Demystifying In-Office Whitening
by Sheri B. Doniger, DDS
A review of the whitening systems available enables practitioners to choose the best method for them.
One of the most effective and immediately satisfying procedures we perform is vital whitening. Our patients request it. They are inundated with input from television, magazines, and movies for the perfect white smile. They are involved in the process and appreciate the results. The office-monitored system provides:
- Speed of whitening
- Accuracy
- The ability to correct shade differences
- Patient education regarding the mechanisms of treatment, protocols, and postoperative expectations.
This article is an overview of systems available. No specific product is highlighted, and the author recommends no specific technique. Knowledge about the variety of systems available will help guide offices to a product that is suited to their needs.
Whitening is accomplished by the oxidation of stains by hydrogen peroxide, which is the active ingredient in all office-whitening procedures. This technique has been used to bleach teeth in the dental office for more than 125 years. Hydrogen peroxide breaks down to free radicals (H2O2) that penetrate the enamel. These free radicals attack the organic components of the enamel (which is approximately 96 percent inorganic, 4 percent organic), forming smaller components that reflect less light. These less reflective, smaller molecules are colorless, hence causing the tooth to appear lighter.
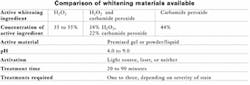
The basic process of oxidation with hydrogen peroxide has changed little during the past 25 years, but there have been advances in techniques. The active ingredient remains hydrogen peroxide. A few companies, though, utilize carbamide peroxide (which breaks down to hydrogen peroxide) or a combination of the two products. The H2O2 requires a pH that is slightly buffered to elicit the formation of more free radicals. The concentration of the H2O2 varies between products, ranging from 35 to 55 percent. The manufacturers present the materials in one of two forms - either a premixed gel or a powder/liquid
that is operator-controlled. The activation of the chemical reaction occurs via three avenues: light source, laser, or neither. Heat was previously utilized and still may be a technique in some offices. The light source speeds up the oxidation reaction, making the process quicker. The treatment time may range from 20 to 90 minutes per session.
The reapplication of the product depends on the manufacturer's recommendations and the activation process utilized. Completed treatment may be accomplished in one or several sessions, depending on the severity of the stain and type of stain presented. Yellow stains appear to be the easiest to whiten while tetracycline stains will be the most difficult.
Some in-office procedures recommend at-home follow-up and the fabrication of trays. These trays can be fabricated during the treatment visit, and clincians need need explain their use to the patient. The trays serve the dual purpose of performing the at-home bleaching procedure and, if the patient has sensitivity, delivering the desensitizing treatment. A 1.1 percent neutral NaF or desensitizing paste of potassium nitrate usually alleviate postoperative sensitivity. Some companies furnish these products with their kits.
The various adjunctive activation sources available are the curing lights currently used in the office for dental resins, as well as lasers.
These lights all have similar wavelengths for activation of the photoinitiators in resin materials. The two types of halogen lights are the standard or conventional halogen and the fast halogen.
The main difference between these lights is the Uva intensity or power output. Several fast halogen lights are capable of increasing their power intensity via higher output lamps coupled with smaller diameter light focusing tips. The more output on the light, the shorter curing time. So, a curing light with a bandwidth of 400 to 25 NM (the higher range of halogen lights) will cure longer in the higher output or "boost" mode. The power is increased from 600 to 850 mW/cm2 to over 1000 to 1600 mW/cm2, depending on the light utilized. The curing process and activation of the bleaching materials is thereby quickened.
A comparison of various dental lights and lasers reveals the following bandwidths:
- Halogen, 385 to 535 NM
- LED, 440 to 490 NM
- Plasma arc, 380 to 495 NM
- Laser, 400 to 980 NM
Newer technology is always evolving. CRA Newsletter described plasma arc lights as utilizing "an electrical arc between two electrodes in a xenon gas-filled lamp to generate intense white light." This plasma arc light is filtered as a halogen light to fall in the appropriate photoreactive curing range for composites and bonding materials. These lights are faster and create more heat than both halogen types, which could hasten whitening procedures. One delivery system combines the plasma arc light with a mouthpiece that covers the entire smile line.
LED (light-emitting diodes) appears to be one of the newest technologies. They consist "of semiconductors that emit low-intensity, narrow spectrum light via electrically excited atoms," according to CRA Newsletter. Operating in a wavelength of 430 to 510 NM, they do not generate heat due to the low intensity of power. They are battery operated, lightweight, and portable.
Lasers also are available as adjuncts to whitening. All electromagnetic radiation consists of photons or discrete packets of energy. Lasers operate in the infrared, visible, and ultraviolet radiation portion of the electromagnetic spectrum.
The optical bandwidths of the electromagnetic spectrum that are used in dentistry are:
- Ultraviolet, 100 NM to 400 NM
- Visible, 400 NM to 750 NM
- Near infrared, 750 NM to 3000 NM
- Far infrared, 3000 NM to 1 mm
All lasers have their own specific wavelength (monochromatic). They are directional (the light can be focused in a narrow beam as opposed to visible light, which has a scattered emission). They are in-phase (light energy in step with each other), and they are coherent (they can deposit a large amount of energy in a very small area). Lasers have a high-intensity output (ranging from 700 to 1800 mW/cm2).
Lasers currently in use in dentistry for whitening include CO2 gas lasers that have a primary output of visible red light. Xenon and argon lasers, which are eximer types of lasers, use reactive gases (Cl and Fl) mixed with inert gases. These inert gases, when stimulated, form a pseudomolocule or dimer (hence the name eximer or excited dimer). They produce light in the blue to blue-green range. The diode or semiconductor lasers are small electronic devices that use low power. They have a wavelength of 815 to 980 NM, which fall in the near infrared category. The speed of the lasers is the fastest of all the options listed.
Other lights are available under exclusive licenses that are utilized with specific products. Due to the proprietary nature of these activating devices, they will not be discussed in this article.
The team approach
The whitening process is a team effort. The dentist accomplishes the initial diagnosis and treatment planning, but the hygienist and the assistant truly are the initiators of the process. During the initial patient experience or a routine preventive care visit, the hygienist discusses the possibilities of whitening with the patient. There are always questions regarding time, comfort, cost, and post-treatment experiences, which means that the hygienist plays an important role in the whitening center of the practice.
Patient expectations should be discussed between multiple staff members. The hygienist leads the way, working closely with the dentist on the limitations of certain stains to be whitened and the single tooth discrepancies that may involve more time and attention.
When the question "how long will this take?" arises, the only true response, as we can all attest, is "as long as it takes." For the majority of cases, we will have met or exceeded our expectations with the initial diagnosis and pursuant treatment plan. Those few rare cases with the recalcitrant stains may take a little longer. Patients need to be informed about the non-finite time line of the procedures.
The application of whitening agents by hygienists and assistants - with or without activation lights - is dependent on state dental practice acts. Upon consultation with the American Dental Association's legislative liaison, each state has its own definition of dentistry, and the application of these procedures is on a state-by-state basis.
Knowledge about the product utilized and the expected outcomes are paramount to a successful result. Whichever product is utilized in your offices, all of those parameters should be known. Any marketing literature utilized by the office for the in-office whitening should be examined and reviewed by the entire team, as should the procedure itself.
Through the dental team, the patient understands the process and the value of whitening. The choice of product and activation method is solely in the hands of the individual dental office. The immediate results of successful whitening make the patient very happy. Happy patients are excellent referral sources. There is nothing mystical about being happy.
The author wishes to thank Paul A. O'Connor for his extensive research assistance. He is the legislative liaison of state government affairs for the American Dental Association. The author also thanks Dr. Kenneth A. Jurek for his invaluable knowledge and information concerning lasers.
Sheri B. Doniger, DDS, practices in Lincolnwood, Ill. She graduated from the University of Illinois College of Dentistry in 1983 and obtained her bachelor's degree in dental hygiene from Loyola University of Chicago in 1976. She can be reached at (847) 677-1101 or [email protected].
In-Office Whitening
An example of the process for in-office whitening
- Initial diagnosis and treatment plan by dentist
- Informed consent with financial arrangements
- Pre-procedure clinical photographs
- Prophylaxis to remove all organic debris
- Tissue protection (cured resins, various gels or rubber dam)
- Application of materials with reapplication as per manufacturer
- Remove all whitening product from tooth
- Re-clean teeth
- Remove tissue protection
- Educate and reinforce protocol
- Discuss any possible postoperative effects from modalities of treatment
- Follow up and photographs