Welcome
One of the most challenging aspects of any dental practice is managing patient appointments. Office policy varies from practice to practice, yet the situations encountered with managing patient appointments seem to be universal.
Other industries use management systems to assist them with the way they do business. In this article, we'll examine using this type of an approach with patient appointments.
A management system defines what an organization does to manage its processes or activities, such as managing patient appointments. It inherently incorporates risk-management strategies in documents such as "standard operating procedures" and forms. Documentation helps ensure a standard approach to the way an organization goes about its business.
A system has the added value of reducing the risk of omissions or wrong decisions, ensuring that everyone is clear about who is responsible for doing what, when, how, why, and where. A management system makes you think about your objectives and processes.
Every office has objectives in managing appointments, even if they are unstated. Most are inherently part of the office culture and are achieved without conscious effort. However, the lack of a documented system often can lead to complacency. Objectives include, but are not limited to, the following:
- Fill all available time slots
- Match patient requirements with the office's competencies and capabilities
- Minimize risk of patient no-shows, rescheduling, and cancellations
- Minimize risk of office-initiated rescheduling
- For patients who present without an appointment, minimize the ris of them being recorded in the scheduler
- Keep the scheduler accurate and up-to-date on a real-time basis
- Make the patient's overall visit a pleasant experience. This includes efficient appointment management
- Learn from patients comments, and adjust the system as necessary
Responsible office managers need to review objectives periodically to ensure that they still are adequate and suitable. The process for achieving these objectives should be practical, realistic, and effective.
An area of risk exposure indicates a potential for something to go wrong in a process. The challenge is to identify what potentially could go wrong (or has gone wrong), and then decide what actions can be taken to control and minimize the risk of occurrence or recurrence.
After identifying a risk, staff members should assess it to determine its likelihood of occurrence, frequency of occurrence, and the consequences of occurrence. This does not need to be a long, drawn-out, formal process. Any corrective or preventive action taken should be appropriate to the magnitude of the problem and commensurate with the risks encountered.
What follows are descriptions of some areas of identified risk exposure and examples of strategies to deal with them.
New patients
Risk 1: Not getting accurate and correct information needed for the treatment of the patient, including relevant medical history.
Strategy 1: Provide a standard form with questions and prompts. Include guidelines to assist staff in obtaining information that might be critical in managing appointments.
Risk 2: Not familiarizing the patient with office policy regarding appointments.
Strategy 2: Have staff brief the patient on office policy. This is done in a standard manner so that all patients are told the same thing.
Queries other than appointments
Risk 1: Providing the patient with the wrong information or not processing the patient query in a prompt and efficient manner.
Strategy 1: Staff should promptly establish the reason for the patient query. Ensure that staff know who is responsible for processing different types of patient queries, such as questions about insurance.
Matching patient requirements (appointment scope) with office competencies and capabilities
Risk 1: Having the patient come in for an appointment without suitable, qualified personnel available to address patients' needs/requirements. This also applies to having the necessary equipment available for the appointment.
Strategy 1: Staff must ensure appropriate appointment slots are available that match patient requirements and office capabilities. It should be noted that the patient's technical requirements (dental treatment needed) are normally determined by the dental practitioner, rather than the patient. The patient presents with symptoms that the clinical staff translates into a particular condition with an associated treatment.
The patient may provide input into requirements if given treatment options by the practitioner. The patient has more control of timing (appointment-scheduling) re quire ments, although this also may be limited by the urgency of the treatment and available appointment slots.
Appointment cancellations and rescheduling
Risk 1: Patient cancels with sufficient notice (per office policy).
Strategy 1: Reschedule appointment. Attempt to determine reason for need to cancel, but be sensitive in doing this.
Risk 2: Patient cancels without sufficient notice (per office policy).
Strategy 2: Advise patient of office policy and explain importance of appointment. Attempt to determine reason for need to cancel, but be sensitive in doing this. Reschedule appointment (see "Patients with attendance problems" below).
Patients with attendance problems
Risk 1: Making an appointment with a patient who is chronically late, has many last-minute cancellations, or repeatedly does not show up for appointments.
Strategy 1: This is a problem common to other industries, including airlines, hotels, and restaurants. Some of their strategies include issuing non-refundable ticketing, obtaining advance deposits or credit card guarantees that are not refundable after a certain time, and canceling reservations if a confirmation call is not returned. Establishing office policy addressing this topic is necessary to ensure a fair and equitable outcome.
Specific strategies may include an "A, B, C" patient-rating system, where A's are reliable, B's are questionable, and C's are those patients you'd rather not have in your practice. If you adopt this type of strategy, you must have clear rules about changing a patient from one rating to another, including who has authority to make changes. An example of the application of this strategy would be only seeing "B's" on a standby basis, such as when there is a cancellation.
Note: Chronic attendance problems blamed on forgetfulness by the patient may indicate another medical condition. Office staff should bring these cases to the attention of the clinical staff, who may decide to refer the patient for alternative medical help.
Scheduler is not accurate and up-to-date
Risk 1: Staff members do not change the scheduler on a real-time basis.
Strategy 1: Establish a process for ensuring that the scheduler is accurate and up-to-date. Verification strategies may include initialing appointment cards when scheduler changes are completed. (Note: This is not intended as a check on who did this; it is only done to ensure that necessary actions were completed.) In addition, don't permit a "hand over" in the middle of a change; the person who starts the transaction must be the one who finishes it.
Risk 2: Clinical staff are not aware of changes made to schedules.
Strategy 2: When front-desk personnel make changes, they must go to each operatory and modify schedules so clinical staff members are aware of these changes.
Appointment confirmations
Risk 1: Appointment confirmations ineffective (as measured by patient failures).
Strategy 1: Current procedures include both sending cards and/or personal contact. One strategy includes an additional personal contact in the case of critical appointments (the definition of "critical" needs to be established). This would take place in advance of - and in addition to - the normal personal contact and would provide a prior indication of patient attendance.
Risk 2: Office staff is unable to contact patient.
Strategy 2: The advancement of communications techniques may assist in minimizing this risk. In addition to traditional methods - telephone and mail - an increasing number of people have fax machines and e-mail addresses. Determine the patient's willingness to accept messages of this type and include relevant information in the patient database. These options provide additional flexibility in patient contact.
Keeping accurate records of patient contact information -especially if someone other than the patient takes the message - may assist with future contacts, especially if the message-taker proves to be unreliable.
Confirmation messages left on answering machines may not be acceptable for certain patients.
Office-initiated appointment-rescheduling
Risk 1: Disrupting the schedule, thus affecting staff and patients.
Strategy 1: Emergencies and sickness happen. This frequently translates into unplanned, office-initiated appointment-rescheduling. Careful planning should keep other office-initiated appointment rescheduling to a minimum.
Patient coming in without proper preparation
Risk 1: Clinical staff may not be able to see patient for appointment.
Strategy 1: Stress importance of preparation to the patient. Include reminder in confirmations.
Patients presenting without a confirmed appointment in the scheduler
Risk 1: Clinical staff may be unable to accommodate unscheduled patient.
Strategy 1: Staff must enter all patient appointments in the scheduler as soon as they are made and make any changes on a real-time basis. If a patient does come to the office without a confirmed appointment in the scheduler - and has evidence of an appointment - staff should make every effort to accommodate the patient. If you need to make another appointment because the patient cannot be seen, the inconvenience to the patient should be minimized.
The patient's next appointment
Risk 1: Appointment not scheduled.
Strategy 1: Staff should attempt to schedule the patient's next appointment at the conclusion of the current one. If this cannot be done, staff should initiate contact with the patient, rather than wait for the patient to do this.
Patient follow-ups
Risk 1: Not obtaining feedback on level of patient satisfaction.
Strategy 1: Regularly structured patient-satisfaction surveys, performed by someone independent of the patient's caregiver, provides invaluable information for the practice. Office and clinical staff also can provide valuable anecdotal evidence to this process. Staff should analyze information received and adjust the management system as necessary.
Make it your own!
A well-thought-out system may greatly assist the practice in managing patient appointments. Such a system needs a mechanism for continual improvement as new scenarios occur or are reported. The system should always reflect the "best practice" of the office. This can only happen if the staff members themselves develop, implement, and maintain the system, so they own it, use it, and improve it.
Shelley R. Blumstein, RDH, is a practicing hygienist who has worked in periodontal practices since 1973. She may be contacted by e-mail at [email protected].
Barry S. Blumstein, CQMC, CMC, is a consultant specializing in the facilitation of management-system development and implementation, operational controls, and process improvement. He assists organizations in transforming strategies into results by "best practice" discovery, then by process documentation. He may be contacted by e-mail at [email protected].
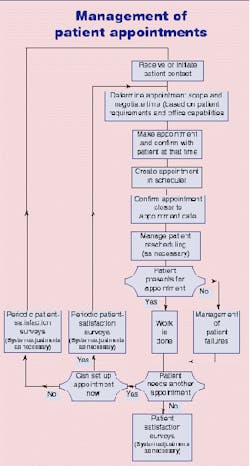
Phases of Management of Patient Appointments
Phases of management of patient appointments include the following activities:
- Patient contact
- Making the appointment
- Appointment confirmation
- Appointment rescheduling (as necessary)
- Patient presentation
- Follow-up
Each of these phases can be described as a process during which staff members perform many actions. Staff also may need to make decisions to ensure objectives are met. Actions and decision-making include areas of risk exposure. Strategies need to be formulated, agreed upon, implemented through process management, and "owned" to control and minimize risk. Ac com plishing this is a team effort.