A candid talk about pain
You told us about how the job hurts you. Here`s what we have to say.
Carol Coady
Editor`s Note: In a questionnaire published in the November 1999 issue, RDH asked readers 20 questions regarding occupational injuries or illness. In a related article in the same issue, RDH featured Carol Coady, RDH, BA, the founder of the Hygienists` Pain Network. She revealed many of her own experiences in rehabilitating from an occupational illness that nearly disabled her. RDH asked Ms. Coady to comment on the responses to the questionnaire below.
The survey was completed by 468 readers. According to a general question that led off the survey:
- 11 percent of the responding readers have practiced for less than five years.
- 17 percent have been in practice for five to 10 years.
- 27 percent have practiced for 11 to 20 years.
- 45 percent have practiced for more than 21 years.
Obviously, RDH recognizes that the results of the survey are heavily influenced by veteran hygienists who have been working for a long time. Many occupational injuries and illnesses develop as a result of prolonged exposure in a work environment.
However, Ms. Coady observes, "Pain, for some individuals, starts even before finishing hygiene school and entering clinical practice. I have received reports from some dental hygiene students who experience work-related pain. Pre-existing and co-existing factors are often culprits.
"On the other hand, there are hygienists who have practiced for many years who don`t have pain problems. We could all learn from them by studying their health factors, lifestyles/ activities of daily living, work-ing environments, and their neuromuscular and postural habits. Physical exercise, nutrition, tobacco use, genetic factors, and mental outlook are some of the issues that play into the risk-factor equation.
"In other words, the number of years in practice does not necessarily equate with symptom development."
Coady can be contacted at Hygienists` Pain Network, P.O. Box 24, Paradise, CA 95967 (include a SASE) or by e-mail at [email protected].
Do you feel you are well-informed about how to prevent work-related musculoskeletal pain?
RDH`s answer: 68 percent of the readers indicated that they do not feel well-informed.
Coady`s comment: According to an extensive national study, one-fifth of the dental hygienists who leave dental hygiene practice permanently are affected by disability. Those of us who are in leadership positions must increase our efforts to provide practitioners access to occupational health information. As oral health preventive specialists, we value the concept of prevention and must expand our efforts to prevent occupational illness as well.
Source:
- Miller DL: An Investigation Into Attrition of Dental Hygienists From the Work Force, Journal of Dental Hygiene, Jan. 1991; 65. pp.25-31.
In general, do you experience what you perceive to be an unhealthy level of stress and tension while at work?
RDH`s answer: 61 percent believe that an unhealthy level of stress and tension is present in the work setting.
Coady`s comment: Muscles become less resilient and more dysfunctional when stressors exceed the muscle`s ability to rebound. Unfortunately, due to patient needs and limitations, we find that there are times when we must work in awkward positions. There are also times when we find ourselves overtaxing the small, delicate musculoskeletal structures in our hands as we perform our clinical duties. The physical demands of clinical practice are great. The emotional demands we face affect muscle tension as well. It behooves every member of the dental team to take responsibility for minimizing emotional and physical stress in the workplace. Interpersonal relationships, work procedures (including instrument selection and technique), workload management, work station design, and environmental factors (such as room temperature) play important roles when it comes to promoting a healthy working environment for all office members.
At the end of the work day, how do you usually feel?
RDH`s answer: Readers had several options they could check off. Only 4 percent, though, said they were "comfortable" at the end of the work day - the only positive response available.
The other responses were:
- Uncomfortable (17 percent)
- More than uncomfortable; I am in pain (18 percent)
- Muscles feel tight, but I can relax them before I go to sleep at night (17 percent)
- Muscles feel tight, and I am not able to relax them before going to bed at night (23 percent)
- Overly fatigued (21 percent)
Coady`s comment: This question hints at how working affects how hygienists feel when they are not at work. In other words, there is a price to pay for generating work-related pain. Work-related pain can affect the quality of well-being experienced outside the office (as well as inside the office) and can influence our thinking, emotions, attitudes, behaviors, and actions - what a price to pay!
Our relationships with others are affected, and our choices about the activities we choose to participate in are affected too. Work-related pain changes lives. Yet those changes can be so subtle that we may not realize the far-reaching consequences.
Muscles that can`t be relaxed easily and bodies that are overly fatigued are at greater risk for a multitude of health problems.
Which of these sensations do you experience on an occasional or regular basis as a consequence of clinical dental hygiene work?
RDH`s answer: The "sensations" listed as possible answers were tingling, numbness, pain, and diminished dexterity. Readers were encouraged to "check all that apply." Since 1,085 responses were given to the question, most readers checked off at least two symptoms. Only 22 respondents did not answer the question.
"Pain" was the most common answer (37 percent). "Tingling" (23 percent), "numbness" (20 percent), and "diminished dexterity" (20 percent) were also reported.
Coady`s comment: These are commonly expressed symptoms relayed by Hygienists` Pain Network participants. They can be caused by compression, entrapment, or distention of nerves as they pass through anatomically restricted areas and/or tight muscles. Nerves that suffer impairment at proximal sites increase the potential for distally located symptoms and pathology - hence the potential for double- or multiple-crush injuries.
Sources:
- Nemoto K, et al.: An experimental study on the `double crush` hypothesis. Journal of Hand Surgery. July 1987 (12A:4)552-559
- Kasdan ML, ed.: Occupational hand and upper extremity injuries and diseases. Philadelphia, PA: Mosby-Year Book, Inc. 1991.
Do you feel as though work- related musculoskeletal pain is negatively affecting the quantity and/or quality of your usual sleep cycle?
RDH`s answer: 64 percent of the readers said work-related pain affects sleeping habits.
Coady`s comment: Hygienists who are experiencing a decline in their sleep patterns should discuss the problem with their physicians. A normal sleep cycle is vital to good health.
Prolonged sleep deprivation may affect a number of biological processes, including cognitive function, mood, pain level, thyroid function, plasma cortisol and iron, and immune system alterations. Lack of quality sleep can exacerbate pain problems which, in return, can make it difficult to obtain quality sleep. This creates a vicious cycle of pain generation and sustenance. Chronic pain can lead to the development of chronic pain syndromes such as myofascial pain syndrome and fibromyalgia.
Growth hormone is vital for tissue growth and cellular repair. We all experience microtrauma on a daily basis, and growth hormone is necessary for normal muscle cell turnover and homeostasis. When muscles are chronically tight, circulation is impaired, resulting in an even greater need for the beneficial effects of growth hormone.
However, almost all growth hormone is produced as a result of the deep, restful phase of sleep consisting of stages three and four slow-wave-sleep. Individuals with disturbed sleep patterns may not produce adequate growth hormone. Abnormal brain waves during deep sleep diminish the production of the growth hormone necessary for normal tissue metabolism. This metabolic pitfall may place individuals at even greater risk for tissue decline and musculoskeletal problems.
Source:
- Fibromyalgia Network Newsletter, January 1997, pp. 3-6.
- HealthNews Newsletter from the publishers of "The New England Journal of Medicine," February 2000, pp. 1-2.
Do you use any ergonomically oriented products/ equipment in the practice of dental hygiene to benefit your own comfort or health?
RDH`s answer: The short list provided in the questionnaire included the following options:
- Ergonomically designed operator`s chair (19 percent)
- Magnification system/telescopes (6 percent)
- Right and left fitted gloves
(13 percent)
- Ergonomically designed instruments (46 percent)
- Extraoral vision system
(4 percent)
Readers were invited to write in other ergonomic steps taken in the hygiene operatory. The submitted comments referred to back braces and belts, visual reminders about posture, special headrests for positioning a patient`s head more favorably, exclusive use of ultrasonic equipment, and modifications to equipment such as reducing the reach for the suction arm.
One reader added, "I stand while I work; I alternate between work shoes."
Coady`s comment: Ergonomically oriented products and equipment can be of tremendous benefit to clinicians. One comment that I would like to make is in regard to telescopes. It is important to make sure that the angulation of the telescopes is steep enough to allow the operator to sit upright without needing to drop the head down. Inadequate angulation of the telescope results in the operator needing to bend at the neck in order to see into the mouth. Chronic forward bending of the neck is a risk factor for pain and the development of musculoskeletal disorders.
Exercise makes me feel better, worse, or about the same?
RDH`s answer: According to the readers, exercise makes 48 percent "feel better." A fourth option - an inconclusive "sometimes better, sometimes worse" - was chosen by 36 percent. Twelve percent answered with "about the same."
Only 4 percent said exercise definitely makes them feel worse.
Coady`s comment: Exercise can help or exacerbate work-related pain - due to the many variables involved. One point to make is that chronically stressed muscles can become hyperirritable. Hygienists with chronic muscle tension may find that exercise - which relieves muscle tension and discomfort when muscle tone is normal - may find that certain movements may exacerbate pain problems.
When muscles are hyperirritable, activities such as the normal swinging motion of the arms while walking may intensify upper body pain and tension. In such a situation, what can happen is that tight muscles may impair circulation and lead to the development of active trigger points. These trigger points are loci of muscle dysfunction and hyperirritability, which results in the magnification of pain and the sustenance of muscle irritability, hence perpetuating a vicious cycle.
This sustained muscle irritability then increases the likelihood that activities such as intraoral services (with the inherent static postural demands) generate pain. Also, nerves that run through tensed muscles can become compressed and generate feelings of numbness and/or paresthesia (the feeling of "pins and needles," or a prickly sensation). These unpleasant sensations of pain, numbness, and/or paresthesia can cause emotional distress, which generates even more stress and tension, becoming a part of this multifactorial continuous vicious cycle.
What exercise approach do you use to prevent or help alleviate work-related musculoskeletal pain?
RDH`s answer: Five different answers provided examples of common ways to exercise: aerobics, yoga, stretching, resistance or weight training, or back strengthening. Of the 200 readers who took advantage of the opportunity to personalize responses to this question, more than half referred to routines that included walking or running - with an emphasis on the former.
Others answered with massages, traditional exercise equipment, swimming, or Tai Chi. Some unique solitary answers included tap dancing, ballet, roller hockey, or housework or yardwork.
In regard to the answers provided on the survey, the following levels of participation in these exercise routines were noted:
- Stretching (31 percent)
- Resistance or weight training (16 percent)
- Aerobics (14 percent)
- Back strengthening (14 percent)
- Yoga (5 percent)
Coady`s comment: A variety of exercise approaches are likely to be helpful to hygienists. The important point to be made here is that the exercise program should counteract the static postural demands of dental hygiene practice. Ideally, the muscles that are chronically contracted during clinical work should have the opportunity to stretch and relax during the exercise. Not only is it important to exercise, but it is important to employ the body well in the process. Poor form can exacerbate pain and musculoskeletal problems.
In addition, it is important that the activity be something the individual finds to be enjoyable and that results in an enhanced sense of well-being by the time the activity is completed.
Where do you experience chronic, recurring work-related pain?
RDH`s answer: The survey listed 15 regions of the body, and readers were encouraged to "check all that apply." The percentage of readers who experienced chronic pain in each of these body areas are as follows:
- Neck, 82 percent
- Upper back, 62 percent
- Right shoulder, 56 percent
- Lower back, 48 percent
- Right wrist, 43 percent
- Left shoulder, 39 percent
- Right forearm, 32 percent
- Right elbow, 25 percent
- Left wrist, 16 percent
- Left elbow, 13 percent
- Right leg, 14 percent
- Left leg, 13 percent
- Left forearm, 10 percent
- Right foot, 8 percent
- Left foot, 6 percent
A final option to answering this question was, "Generalized pain, or pain that moves around frequently;" 13 percent checked off this answer.
Coady`s comment: I would like to call attention to two similar surveys that have been done, including one in the Journal of Dental Hygiene. Dr. Tommy Oberg and Ulrika Oberg studied the "frequency of complaints from different parts of the body" in a 1993 study. The other one was an informal gathering of data from participants of the Hygienists` Pain Network.
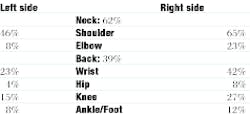
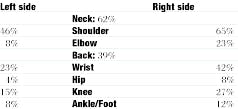
Regarding Obergs` survey, their results showed frequency of complaints as follows:
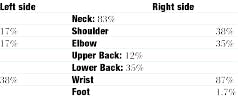
According to a 1996 survey of 60 participants in the Hygienists` Pain Network, the body parts experiencing pain were as follows:
"Eighty-two percent of the RDH readers who responded to the November 1999 survey reported having neck pain. Both of the other surveys also revealed high percentages of neck complaints (62% and 83%, respectively). This is critically important to note since much of the musculoskeletal pain problems that hygienists are experiencing are likely to be related to frequently dropping the head forward and down, as well as tilting and leaning the head laterally for prolonged periods of time. These detrimental postural patterns are common in clinical practice and can result in far-reaching consequences. The cervical spine contains delicate neuromuscular structures which are easily damaged and often implicated in work-related musculoskeletal disorders.
In addition, innervation of the upper extremities occurs at the cervical 5-8 down to the thoracic 1 levels of the spinal column. It is in the cervical 4-5-6 region that the most severe neck-bending occurs during forward neck flexion. Many of the hygienists who have shared their pain experiences by way of the Hygienists` Pain Network have expressed that imaging studies taken of their necks reveal damage to the cervical structures, particularly at the cervical 4-5-6 level. Damage at this level not only affects the health of the cervical spine, but also can contribute to the risk of developing double- or multiple-crush injuries distal to the cervical spine and along the same nerve pathways that serve the upper extremities.
Notice that all three surveys reported that pain is greatest on the right side. This consistent finding is likely to be related to most hygienists being right-handed and leaning to the right. There is more compression and loading (especially during intensive hand instrumentation) on the right side for right-handers. Right-handers often lean to the right - particularly if they are not maximizing their opportunities for indirect vision.
Many of us sustain the bad habit of straining to see directly into the mouth when we should be sitting upright and utilizing our mouth mirrors to indirectly view the hard-to-see areas. Prolonged forward leaning, lateral tilting, and twisting of the back, neck, and shoulders places tremendous stress on these structures and places hygienists at risk for a variety of musculoskeletal disorders. In addition, we are taxing the delicate structures of our hands when we vigorously hand scale, rather than maximizing the use of ultrasonics. I am a proponent of hand instruments, but I try to remove as much of the tenacious calculus as I can with ultrasonic instrumentation.
The damaging effects of these stressful postural and neuromuscular habits are extremely important for hygienists to recognize and modify. It is imperative that we sit tall and flex from the top of our spines, where there are no intervertebral discs to damage. Rather than bending at the neck, we must be in the habit of flexing at the occiput-atlas-axis articulations and peering into the mouth by casting our eyes downward. Making these kinds of postural modifications may feel awkward at first and may require instruction from individuals who are well-versed in postural health. However, the benefits are well worth the effort.
Improving our postures improves the way we feel. Good postural form generates reduced muscular tension and greater ease. Working with lengthened spines and greater neuromuscular balance results in less strain, better endurance, and greater overall comfort. We find that with good posture and wise instrument selection, we not only feel better but we reduce our risks for developing and perpetuating musculoskeletal disorders.
Source:
- Öberg, Tommy MD, PhD. and Öberg, Ulrika RPT: Musculoskeletal Complaints in Dental Hygiene: A Survey Study From a Swedish County. "Journal of Dental Hygiene," July-August 1993. 67:5:257-261. Page 259: Figure 1 "Frequency of complaints from different parts of the body during the last 12 months in 28 dental hygienists.
Do you have chronic/ recurring work-related pain that has spread beyond the point of where the pain originated?
RDH`s answer: 55 percent indicated that the work-related pain they feel has spread to other areas.
Coady`s comment: This question was asked for two reasons. First of all, musculoskeletal stress at one site of the body can make others sites more vulnerable for symptoms - due to peripheral factors. The double- or multiple-crush injury is an example of peripherally based factors and was discussed previously.
In addition, bombardment of pain signals from the periphery can create functional changes within the central nervous system. These changes amplify the sensation of pain, allow for previously nonpainful stimuli to become painful, and can spread pain beyond its original site of occurrence.
Source
- "Understanding Chronic Pain," Robert Bennett, MD, Professor of Medicine at Oregon Health Sciences University.
For what length of time have you experienced chronic work-related pain?
RDH`s answer: As indicated at the beginning of this article, 72 percent of the readers participating in the survey have practiced more than 11 years. With that in mind, 44 percent of the respondents said they have experienced chronic pain for more than five years.
Otherwise, the answers were broken down into the following time frames:
- 32 percent reported symptoms of work-related pain for the last one to three years.
- 13 percent said within the last four to five years.
- Six percent indicated within the last three to six months.
- Five percent said within the last seven to 12 months.
Coady`s comment: As I mentioned earlier, we need to be aware that some individuals experience work-related pain even while in dental hygiene school. However, as the results show, hygienists who have been in practice for five or more years have had more time for the cumulative effects to occur.
Have you ever consulted with a physician regarding work-related musculoskeletal pain?
RDH`s answer: 79 percent have consulted with a physician.
Coady`s comment: Hygienists often question what kind of doctor is most likely to understand work-related musculoskeletal disorders. There isn`t a hard and fast answer. However, early and appropriate intervention provides the best approach to a successful outcome. I would suggest that hygienists who are in need of medical attention ask around regarding well-informed doctors. Hygienists` Pain Network participants share this kind of information with one another and have even accompanied one another to various medical appointments. Sharing support and information can help immeasurably.
Many hygienists are surprised to learn that the specialty of rheumatology is often a good place to start looking. There is substantial research on musculoskeletal disorders published in the rheumatology literature. Hygienists may wish to contact the Arthritis Foundation for assistance. However, the specialty of rheumatology is just one option.
For hygienists who are experiencing complex chronic pain problems, it may be best to seek out a well-established, multidisciplinary pain treatment program, particularly one which is affiliated with a major university or hospital. Work-related musculoskeletal problems can be very complex and may require a multifaceted approach to treatment.
A concern that I have is regarding those hygienists who have not sought out medical advisement and care for potentially serious work-related pain. There are likely to be a variety of reasons for not seeking out professional attention. However, if a hygienist is experiencing recurring or persistent pain, it is not a good idea to ignore the warning signs. Work-related pain is likely indicating that something isn`t right. Pain can be a very useful tool since it can alert us to a problem that needs to be addressed.
Has a physician ever diagnosed you with a work-related musculoskeletal or secondary disorder?
RDH`s answer: A list of 21 disorders was provided in the survey, and readers were asked to indicate whether they had been diagnosed or if they suspect they have suffered from an undiagnosed disorder. The percentages of readers diagnosed, or who suspect an undiagnosed disorder, are as follows:
- Tendinitis: diagnosed (32 percent); suspect undiagnosed (11 percent)
- Carpal tunnel syndrome: diagnosed (20 percent); suspect undiagnosed (16 percent)
- Myofascial pain syndrome: diagnosed (9 percent); suspect undiagnosed (10 percent)
- Temporomandibular dysfunction: diagnosed (19 percent); suspect undiagnosed (7 percent)
- Chronic headaches: diagnosed (14 percent); suspect undiagnosed (15 percent)
- Chronic shoulder bursitis: diagnosed (10 percent); suspect undiagnosed (14 percent)
- Ulnar nerve neuropathy: diagnosed (10 percent); suspect undiagnosed (6 percent)
- De Quervain`s disease: diagnosed (3 percent); suspect undiagnosed (1 percent)
- Osteoarthritis of the thumb(s)/finger(s): diagnosed (10 percent); suspect undiagnosed (13 percent)
- Stenosing tenosynovitis: diagnosed (1 percent); suspect undiagnosed (1 percent); no response (57 percent)
- NSAID-induced colitis: diagnosed (2 percent); suspect undiagnosed (4 percent)
- Degenerative disc disease: diagnosed (14 percent); suspect undiagnosed (5 percent)
- Osteoarthritis of the spine: diagnosed (10 percent); suspect undiagnosed (4 percent)
- Cervical radiculopathy: diagnosed (4 percent); suspect undiagnosed (1 percent)
- Sciatica: diagnosed (12 percent); suspect undiagnosed (7 percent)
- Shoulder impingement: diagnosed (11 percent); suspect undiagnosed (16 percent)
- Thoracic outlet syndrome: diagnosed (6 percent); suspect undiagnosed (6 percent)
- Fibromyalgia: diagnosed (9 percent); suspect undiagnosed (9 percent)
- Reflex sympathetic dystrophy: diagnosed (1 percent); suspect undiagnosed (1 percent)
- Chronic back pain: diagnosed (25 percent); suspect undiagnosed (16 percent)
- Foraminal stenosis: diagnosed (1 percent); suspect undiagnosed (1 percent)
Coady`s comment: The fact that so many of the hygienists suspect that they have specific disorders - yet remain undiagnosed - concerns me. If they really have these disorders, it is important that they receive the care they need so they can avoid serious consequences.
How would you rate your treating physician`s knowledge and understanding of your work-related pain?
RDH`s answer: 44 percent described the care from their physician as being "moderately helpful;" 27 percent said "not very helpful;" 17 percent said "excellent;" and 11 percent said "poor."
Coady`s comment: It is very important that hygienists have access to quality care to maximize the potential for successful outcomes. Many of the physicians who provide services through the workers` compensation system are earnest in their efforts to help those in pain. However, a number of Hygienists` Pain Network participants have expressed frustration, anger, and mistrust of the system that is supposed to help injured workers.
Hygienists who have opened workers` compensation claims should keep running journals of pertinent issues pertaining to their cases. In the event that they become dissatisfied with how their claims are being handled, they can approach the appropriate parties regarding the details they feel are being mismanaged and express what they think needs to take place.
Which activities exacerbate your symptoms of pain, tingling, or numbness?
RDH`s answer: Seven common activities were listed in the survey. Carrying children, packages, or other weighty objects present additional strain to 57 percent of the respondents. Symptoms also were reported with the following activities:
- Housework (56 percent)
- Writing (54 percent)
- Driving (51 percent)
- Hobbies (35 percent)
- Keyboarding (34 percent)
- Sports (25 percent)
Readers were invited to submit other activities where pain symptoms surfaced. These activities included yardwork, stairs, personal hygiene, cooking, home repairs, and sitting, standing, or grasping in one position for too long.
Coady`s comment: Work-related musculoskeletal problems can severely curtail participation in a broad range of activities. It is vital that we recognize the seriousness of these disorders and how intrusive they can become.
Do you have any previously occurring or concurring medical conditions that exacerbate your work-related pain?
RDH`s answer: 74 percent indicated that the work-related pain was unrelated to any other medical condition or injury.
Coady`s comment: Physicians, workers` compensation claims agents, employers, co-workers, family, and friends sometimes express skepticism regarding linking clinical hygiene work with musculoskeletal disorders.
However, as can be seen by this answer, most of the hygienists surveyed claim that clinical work is directly linked to the development of their symptoms. We can better understand and express this link if we take the time to become well-informed regarding these disorders.
At the same time, it is important to note that, in some cases, pre-existing and concurring medical conditions may be risk factors for the development of musculoskeletal symptoms. Whiplash injuries and scoliosis are conditions that were frequently mentioned by survey respondents. Potential student applicants should be informed of these kinds of risk factors so that they can make informed decisions as to whether or not to pursue careers in clinical hygiene.
Has chronic work-related musculoskeletal or secondary pain ever caused you to alter your work schedule in any way?
RDH`s answer: The impact of pain on a dental hygiene career appeared in the following ways:
- 43 percent said they reduced the number of days that they work(ed).
- 36 percent said that work-related pain is causing them to consider leaving clinical hygiene practice prematurely.
- 21 percent said they reduced the number of hours per day that they work(ed).
- 15 percent said they stopped practicing clinical hygiene for a period of time.
- 14 percent said they reduced or eliminated the number of root planing patients that they treat(ed).
- 8 percent said they are no longer able to practice clinical hygiene due to work-related pain or disability.
Coady`s comment: I concur with the findings reported by respondents. In addition, I would like to emphasize the importance of education. Understanding proper body mechanics, ergonomics, and the many additional factors that affect physical and mental well-being are important features to incorporate into our lives. These problems are much easier to prevent than to resolve.
Have you ever received medical or alternative treatment for work-related musculoskeletal pain?
RDH`s answer: 63 percent of the respondents said they have taken oral medication for work-related pain, and 58 percent have tried massage therapy.
Other treatments include:
- Chiropractic adjustments (54 percent)
- Physical therapy (50 percent)
- Splints or braces (42 percent)
- Trigger-point injections, steroid injections, or nerve blocks (26 percent)
- Acupuncture (10 percent)
RDH then asked which approaches have best helped to relieve work-related pain. According to the respondents, the most successful approaches were exercise (59 percent), reducing the workload (44 percent), massage therapy (43 percent), chiropractic adjustments (33 percent), relaxation techniques (24 percent), and physical therapy (24 percent).
Coady`s comment: It is my opinion that education - coupled with a well-designed working environment and health-promoting working conditions - is our best approach to preventing these disorders. It is much easier to prevent these problems from occurring than to try to resolve them once they`ve become chronic.
If you filed a workers` compensation claim, how would you describe your experience with your employer related to filing the claim?
RDH`s answer: The options were "very stressful" (35 percent), "moderately stressful" (37 percent), and "not very stressful" (28 percent). However, 254 readers did not respond to the question, indicating that many have not filed a claim for work-related pain.
Coady`s comment: Unfortu-nately, the system that our society has in place to help resolve these problems all-too-often exacerbates them. The workers` compensation system, as it currently is set up, can be a nightmare for legitimately injured workers. Good people, representing the various sides of the situation, can end up feeling a great deal of frustration and animosity toward the others who are involved.
The Hygienists` Pain Network has helped to bring hundreds of dedicated Hygienists` Pain Network participants together. Thanks to the Internet, the communication between Hygienists` Pain Network participants is more dynamic and productive than ever. The network welcomes new participants and urges interested readers to e-mail Coady at: carol coady@aolcom.
Readers who do not have direct computer access can participate by asking an intermediate party (such as a friend or relative) to relay communication. Readers who must rely on the postal service may send a SASE to: Carol Coady, RDH, BA, Hygienists` Pain Network, P.O. Box 24, Paradise, CA 95967.