Is it an aphthous ulcer or lip cancer?
Susan P. Burzynski, MSEd, RDH, FAADH
I have had several patients present with aphthous ulcers. We should all be performing oral cancer exams, but do you examine the lips as well as the intraoral cavity? Do you know the difference between lip cancer and an aphthous ulcer? Do you know what causes aphthous ulcers and lip cancer?
Aphthous ulcers
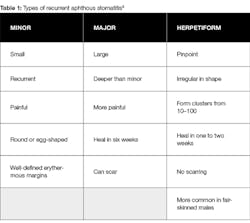
Recurrent aphthous stomatitis (RAS), or aphthous ulcers, is a common ulcerative inflammatory condition of the mouth. Patients usually begin developing RAS in their early teen years, and the condition can continue into their adult lives. There are three types of RAS: minor, major, and herpetiform1 (table 1).
There are many causes of RAS. It can be caused by stress, biting the inside of the cheek, family history, food allergies, spicy foods, and even toothpaste or mouthwash that contains sodium lauryl sulfate. Diets lacking in vitamin B12, zinc, folate, or iron can cause RAS, as can the bacteria found in the oral cavity, such as Helicobacter pylori, which is the same bacteria that causes peptic ulcers. Finally, inflammatory diseases, celiac disease, Behcet’s disease, and HIV/AIDS can cause RAS.1
There are no tests to diagnose RAS. To help prevent it, encourage your patients to choose a healthy lifestyle and practice good oral hygiene habits. You can attempt to find the underlying cause—for example, stress—and encourage the patient to eliminate or reduce the stressor.2
Cancer of the lip
Cancer of the lip is caused by an oncogene, a gene that has the potential to cause cancer.3 Despite being the most malignant neoplasm, it is the most overlooked type of nonmelanoma skin cancer (NMSC). Statistics reveal that .06% of cancers are lip cancers, and that lip cancers are the second most common malignancy of the head and neck.4
The most common skin cancers are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). SCCs are generally found on the lower lip with a possibility of neck metastases. BCCs are generally found on the upper lip and usually do not metastasize to the lymph nodes.3 The Memorial Sloan Kettering Cancer Center states that common symptoms of lip cancer include a sore on the lip that does not heal, a lump on the lip or a thickening of the lip, and bleeding, pain, or numbness of the lip.
Research shows that if a patient’s occupation involves sun exposure (90% of NMSCs are caused by UV exposure), or if the person uses tobacco—including smokeless tobacco—and alcohol, the person has an increased chance of developing lip cancer.
© Vampy1 | Dreamstime.com
Kidney transplant patients have a 30 times greater chance of developing lip cancer due to their need to take immunosuppressive antirejection drugs. Being fair skinned and having a light complexion are risk factors. HPV is not currently found to be a major cause of lip cancers; however, HIV-positive patients have a higher risk of developing skin cancer.4
The rate at which lip cancer can be cured is very good, and the recurrence-free survival rate is 90%. Early detection is crucial. Early stages exhibit with an area of crusting, with leukoplakia or erythroplakia in the mucosa, and with advanced areas of bleeding and disfigurement.3
According to the Head and Neck Cancer Guide, doctors use the American Joint Committee on Cancer (AJCC) TNM system to determine the stage of lip cancer. The following three factors are considered when staging: “T”—characteristics of the main tumor mass, “N”—status of the lymph nodes in the neck, and “M”—status of cancer spread (metastasis) to parts of the body outside of the head and neck.
The “T” stage is decided at the physical exam appointment. There are eight stages from the time the doctor assesses the primary tumor (Tx) to the time the mass is an advanced local disease and invades the masticator space, pterygoid plates, base of the skull, or encases the carotid artery (T4b). The “N” stage is after review of the information is collected and ranges from the neck lymph nodes cannot be assessed (Nx), to the cancer has spread to one or more neck lymph nodes and the node is larger than 6 cm (N3). The “M” stage deals with the spread of the cancer outside the head and neck and can go from no evidence of distant spread (M0) to evidence of spread outside the head and neck, for example, to the lungs or brain (M1).
Early detection of lip cancer allows for surgery, radiation, or cryotherapy, and the relapse rate is 5% to 35%. According to the Skin Cancer Foundation, the most common cure for lip cancer is Mohs micrographic surgery. During this surgery, thin layers of skin are removed and examined microscopically. Should more cancerous cells be found, more tissue is removed until no cancer is evident.
As research shows, it is important for us to do the extraoral exam on our patients and to know the difference in the pathology that we see. Instruct patients to call your office should a site not heal in one to two weeks. If the patient calls and reports that the site has not healed, refer the person to an oral surgeon.
References
1. Canker sore. Mayo Clinic website. https://www.mayoclinic.org/diseases-conditions/canker-sore/symptoms-causes/syc-20370615.
2. Thoppay J. Aphthous ulcers. Medscape website. https://emedicine.medscape.com/article/867080-overview. Published April 24, 2018.
3. Moretti A, Vitullo F, Augurio A, Pacella A, Croce A. Surgical management of lip cancer. National Institutes of Health website. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3146335/. Published February 2011.
4. Stebbins W, Hanke CW. Lip cancer: Not uncommon, often overlooked. Skin Care Foundation website.https://www.skincancer.org/skin-cancer-information/lip-cancer-not-uncommon.
Susan P. Burzynski, MSEd, RDH, FAADH, received her associate degree from Erie Community College, and her bachelor’s and master of general education from Canisius College in Buffalo, New York. She was awarded the Sunstar/RDH Award of Distinction in 2010, a fellowship from American Academy of Dental Hygiene in 2011, and Excellence in Leadership in 2013 from the New York State Dental Hygienists’ Association. Besides working in clinical hygiene full-time, Susan writes numerous articles for hygiene magazines, served as a key opinion leader for various dental companies, and serves as a volunteer for veterans.