saved! The inside of the tooth is cleaned, sterilized, and filled with a sterile material. Then, a filling is placed in the top of the tooth, and the tooth is restored to function.
Having a root canal will save a tooth that, in the past, might have been extracted. You will be able to chew on the tooth again, but following the root canal, the tooth may become more brittle because it is drier without the pulp. This can cause the tooth to appear grayer and slightly darker over the course of a few years, and the brittleness can cause the tooth to split, creating the need for it to be extracted. To protect the tooth after a root canal, it is extremely important to have a crown placed on the tooth.
A root canal can be an expensive treatment, depending on the number of roots the tooth has, but it is worth trying to save the natural tooth. An extraction causes an empty spot in your smile, and a plastic replacement with a partial denture is never as good of an option. The dentist will probably put you on an antibiotic for the infection and maybe a pain medicine, if needed. The procedure usually requires two visits. After it is over, the filling will be placed in the top of the tooth and the decision about covering it with a crown can be made.
You may also need to have the prices for the procedures readily available for the patient so he or she will know the cost and whether it will be covered by insurance. The front office staff or office manager can provide this information for you.
I hope this quick "dentistry bite" has helped you learn how to describe this procedure to your patients. Root canals have a bad rap among patients. You always hear the horror stories about the rare few that don't go well, but you never hear about the successful ones that happen every day. This can cause patients to be afraid, but we can help alleviate those fears and help them to take ownership of their dental health with good patient education. It takes only a few minutes to help a patient understand what needs to be done to save a tooth.
I encourage you to watch some dentistry in your office when you have free time and ask your dental assistant questions about the procedures that you don't understand. You can learn a lot from these valuable professionals. You can do this-we can talk to our patients about more than flossing, and it can be exciting for us to learn more about dentistry, too. Have a great month, and happy scaling! RDH
Jannette Whisenhunt, RDH, BS, MEd, PhD, is the Department Chair of Dental Education at Forsyth Technical Community College in Winston-Salem, N.C. Dr. Whisenhunt has taught since 1987 in the dental hygiene and dental assisting curricula. She has a love for students and served as the state student advisor for nine years and has won the student Advisor of the Year award from ADHA in the past. Her teaching interests are in oral cancer, ethics, infection control, emergencies and orofacial anatomy. Dr. Whisenhunt also has a small continuing education business where she provides CE courses for dental practices and local associations. She can be reached at [email protected].
References
1. Bird DL, Robinson DS, Behrens A, Torres HO, Ehrlich AB. Modern Dental Assisting. 10th ed. St. Louis, MO: Elsevier Saunders; 2012.