Pretty in pink
A case can be stated for why dental hygienists need to use lasers in cosmetic cases. Gingiva decontaminated by lasing promotes esthetic success.
by Martha Cortés, DDS
Dentistry is a patient-based profession. What ultimately benefits the American patient is a system that is flexible and allows for a maximum number of patients to receive actual dental care from a professional. The dental hygienist, who is often the first professional a patient sees in a dental office, is a member of a complex and adaptable profession. Fortunately, the public is free of any aberrant view of hygienists; patients perceive the hygienist as non-threatening. This view is what can make the hygienist an important therapeutic factor for patients needing periodontal care.
Bacterial decontamination of the periodontium is easily and viably achieved via laser. Elimination of the microorganisms causing periodontal disease will prevent the disease from manifesting. Who better to perform this task than those already in the preventive capacity within a dental practice? Dental hygiene should be fully implemented for its preventive role. When a procedure involves a dentist or specialist, the problem is well underway and developed as disease.
Eighteen states, including the District of Columbia, do not allow hygienists to perform soft-tissue laser therapy. Approximately 100 million Americans suffer from periodontal disease in varying stages, but only a comparatively minute portion of this population actually receive treatment. Periodontists make up approximately 3 percent of the dentists in the United States, customarily treating gum disease when it is well advanced in the patient. In view of this, it is paramount that patients receive care in the earlier stages of disease, when it is easily treated and managed from a preventive standpoint.
There is an inherent partnership between the dentist and hygienist as they share patients and interact for the patients' ultimate benefit. In many ways, the periodontal care of patients is already in the hands of the hygienists; they perform scaling and root planing. Often, the dentist has no proficiency in dealing with this silent disease, waiting until the problem is no longer manageable before finally sending the patient to be seen by a specialist (or, worse yet, it is never diagnosed). Meanwhile, the patient suffers since the disease was only "managed" and not prevented.
Practitioners need to stop passing these patients from professional to professional. As time passes, the gingival condition becomes worse. If general practitioners cannot take responsibility for their patients' early-stage gum-disease, the hygienist should. Waiting until gum disease becomes significant enough to pass the patient on to a periodontist is not treatment. Treating the first signs of periodontitis with laser — in combination with scaling and root planing — is an efficient and profitable means for all concerned. Since profitability is part of the equation, the patient, hygienist, and dentist all win in different and unique ways.
Since I live in a state where only the doctor is allowed to perform subgingival laser treatment, I must do all of the laser work myself. I use the laser in a multitasked way — often times using it to "pretty up" diseased gums before an esthetic case. Red, swollen gums do not go well with veneers or crowns; they must first be treated if the case is to be an esthetic success. Red, swollen gums are an indication of mild disease that is easily treated by a Nd:YAG laser.
Three cases where periodontal disease was treated with lasers in conjunction with esthetic restorative treatment are described on subsequent pages.
The periodontal connection to lasers
Periodontitis is a silent disease, often remaining undiagnosed for years while it systemically affects the entire body. It has been linked to heart disease, osteoporosis, diabetes, stroke, lung disease and low-weight premature babies. Periodontitis is an infection of the supporting structures of the teeth, which include the alveolar bone, periodontal ligament, attached gingiva, and the mucosa. Bacterial colonies usually are found along the inner mucosa.
The clinical signs of periodontitis are gingival bleeding, gingival redness, gingival enlargement, gingival recession, bacterial exudate, and loss of gingival structure.
The general dentist often ignores periodontal disease, considering it part of a specialist's domain. And it is, when it is at a late stage and no preventive work can be done. However, if caught and diagnosed in the early stages, periodontal disease is curable and treatable with laser therapy. The important factor to remember about laser is the anti-microbial component. Furthermore, it is a conservative and minimally invasive tool and modality.
Once periodontitis is established as a disease within the host, the host/parasite equilibrium is imbalanced, as the host's immune response can no longer return to homeostasis. A consequence of this disease is the breakdown of bone tissue, which worsens with the severity and the duration of the disease. Severe periodontitis is considered an incurable systemic disease, with resulting bone loss, gingival loss, and tooth loss. It is considered completely irreversible as a condition.
One of the ancillary benefits of laser ENAP is bone and ligament regeneration. A significant percentage of cases demonstrate this ancillary benefit to make it more than an occasional side effect. It seems that once bacterial levels are significantly down, the body's regenerative capability kicks in unaided. This is rarely seen in periodontal surgery not involving lasers, which suggests that bacterial levels are not significantly reduced in non-laser modalities. Since dental lasers are a physical and mechanical intervention, bacteria cannot build up immunity as they do with antibiotics, antimicrobial solutions, and drugs.
Furthermore, the bio-modulation initiated by lasers helps to release cytokines and other immune bio-modulators that are necessary for a return to homeostasis and health. The etiology of periodontitis is bacterial infestation; however, the general health of the individual will impact this oral disease. Supplements, especially for intestinal health for example, may aid in complementing periodontal therapy. Periodontitis is a complex disease. A successful return to health requires bacterial elimination, a responsive immune system, healthy eating habits, hygienic maintenance, intestinal and gingival supplementation, and excellent occlusion.
The role of the hygienist is pivotal in the prevention and control of this disease. Tools that easily eliminate bacteria should be provided for everyone in this profession.
Lasers avoid iatrogenic cross-contamination of the periodontium, since the laser remains sterile throughout the whole procedure. Hygiene instruments, on the other hand, are dipped into multiple periodontal pockets, potentially spreading the bacteria that is being removed. In addition, during classical instrumentation of the periodontium without lasers, effective removal of bacterial contamination from the soft tissue that opposes the tooth and the bone cannot be accomplished; as a result, bacterial re-colonization remains a possibility.
Every hygiene department in every state and municipality ought to be equipped with a laser. Every hygienist should be trained in lasers and the necessary protocols involved, as this is a major preventive concern for the health of the American people. Prevention is the key.
Dr. Martha Cortés is past president of the American Academy of Cosmetic Dentistry-New York chapter, and has been an accredited member since 1992. She has served two years as co-chair of dentistry with the American Society of Laser Medicine and Surgery. She is a qualified laser educator, an examiner for laser qualifications for the Academy of Laser Dentistry (ALD) and has a mastership in laser technology through the ALD. She also is a fellow of the American Society for Laser Medicine and Surgery. Dr. Cortés is in private practice in New York City and may be reached by phone at (212) 262-0950, or visit www.cosmeticlasercenter.qpg.com.
Case I
A 25-year-old female presented with multiple problems. The patient had an oral abscess, facial cellulitis, three fractured carious endodontic teeth, a loosely fitting temporary acrylic bridge, edematous soft tissue, foul taste, bad breath, and pain. She was an emergency patient who had avoided the dentist for some time. Besides emergency pain management and treatment, the patient desired beautiful teeth.
I explained that the present condition of her oral cavity would ultimately affect how the esthetics would come out. A structurally sound and functional oral cavity was the first step in creating excellent esthetics.
The patient suffered from moderate periodontal disease, with pockets ranging from 4 mm to 7 mm, requiring immediate attention. Laser ENAP (Excisional New Attachment Protocol), as developed by Drs. Robert Gregg and Delwin McCarthy, was used to eliminate the periodontal disease, promoting gingival health and soft tissue attachment.
With this technique, pockets are not cut or sutured to facilitate future scaling and root planing. The laser is conservatively used to remove inflamed necrotic tissue. At the same time, the bacterial colonization causing the periodontal disease is eliminated. Dental lasers are easy to use, manage, and wield because of the ergonomic pen-like design of the laser handgrip.
The conservative nature of laser ENAP minimizes the loss of soft tissue during surgery, allowing for reattachment. In addition, the technique is minimally painful, and recovery from surgery is quick. Furthermore, laser periodontal surgery is esthetically superior because of its conservative nature.
The laser's fiber-optic tip is premeasured to the pocket depth. The tip is then inserted to the root surface and tilted toward the gingiva until contact with the epithelium. The laser is used to debride the necrotic tissue and to eliminate the bacterial infection. Between 97 and 99 percent of the bacteria that causes periodontal disease is eliminated by the thermal and photo action of the laser.
Starting from the gingival margin, the fiberoptic tip is gradually brought to the depth of the pocket as it is moved horizontally back and forth, removing epithelial margins and inflamed necrotic connective tissue with a sweeping motion. Plume and debris are removed using a high-volume evacuation device. Each pocket is lased for approximately 30 seconds on the inside of each pocket, using 20Hz (pps), and 2.5W cross-sweeps. Ultrasonic scaling and light root planing is then performed. All sites are rinsed and examined for remaining diseased tissue. A final laser sweep is set at 20 Hz with 3W for the final seal. Folded wet gauze is placed and compressed for two minutes at the laser site, holding the tissue in place over the alveolar bone.
Laser can also be used when there is no pocket depth and the gingival zeniths are red and slightly inflamed as in early stage disease. The laser is used gingivally to decontaminate the gum tissue before pockets begin to form and before the bacterial count begins to climb logarithmically.
Laser Settings
Parameters for FR:Nd:YAG set at Duopulse 2000 rated 115 volts and 15 amps/pulse width of 150 microseconds:
- Power: 3.0 watts
- Beam diameter: 320 micrometers
- Repetition rate: 20 Hz or pps (pulses per second)
- Wavelength: 1064 nm
- Exposure time: 30 second per pocket per laser sweep, two consecutive sweeps
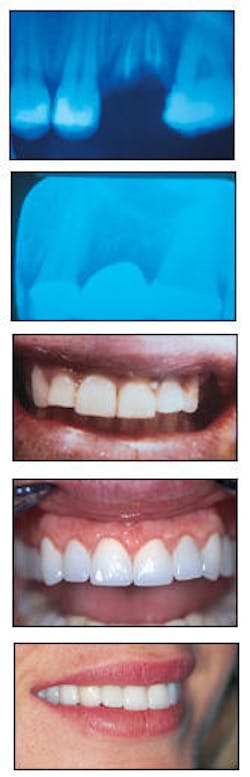
From top to bottom, an emergency visit reveals two abscesses with bone loss and periodontal involvement with teeth #13, 14, and 15; three months after the insertion of the bridge, bone regeneration is visible; appearance at second visit of emergency phase before cosmetic enhancement; appearance after seven veneers, two porcelain-fused-to-gold bridges, two extractions, and periodontal surgery; one year after treatment.
Case II
A woman in her mid-twenties presented for the conservative replacement of an old Maryland bridge. At an early age, she lost her front tooth, and she indicated that she had been embarrassed by the appearance of her smile since then. She wanted an even and natural smile — one that was conservative, life-like, and beautiful. I suggested that she first deal with the health and asperity of her gingival tissue before cosmetically altering her smile since this would enhance the outcome. Her teeth were very dark for a young woman, so I suggested she undergo laser whitening in combination with a passive bleaching method at home.
The patient's teeth previously were restored with an assortment of gold castings, mercury alloys, resin, and porcelain-fused-to-metal restorations. The anterior Maryland bridge was very opaque and had the typical dead-gray shine of the abutment teeth. The smile furthermore suffered from a soft tissue and tooth imbalance. Diagnostic models and photographs were evaluated for the possible placement of a fiber-reinforced composite veneer bridge, which would be biocompatible with the soft tissue of the anterior segment.
Since there was an edentulous space that needed restoring, the soft-tissue aspect needed to be optimized so that the prosthesis will interface with healthy tissue. The patient suffered from moderate gum disease, displayed by periodontal pockets of 4 mm to 6 mm along her anterior maxillary teeth. The esthetic appearance was worsened by asymmetrical gingival margins, where the zenith of the gingival margins did not coincide with her upper lip smile line.
By performing laser ENAP, the bacteria that causes periodontitis was eliminated, and the gingival zeniths and gingiva were made to correspond with the upper lip smile line and canine gingival zeniths. Laser ENAP was performed with three things in mind — evening of the gingival tissue, decontamination of the periodontal pockets, and creating a life-like gingival pontic and abutment to the prosthetic device (where the edentulous space could create an esthetic problem).
The Nd:YAG laser with a 320-micron tip easily negotiates the curves and mucobuccal folds of the gingiva (with a dry field) facilitating the three objectives above. Laser treatment was necessary, because, if the cosmetic portion of the case were to be executed without attending to the early stage disease, the patient would eventually suffer from a progressing and worsening periodontitis. Esthetics requires equally esthetic healthy tissue and teeth in order to be a viable treatment.
Protective eyewear for patient, assistant and doctor, and high-volume evacuation were prepared prior to commencing. The 320-micrometer fiberoptic tip was pre-measured for a 2.5 mm depth and was brought into contact with a circular motion for tissue shaping and decontamination. The Nd:YAG laser sculpts a continuous anterior segment of the gingival margin and corresponding zeniths. This was followed with the fiber in contact with the tissue to reshape the area, followed by 1 mm non-contact-defocus optic laser tip to obtain hemostasis and evacuation of the laser plume. This was followed by the laser ovate pontic preparation.
Laser Settings
Parameters for Nd:YAG set at Duopulse 2000 rated 115 volts and 15 amps:
- Power: 3.0 watts
- Beam diameter: 320 micrometers
- Repetition rate: 20 Hz
- Wavelength: 1064 nm
- Exposure time Two minutes total
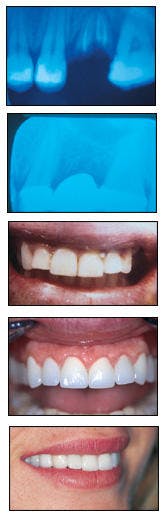
From top to bottom, gingival tissue is red and inflamed prior to treatment; retracted anterior view shows appearance after laser whitening, but before laser ENAP procedure; appearance shows missing lateral incisor #7; restoration of #7 is shown, as well as effect of laser ENAP on tissue; appearance approximately 3½ years after treatment.
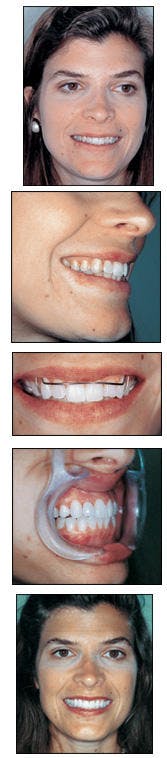
Case III
A female patient presented for an esthetic consultation, desiring to alter what she considered to be dark and twisted teeth. The initial treatment included an exam, a cleaning, oral hygiene instruction, periodontal re-education, soft-tissue laser therapy, passive home bleaching, and orthodontic treatment. This treatment was followed by laser bleaching and two porcelain veneers. Both lateral incisors would receive porcelain laminates, since tooth #7 had a gingival fracture and #10 had an obvious incisal defect. In addition to these defects, both teeth were esthetically shorter than the other anterior teeth.
Again, the gingival health was a concern. The patient had red, inflamed gingival tissue that, if not treated, would diminish the esthetic work. Furthermore, without treatment, the mild periodontitis would most likely evolve into a destructive pathology.
The treatment would benefit the patient's esthetics and, even more so, her long-range health. She was planning for her future, which included a wedding. When she looked at her teeth, she did not see a periodontal issue, only unesthetic teeth. It would have been easier and faster to merely perform a gingivectomy and remove any gingival tissue that was unesthetic and necrotic than perform periodontal laser therapy. The gingival tissue would go well with the bleaching and the new veneers. However, not treating the periodontal infection would render the patient's efforts at esthetic enhancement into failure. With time, the disease would encroach on the temporary health of the gingival tissue.
Every consideration was given for a complete conservative treatment and esthetic restoration in conjunction with soft-tissue health. Laser ENAP was performed with cosmetic enhancement in mind.
Classical instrumentation is combined with laser for microbial decontamination and for the promotion of gingival healing. Surgical treatment is initiated prior to orthodontia and laser bleaching. The laser is utilized to vaporize bacteria, diseased tissue, and pathologic proteins, while conservatively maintaining gingival tissue for future reattachment.
A 320-micrometer fiberoptic tip is pre-measured, and is brought into gingival contact for laser ENAP. Starting from the gingival margin, the fiber is gradually brought to the depth of the pocket as it is moved horizontally back and forth, removing epithelial margins and inflamed necrotic connective tissue with a sweeping motion. Plume and debris are removed using a high-volume evacuation device. Each pocket is lased for approximately 30 seconds, using 20Hz (pps), and 2.5 W cross-sweeps totaling 30 seconds on the inside of each pocket. Ultrasonic scaling and light root planing is then performed. All sites are rinsed and examined for remaining diseased tissue. A final laser sweep is set at 20 Hz with 3W for the final seal. A 1 mm noncontact, defocused optic laser tip is utilized afterward to obtain hemostasis.
Laser Settings
Parameters for Nd:YAG 1064 nm laser set at Duopulse 2000 rated 115 volts and 15 amps:
- Power: 3.0 watts
- Beam diameter: 320 micrometers
- Repetition rate: 20 Hz
- Wavelength: 1064 nm
- Exposure time: Approximately 30 seconds per pocket
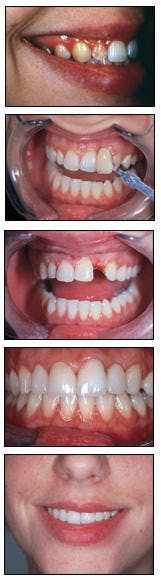
From top to bottom, the patient's appearance before treatment; the gingival condition is apparent in lateral view of smile; appearance after six months of orthodontic treatment before cosmetic enhancement; lateral view after treatment; patient's appearance after laser whitening, laser periodontal therapy, orthodontics, and two veneers on teeth #7 and #10.