A click away
Health information technology expedites communication between providers
by Cindy Quinn, RDH, BS
What a day Cathy has had! Her first patient was a recently diagnosed diabetic with deep pocket depths. An older woman who has taken medication for osteoporosis for four years was her next patient. On today’s radiographs, the woman’s mandible looked unusual. The next patient indicated a dose of six aspirin daily for joint pain on her updated medical history, claiming she was taking it on the advice of her physician. There was blood everywhere during routine scaling.
Cathy’s morning ended with a nervous gentleman who said he was allergic to anesthetic. She could not administer anesthesia until she checked with the man’s physician. In fact, she had to call a physician for each of today’s patients. Of course, the physicians were busy seeing their own patients, just as she was.
Cathy’s afternoon was no better, what with jotting down reminders to contact other providers about new and vertical bony defects on the upper right, requesting bitewings from a dentist who took them six months ago, or contacting the vacationing cardiologist to discuss his recommendations for the man who was still recovering from a heart attack.
What would it be like if …
Driving home, Cathy’s mind drifted to a discussion she had with her sister, Malinda, a nurse. The hospital had received federal incentives to create electronic health records (EHRs), converting their hard copy patient charts into a paperless system, where orders were generated, detailed referrals sent, and documentation completed at a patient’s bedside with a couple of clicks on the keyboard. The simplest example was recording each patient’s height, weight, and blood pressure, and there were 15 required medical criteria in all. Cathy drove home, imagining. What would it be like to integrate the office’s existing practice management software system with cloud computing for all of the dental practices in the United States? Even bigger, consider the efficiencies if she could access a patient’s relevant health information through a secured network, read the highlights from a cover sheet, and find medication or allergy lists with one click. If she needed to collaborate with other professionals involved in her patient’s care, she could send an electronic query instead of playing phone tag — all from the same computer that she uses for periodontal charting. Most importantly, Cathy could practice efficiently and safely with this information at her fingertips.
Current government initiatives
Congress passed the American Recovery and Reinvestment Act (ARRA) in 2009, which has been dubbed “Health Care Reform,” to focus on quality patient care, and the effectiveness, safety, and efficiency of treatment. This Act enabled the U.S. Department of Health and Human Service’s Office of the National Coordinator (ONC) for Health Information Technology (HIT) to fund 82 community colleges to train 3,000 midcareer professionals for six different roles to assist with the reform process. The process will continue for two years. The programs are detailed in the HITECH Act, which stands for Health Information Technology for Economic and Clinical Health.
These individuals will help build the electronic infrastructure to support secure electronic data capture, clinical data integration, and health information exchange. The Act also established 62 Regional Extension Centers throughout the nation to help health care providers adopt electronic health records with less patient disruption and better data capture. The ONC has also sponsored a national information network to manage all the generated data, with this mission: “To achieve better quality, value, and affordability of health and wellness services by establishing the Nationwide Health Information Network (NHIN) as the common, secure, nationwide, interoperable network for exchanging health information, and provide this infrastructure with low adoption barriers.” Several components make up the foundation of NHIN — authentication and certification, vocabulary and message standards, delivery protocols, directories, a trust framework, and security.
What part does dentistry have in the government mandates to improve patient oral health care? The U.S. Department of Health and Human Services (HHS) Oral Health Initiative of 2010 delivers the key message that “Oral health is integral to overall health.” Of course, this is the dental hygienists’ mantra! This initiative uses a systems approach to create and finance programs that emphasize oral health promotion and disease prevention, increase access to care, enhance the oral health workforce, and eliminate oral health disparities. The Health Resources and Services Administration (HRSA), an HHS agency, includes oral health in the first goal of their strategic plan, and speaks of interdisciplinary health teams in their second.
Dr. Bertolami, former president of the American Dental Education Association, put the impact of dental disease in perspective when he authored a special Roll Call article on April 23, 2009. It provided clear evidence to legislators for the need to consider dentistry in health care reform, a year before it was voted into law. He advised that each year millions of productive work hours are lost due to dental disease. Dental disease is also one of the leading causes of school absenteeism for children — children miss 51 million hours of school due to dental problems. Workers lose 164 million work hours because of dental disease. According to the Journal of Dental Education, oral-related illnesses account nationally for 3.6 million days of bed disability and 11.8 million days of restricted activity.
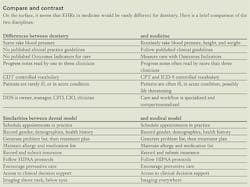
However, the government program missed dentistry’s correlation to medicine, and vice versa. Most of the Meaningful Use directives focus on hospitals, federally qualifying health centers, and physician practices, though dentists are listed as eligible professionals for federal incentives. The patient base of qualifying facilities must represent 30% of those on Medicare or Medicaid, which eliminates many dental practices. Government panels and academicians generally agree that the separation of dental and medical records leads to “incomplete, inaccurate, inefficient, and inadequate treatment of both medical and dental disease.” In advocating the benefits of a team approach to care at the 2010 Institute of Health Conference, Dr. Michael Helgeson highlighted the successful model of the Mayo Clinic. He pointed out that the success of the Mayo Clinic model lies in their philosophy of focusing first and foremost on the needs of patients by bringing together every health care specialty to collaborate in the team diagnosis and treatment of each patient. According to Dr. Rudman et al., there are no national, systematic studies that measure EHR adoption by dentists, but popular belief is that there is low adoption. Certainly the government has missed the point that dental offices deserve realistic incentives to adopt EHRs.
The culmination of government involvement is a Patient Centered Health Home, sometimes called a Medical Dental Home, where there is access to information about current medications and conditions. It also explains historical procedures, such as immunizations or drug reactions, that would be difficult to determine after the fact. To achieve this, the health care system must have interoperability, the buzzword of health information technology, which means that diverse systems and organizations must be able to exchange information. It is the precursor to Health Information Exchange, requiring standards and controlled vocabularies, among other parameters. For example, the computer will not know that “MA” stands for materia alba, or that “endo” is not endoscopy. It will, however, be able to work with clinical documentation in a standardized format, such as SOAP notes. Even more exciting is the ADA’s willingness to investigate whether the standard terminology of SNODENT (Systematic Nomenclature of Dentistry) could adapt to its medical counterpart, SNOMED-CT.
The world according to acronyms
EHRs are required to be certified through the Certification Commission for Health Information Technology (CCHIT), an independent 501(c)3 nonprofit organization, recognized by the U.S. Department of Health and Human Services (HHS) as the official certification body for EHRs in medicine. It checks how well they achieve Meaningful Use requirements, a process that reflects good health practices that have been specified by HHS. Some medical facilities may already have their own electronic medical record (EMR), and while this term is often interchanged with EHR, they are not the same. The alphabet soup gets thicker when people discuss a personal health record (PHR), information electronically stored and maintained by an individual to enable access should they have a medical emergency that leaves them unconscious. An example is Microsoft’s HealthVault (www.healthvault.com). Discussions have begun on electronic dental records (EDR) so that providers have access to information should patients have an out-of-town emergency. Rest assured that complicated encryption methods will keep this information secure in transit, and it will also be password protected.
Achieving synergy
Now add the potential for dental care providers to electronically achieve synergy in patient care with primary care physicians. Dental clinicians are the most likely to recognize periodontal disease in patients at risk for cardiovascular disease, low birth weight babies, bulimia, bruxism, smokeless tobacco use, sleep apnea, xerostomia, or Sjogren’s syndrome. They may also spot evidence of child abuse. A physician will not be aware of decreased bone density in the mandible unless images are on file. In turn, dental professionals should know when a patient has decreased renal function, unstable HbA1c levels, or has undergone chemotherapy and radiation treatments. This is in the doctor’s best interest, too. If dentists do not treat periodontal disease in diabetics, patients will likely experience a systemic inflammatory response as well, which increases their risk for cardiovascular disease, stroke, and other life threatening conditions. Poorly controlled diabetics often have an increased susceptibility to oral disease, and the reverse is also true. Periodontal disease can impact the level of control in diabetes.
The past is forever past
The American health care system has been historically structured as silos. There has been talk of integration, but little integration arrived until the use of technology. How do providers stop thinking about just their silo? Dental professionals must think outside their silo. Where is health care headed? It is headed paperless and integrated. High tech speaker and dentist Dr. Larry Emmott feels that a paperless office changes workflow significantly. He wrote recently, “Work flow can now be described by tasks, not places. The most basic tasks are either clinical or administrative. Secondary tasks are communication and documentation. People are freed from the drudgery of filing, typing, looking for lost records, and doing all the rest of the busywork needed to keep a dead-tree system working.” That translates to more time with patients.
One thing is certain. Health care professionals cannot use technology like we have in the past. Exercising the value of the Internet, health information represents care enhanced by readily available clinical decision support. The advent of mobile devices and wireless connections allows providers to branch out from the practice management system currently used in health care. It creates effective communication not only within the office but also with other health care providers. It also facilitates an efficient workflow with no redundancies. Providers and their staffs also have tools for smarter tracking and reporting of referrals, or the lifespan of various types of restorations.
When providers are able to make a one-stop review of their computer screen that highlights the entire patient chart, and has real-time access to information, they are using technology to complete the task at hand without notes, charts, or phone calls. The fundamentals of health information technology focus on removing the paper shuffle. The space once occupied by paper can be used for revenue generating activities. A patient’s recent bitewings taken on the East Coast can be readily available on the West Coast. Customizable triage questions can facilitate efficient patient screening by an assistant.
Tools for clinical decision support can locate an article about fluoride varnishes in a minute. Electronic prescriptions can have medicine ready for patient pickup on the way home. Reports that use electronic data to compare variables, detect patterns, and track the progress of labs or insurance claims will appear in a standard template on the laptop. Pretreatment estimates will print out before the patient has a chance to swallow. Automated office visit charges will directly feed into the billing system, and insurance claims will be instantaneously submitted. Finally, patients will have their own portal for office information for scheduling appointments or signing up on a waiting list. Does this all sound too good to be true?
Cathy finishes imagining as she pulls into her driveway. She is ready for action. In the foreseeable future, Cathy will begin each query with a click to learn if the physician is aware of the mandible density, for example. Has the patient been tested for a particular anesthetic allergy? Click. She can alert the cardiologist that a patient has confused his prescription regimen, before he must be readmitted to the hospital. She can request and view the bitewings on another visitor. Click. But how do hygienists facilitate these changes in their offices? First and foremost, they must be open to change. They must recognize that there will be intermediate imperfections, and that they can help find solutions. Health information technology has already developed an infrastructure in medicine.
Proactive hygienists can generate use of electronic health records in dentistry. At a minimum, they should stay abreast of developments in the federal program. They can tell patients how easy care is to coordinate with EHRs. They should explore SNOMED-CT and SNODENT to see what has already been accomplished in nomenclature for the future. It appears that these may be the foundation for Health Level Seven, which will be covered in another article. Hygienists can work to establish standards for documentation and protocols for treatment that align with the format required by HITECH because it is vastly different, but working on it is much better than whining about it. They should investigate the necessary steps to form the standards required for CCHIT certification for dental records, and encourage vendors to join in. Eligible professionals have until the end of February 2012 to apply for incentives.
Dr. Michael Glick, editor of JADA, wrote a commentary in 2009 that discussed the patient-centered health home. His succinct conclusion says it all: “A medical home, a dental home, or a patient-centered health home will need staff members who are intimately involved in patient care, especially in coordinating services across the health care system.
“Dentistry is not a subspecialty of medicine, but an autonomous partner in health care delivery. We are health care professionals who happen to be dentists, and we need to ensure that our contribution to overall health and well-being is recognized as essential. The dental community needs to take part in setting health goals for all patients and in forging a system that achieves the best possible health outcomes for all patients. This requires our active involvement in creating the patient-centered health home.”
Cindy Quinn, RDH, BS, has completed 13 courses in the federal Workforce Development Program under the provisions of the HITECH Act, aimed at improving the health care system. As a former clinician, manager, and dental hygiene educator, she is committed to facilitating the implementation of electronic health records into dentistry that will enhance patient care through collaboration with medical care providers. She can be reached at [email protected].
References
• Agency for Healthcare Research and Quality Health IT Update, www.ahrq.gov 4/8/11
• Agency for Healthcare Research and Quality Health IT Update, www.ahrq.gov/research/Feb11/0211RA8.html
• American Dental Association, www.ada.org
• Bertolami CN, “Health Care Reform Must Include Dental Care” opinion page, special to Roll Call, 4/23/09
• Din FM, Powell V, “Call for Integrated Health Care Model That Optimally Supports Chronic Care, Pediatric Care, and Prenatal Care as a Basis for 21st Century EHR Standards And Products.” Pittsburgh, PA: Robert Morris University, 2009.
• Emmott L, “Digital Workflow?” Dental Economics (November 2010) 116 -118
• Glick M, Commentary “A Home Away from Home,” J Am Dent Assoc. 2009 Vol 140, No 2, 140-142
• Institute of Oral Health 2010 Focus Group #1 Whitepaper, comments from Dr. Michael Helgeson, page 9. www.institutefororalhealth.org/2101fg/IOHFeb2010-focus-group-whitepaper.pdf
• Microsoft HealthVault, www.healthvault.com/Industry/index.aspx
• National Health Information Network, www.nhincentral.com
• Office of the National Coordinator for Health Information Technology, www.healthIT.hhs.gov
• Powell VJH, Din FM, “The Medical-Dental Home: Achieving Comprehensive Care for Chronic Illness through Integrating Medical-Dental Care and Data,” Medical Home News 1, 3 (May, 2009): 1, 5-7
• Rudman W, Hart-Hester S, Jones W, et al. “Integrating Medical and Dental Records: A New Frontier in Health Information Management” Journal of AHIMA 81, no.10 (October 2010): 36-39.
• U.S. Department of Health and Human Services, www.hrsa.gov/publichealth/clinical/oralhealth/hhsinitiative.html
• U.S. Department of Health and Human Services,www.hrsa.gov/about/strategicplan/html.
Definitions
• Electronic medical record (EMR) — the legal medical record used within one organization.
• Electronic health record (EHR) — information that conforms to interoperability standards, used across more than one health care organization component (ex: lab, imaging, pharmacy).
• Personal health record (PHR) — electronic data that provides access to your health information readily so it can be shared with care providers and family members, despite geographic differences (ex: medications, immunizations, lab test results), with patient-controlled access.
• Protected health information (PHI) — individually identifiable health information that can be linked to a specific patient. HIPAA defines the type of information and circumstances in which PHI can be used and disclosed.
• Health information exchange (HIE) — a system that enables the exchange of EHR information between hospitals and regions, facilitating the coordination of care.
• Electronic dental record (EDR) — proposed name for the legal dental record.