Is Flossing Dental Hygiene’s Sacred Cow?
Definition of a Sacred Cow: An outmoded belief, assumption, practice, policy, system, or strategy, generally invisible, that inhibits change and prevents responsiveness to new opportunities.
Definition appears in the book, “Sacred cows make the best burgers.” (Warner Books, 1996)
Ask yourself these questions. On the average day, how many patients do I talk to about using dental floss? How many patients follow this advice?
If you are like most dental hygienists, flossing is the primary tool that you recommend for interproximal cleaning. And, if your patients are similar to the general population, only about 30 percent use the product regularly, and even less do it correctly.1
The gap between what we advise and how well that advice is taken is hugely frustrating for many dental professionals. In response to this, we often try even harder to get patients to floss. We badger, take a strong stance, and lay down the law. And nothing changes. We ask ourselves if they are lazy, uninterested, or unmotivated. And we don’t know what to do.
The fact is that our patients simply do not “love” or embrace floss the way we do. They ask for something easier, and we respond by showing them how to use the floss, again. Now, more than ever, there is a wide variety of effective alternatives to floss for interdental cleaning (see Table 1). So why are we reluctant to recommend something different?
Flossing, it seems, has been woven into the fabric that makes up dental hygiene. It has become part of our culture or a “sacred cow” of sorts. Can we let it go? Can we embrace other methods to meet the needs of the 70 percent who cannot or will not use dental floss?
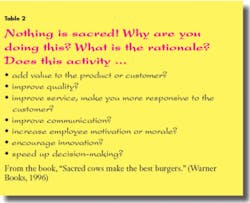
In the book, Sacred Cows Make the Best Burgers, Brandt and Kriegel advocate doing a reality check on some of our more basic assumptions about how we do business every day. One of the things that they advise paying particular attention to is the activities that are taken for granted. Brandt and Kriegel believe that nothing is sacred and that every activity should be viewed from a number of parameters that provide a true sense of the activity’s worth2 (see Table 2).
How well have we evaluated the activity of recommending flossing as a matter of course for most patients? Can it hold up to the scrutiny advocated by Brandt and Kriegel?
·Does this activity (floss) add value to the product (oral health) or the customer (patient)?
Flossing is often recommended as the primary intervention for both gingivitis and caries. The ability of flossing to reduce bleeding and gingivitis is well accepted. Graves et al. found that when floss was added to manual toothbrushing, the reduction in bleeding was nearly double that of brushing alone (67 percent versus 35 percent).3 Similarly, Lang et al. found that those who flossed at least four times per week had less plaque, gingivitis, calculus, and shallower pocket depths.1 However, in a study of health-care professionals that included 14.8 percent male dentists, persons flossing less than once a day were as likely to have periodontitis as those who flossed daily.4
It is generally believed that because floss passes through the contact area, it has a significant impact on the reduction of interproximal caries. The evidence for this is equivocal.5,6 Fluoride remains the most effective measure for the prevention and control of caries.7 Hotz states that in a pre-fluoride era, perfect plaque control was perhaps the only measure to decrease caries, but today, due to the benefit of fluoride from multiple sources, small to moderate amounts of plaque may not produce caries as easily as in the past.6
·Does it improve quality?
Most studies on floss have evaluated surrogate measures such as plaque or gingivitis but have not examined quality of life issues such as tooth retention. A recent study by Kressin et al. of 736 community dwelling men who were participating in the Veteran Affairs Longitudinal Study found that men who brushed and flossed regularly had a 56 percent reduction in the risk of tooth loss compared to those who did not practice regular hygiene habits. In comparison, consistent brushing alone resulted in a 49 percent risk reduction while the addition of a regular prophylaxis to brushing and flossing improved the risk reduction to 67 percent.8
·Does it improve service?
A healthy mouth usually means easier dental hygiene visits and easier visits often mean less chair time for the patient. Less chair time can reduce stress for all stakeholders. For example, a healthy mouth can have a prophylaxis rather than scaling and root planing. Importantly, the focus shifts to prevention and wellness, which has the potential to provide a more optimal level of service for the patient.
·Does it make you more responsive to your customers (patients)?
Even though floss improves oral health, current evidence indicates that only a small number (probably less than 30 percent) actually derive any benefit from the task.1 While batting .300 is great in baseball, in health care, that percentage seems blatantly unacceptable. As the association between oral and systemic health evolves, particularly with the new emphasis on inflammation reduction, it becomes even more important to partner with patients in response to their request for acceptable, effective, alternative tools.
·Does it improve productivity or cut costs directly?
It is easy to say yes to this question because treating a healthy mouth is much more time efficient. But that paradigm only applies to one-third of the people in your practice.1 Working on patients who bleed or have sensitive tissue from inflammation takes more time. More time means running behind, working through lunch and past quitting time. Working with a minimal or no break does not enhance job performance and increases stress and potential for errors.
·Does it improve communication?
The patient has no interest in flossing, yet we keep insisting that they do it. Having the same conversation over and over again is frustrating to all parties. Worse, it gives patients the impression that we are not listening to them. Medicine offers patients choices, even or especially when the disease is serious or life threatening. Discussing different options with people helps them “own” the choices that they make. Importantly, it has been observed that when patients are involved with their health-care provider in decision-making, satisfaction and compliance improves.9
·Does it increase motivation or morale?
Let’s see, we have already observed that people are not following our advice to floss and that the lack of flossing has the potential to increase appointment time, therefore adding to the likelihood of running behind and working into lunch and past quitting time. Going home exhausted and frustrated isn’t the stuff that makes you want to jump out of bed and get to work the next day. This hasthe potential to increase stress both at work and at home. Importantly, burnout is not uncommon in health care and oral care is no exception. All practitioners can take a role in helping to create a healthy work environment. As the dental hygiene leader in your practice, you have the power to “breathe life” into any new idea or device, such as alternatives to manual flossing.2
·Does it encourage innovation?
Focusing on floss as the best or only means for interdental cleaning blinds us to the many other effective methods that exist for removing interproximal biofilm and obtaining optimal oral health. It is surprising to many dental professionals to learn that numerous alternative products such as using floss with a floss holder, interproximal brushes, toothpicks, power flossers, and a dental water jet have been shown to be as effective as dental floss in reducing many traditional clinical parameters5,10-16 (see Table 1). There is often the assumption that a device must do exactly what floss does, such as go through the contact or wrap around the tooth to be effective, but the research does not bear this out.5,10-16 Importantly, in many studies, subjects preferred alternatives to traditional floss.11,13,14,15 In one study, subjects were surveyed six months post-study period to find out if they had developed a flossing habit and if so, with what product. Fifty percent of previous nonflossers were now flossing and 85 percent of those were using a floss holder as opposed to manual floss.14 In a recent study, the addition of a dental water jet to either manual or power toothbrushing provided superior results in reducing bleeding and gingivitis compared to a manual toothbrush and floss. This makes the dental water jet an effective alternative to traditional floss.16 Society seeks to make things easier for its members. Dentistry truly has been at the forefront of this with many products such as digital radiography or power toothbrushes. Yet we cling to a product that has changed minimally in 50 years.
·Does it speed up decision-making?
It has sometimes been said that the definition of insanity is doing the same thing over and over again and expecting a different result. Continuing to recommend floss when a patient is clearly not interested, and then failing to help the patient find an effective alternative product does not speed up or enhance improvements in oral health. If the patient is not responding to your recommendation to floss, try something else. Importantly, bring your patients into this process. Give them some choices of products or talk to them about products they’ve seen or heard about and in which they are interested. Find some mutual ground and give something different a try.
Yes, flossing has significant oral health benefits. But are those outcomes really related to the product or the process of interdental cleaning? Given the research showing that numerous other products provide a benefit similar to floss, and even more importantly, that those products have a better acceptance rate with patients than dental floss, I’d say it’s time to reevaluate that sacred cow.
Anyone for a hamburger?
Carol A. Jahn, RDH, MS, is the educational programs manager for Waterpik Technologies. She provides continuing education courses on periodontics and diabetes. She can be reached at [email protected] or (800) 525-2020, Ext. 8565.
References
1. Lang WP, Ronis DL, Farghaly MM. Preventive behaviors as correlates of periodontal health status. J Public Health Dent 1995; 55(1): 10-17.
2. Kriegel R, Brandt D. Sacred Cows Make the Best Burgers. 1996. New York: Warner Books.
3. Graves RC, Disney JA, Stamm JW. Comparative effectiveness of flossing and brushing in reducing interproximal bleeding. J Periodontol 1989; 60(5):243-247.
4. Merchant A, Pitiphat W, Douglass CW, Crohin C, et al. Oral hygiene practices and periodontitis in health care professionals. J Periodontol 2002, 73:521-535.
5. Brothwell DJ, Jutai DK, Hawkins RJ. An update of mechanical oral hygiene practices: Evidence-based recommendations for disease prevention. J Can Dent Assoc 1998; 64:295-306.
6. Holz PR. Dental plaque control and caries. In Lang, NP, Attström R., Löe H. Proceedings of the European Workshop on Mechanical Plaque Control, Berlin, Quintessence, 1998, pp.35-49.
7. Stookey GK. Caries prevention. J Dent Educ 1998; 62:803-811.
8. Kressin NR, Boehmer U, Nunn ME, Spiro III A. Increased preventive practices lead to greater tooth retention. J Dent Res 2003; 82:223-227.
9. Larrabee JH. The changing role of the consumer in health care quality. J Nurs Care Qual 1995; 9:8-15.
10. Kinane, DF. The Role of Interdental Cleaning in Effective Plaque Control: Need for Interdental Cleaning in Primary and Secondary Dentition. In Lang, NP, Attström R, Löe H. Proceedings of the European Workshop on Mechanical Plaque Control, Berlin, Quintessence, 1998, pp.156-168.
11. Shibly O, Ciancio SG, Shostad S, Mather M. Clinical evaluation of an automatic flossing device vs. manual flossing. J Clin Dent 2001; 12:63-66.
12. Anderson NA, Barnes CM, Russell CM, Winchester KR. A clinical comparison of the efficacy of an electromechanical flossing device or manual flossing affecting interproximal gingival bleeding and plaque accumulation. J Clin Dent 1995;6:105-107.
13. Spolsky VW, Perry DA, Meng Z, Kissel P. Evaluating the efficacy of a new flossing aid. J Clin Periodontol 1993; 20:490-497.
14. Kleber CJ, Putt MS. Formation of flossing habit using a floss-holding device. J Dent Hyg 1990; 64:140-143.
15. Christou V, Timmerman MF, Van der Velden U, Van der Weijden FA. Comparison of different approaches of interdental oral hygiene: Interdental brushes versus dental floss. J Periodontol 1998; 69:759-764.
16. Barnes CM, Russell CM, Reinhardt RA, Payne JB, Lyle DM. Comparison of irrigation to floss as an adjunct to toothbrushing: Effect on supragingival biofilm, gingivitis, and bleeding. J Clin Dent, in press, 2005.