Slaking the Dryness
Detect symptoms of xerostomia and help patients obtain relief from the side effects.
Frances Dean Wolfe
A 62-year-old patient complains of constant thirst, which she attributes to her recently diagnosed diabetes. A 58-year-old female patient, who has recently undergone chemotherapy and radiation treatment following thyroid cancer, shows signs of deteriorating oral hygiene. Her gums are inflamed, and her plaque scores are out of sight. She complains of extreme thirst brought on by the cancer treatment. A 78-year-old grandfather complains of difficulty in retaining his full upper denture. Upon checking his updated medical history, you notice he is under his physician`s care and taking prescription drugs for urinary incontinence and depression.
What`s the common bond linking these patients? Each is suffering from xerostomia (dry mouth), a symptom caused by systemic medical conditions, medical treatments (including prescribed medications), or disease. Xerostomia itself is not a disease or a condition, but rather a symptom. Although it is most frequently associated with alterations of salivary function, xerostomia is not a reliable indicator of salivary hypofunction and should not be used as a diagnosis. While often attributed to the aging process, xerostomia is not a normal condition of aging. With improved home care regimens, hygienists can help each of these patients cope with the symptoms.
Many systemic diseases and conditions may reduce adequate salivary flow, resulting in xerostomia. The most common are medications and radiation treatment, and systemic disease.
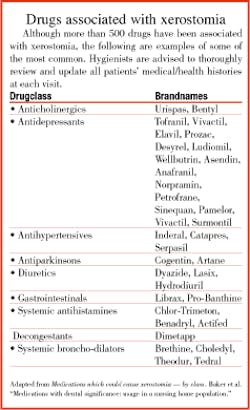
Medications - Xerostomia is associated with as many as 500 prescription and over-the-counter classes of drugs (see the related table for drugs associated with xerostomia), including:
- anorexiants
- antiacnes
- antianxieties
- anticholinergics/antispasmodics
- anticonvulsants
- antidepressants
- antidiarrheals
- antihistamines and decongestants
- antihypertensives
- antiflammatories and narcotic analgesics
- antimetabolites
- antinauseants
- antiparkinsonians
- antipsychotics
- bronchodilators
- diuretics
- muscle relaxants
- narcotic analgesics
- quinolones
- sedatives and tranquilizers
It should be noted that when patients take a combination of any of these types of medications, there is an increased likelihood of a synergistic effect of xerostomia.
Radiation treatment - Approximately 40,000 patients in the United States are treated annually for head and neck cancers using ionizing radiation. When salivary glands are within the fields of radiation, as they are in the majority of cases of head and neck cancers, marked salivary gland hypofunction results.
Salivary dysfunction is often severe and oral sequelae are problematic. Salivary dysfunction may also result from internal sources of radiation, such as treatment of thyroid carcinoma with radioactive iodine.
Systemic diseases - Numerous systemic diseases cause salivary dysfunction and xerostomia. The most common is Sjogren`s syndrome, an autoimmune exocrinopathy. This is the second most common rheumatic disorder and can occur alone (primarily Sjogren`s syndrome) or in conjunction with another connective tissue disease (secondary Sjogren`s syndrome). Conditions associated with Sjogren`s syndrome include rheumatoid arthritis, systemic lupus erythematosus, and primary biliary cirrhosis. All Sjogren`s syndrome patients complain of xerostomia and dry eyes; they also have measurable secretory hypofunction. It is estimated that more than 1 million Americans have Sjogren`s syndrome, most of them undiagnosed; approximately 90 percent are females of perimenopausal or menopausal age.
Other disorders or conditions associated with salivary dysfunction include cystic fibrosis, sarcoidoses, poorly controlled diabetes mellitus, thyroid disorders, and depression. Numerous others include: HIV infection, affective disorder, metabolic disturbances, hepatic disease (cirrhosis), thyroid disorders, autoimmune diseases, sarcoidosis, autonomic dysfunction, dementia (Alzheimer`s disease), and neurologic diseases (Bell`s palsy, cerebral palsy, and parkinsonism).
Xerostomia and elderly patients
Once thought to be an inevitable result of aging, xerostomia is no longer considered an unavoidable ailment of old age. Numerous studies, for example, have shown that parotid gland output and composition remain stable across the human life span. In most cases where xerostomia exists in older patients, it can be attributed to systemic disease, prescription drugs, or other medical treatments.
Decreased salivary flow may predispose older adults to increased decay, especially Class V and periodontal disease. It also may contribute significantly to problems associated with inability to retain full and partial removable dentures. It also may limit a patient`s quality of life and comfort by impairing eating, chewing, swallowing, or normal speaking. In some cases, xerostomia may cause older patients to become socially withdrawn from friends and family members due to the inability to eat at a restaurant, adequately hold a denture in place, or to speak confidently.
Drugs associated with xerostomia may predispose older patients to higher caries incidence, difficulty in mastication, salivary gland swelling and pain, stomatitis, burning mouth and tongue, and oral candidiasis.
Clinical signs of salivary gland dysfunction include dry, chapped lips; pale, dry oral mucosal surfaces; thinned or atrophic mucosa; reddened, furrowed, coated, or depapillated tongue surfaces; absence of a salivary pool in the floor of the oral cavity; presence of shed epithelial cells coating dentition of mucosal surfaces; caries, specifically involving the cervical surfaces or incisal edges; and fungal infections.
The major salivary glands may present as enlarged, and there may be reduced flow upon manual saliva expression. Often, the expressed saliva appears thickened or cloudy; saliva may appear frothy or viscous. The patient may experience difficulty in swallowing without added fluids or the swallowing time may be prolonged.
Symptoms found in xerostomic patients include complaint of dryness of the lips, throat, or nose, in addition to a dry mouth. Other symptoms of xerostomia include difficulty in speaking, or chewing or swallowing dry foods. Patients may report a dry cough and a history of recurrent oral or salivary gland infections with periodic enlargement of the major salivary glands.
Xerostomia and the hygienist
Saliva plays an important role in maintaining dental health because it performs a variety of functions, including lubrication, buffering of acids produced by oral bacteria, remineralization of tooth surfaces, and antibacterial action.
The dental hygienist should be aware that xerostomia may lead to a variety of adverse oral conditions, including:
- Increased plaque index
- Slower healing of gingivitis
- Soft tissue changes
- Root caries (specifically)
- Increased caries activity (generally)
- Halitosis
As often is the case, the hygienist has the first clinical contact with the patient. The dental hygienist must ensure that all medical histories are kept current. When taking a medical history on a new patient, it is important to note all drugs currently being taken and the dosage. This applies to prescription and over-the-counter medications, as well as supplements. Many patients are unaware that readily available over-the-counter drugs and food supplements may have potentially serious side effects or synergistic interactions with other prescription drugs.
When patients of record return for recall appointments, it is important to ask, "Has there been any change in your medical history or drug intake since your last visit with us?" These changes should be noted on the chart by the hygienist along with his or her initials and the date (an important risk-reduction step).
The dentist needs to be alerted if a patient may be taking a prescribed drug associated with xerostomia. The dentist may choose to consult with the patient`s physician to discuss whether changes in medication can be made to reduce risk and to restore the patient to optimal oral health.
Available treatment options
Treatments available for xerostomic patients include artificial salivary substitutes that containing glycerin as a lubricant, a sugarfree sweetener such as sorbitol or flavoring agent (xylitol), paraban as a preservative, and carboxymethycellulose to impart the viscous texture of saliva (see the related table for more information about saliva substitutes). Commonly recommended dry mouth remedies include Xero-Lube®, Salivart®, and Saliva Substitute®. Home-use dental fluoride gels or rinses for caries prevention and enamel remineralization are also effective.
Kelly Schest, a hygienist in Phoenix, recommends Biotene® products. "My xerostomia patients see marked improvement when they use the antibacterial toothpaste, mouth rinse, Oral Balance gel and Biotene gum," she says. "All of these products are alcohol-free," she adds.
Schest recalls two specific patients with xerostomia whom she has treated for several years. "One is a gentleman with a history of oral cancer who has undergone seven surgeries and radiation treatment," she says. "He has practically no saliva and survives on Biotene products." She adds that he takes Saligen® and carries a water bottle with him at all times. "He is 40, has retained all of his natural teeth, has immaculate home care, and uses a powered toothbrush," she says.
She also treats another xerostomic patient, a woman who had a thyroid tumor and radiation treatment. She also uses Biotene products.
"We do an in-office fluoride treatment for both of these patients every three months," says Kelly. "This particular patient used to apply fluoride at home but now likes the quick-dissolving cherry-flavored, troche, Lozi-Flur®." Kelly has found that the tray method used with acidulated phosphate fluoride creates pits in porcelain crowns and feels "like sandpaper."
Patients suffering from xerostomia should be instructed to stimulate salivary flow at liberty to bathe the oral tissues, to reduce bacterial adherence, and to keep the oral cavity moist. Some hygienists also recommend sugar-free gum or candies (lemon or sour cherry) containing sorbitol or xylitol to aid in the stimulation of saliva production. A noteworthy side-effect of either of these ingredients, if used in excess, is diarrhea.
Patients may obtain some relief of symptoms by:
- Sipping water frequently all day long
- Letting ice chips melt in the mouth
- Restricting caffeine, sugar, and cola intake
- Avoiding mouth rinses containing alcohol
- Humidifying the sleeping area
- Coating the lips with Blistex™, Vaseline™ or A&D Ointment™
For patients who are especially susceptible to a high risk of caries, the hygienist may recommend a series of in-office fluoride treatments or home applications of additional fluoride in the form of gels, rinses, or mouthwashes as a proactive measure to help preserve the natural teeth.
Patients receiving radiation or chemotherapy may be especially susceptible to xerostomia-associated rampant caries resulting in tooth loss. Often, patients with extremely high risk for caries in this phase of cancer treatment will be scheduled to return for very frequent recall visits in which the dentist will check for new caries and changes in the soft tissues.
Patients who have some or all of their natural dentition may be instructed to use the amount of saliva substitute recommended by the manufacturer on the printed directions provided. These products, specifically made to relieve the symptoms of xerostomia, include dry mouth toothpaste, chewing gum, and antibacterial (alcohol-free) mouthwash (Biotene™, Laclede).
Edentulous patients with full dentures can be instructed to apply a small amount of moisturizing gel (Oralbalance™, Laclede) on the inside of the denture, creating a "smear" layer between the oral tissue and the inside of the denture. They should also be instructed to remove the denture and reapply small amounts of Oralbalance™ during the day as needed.
The hygienist is often the first person to detect the clinical signs and symptoms of xerostomia. Working with the patient, the hygienist can be an effective educator and coach in helping patients relieve and control the uncomfortable side effects associated with xerostomia.
Frances Dean Wolfe is the pen name of a frequent contributor to RDH.
References:
- Astor, F. et al. Xerostomia: A prevalent condition in the elderly. ENT-Ear, Nose & Throat Journal. Volume 78, Number 7. July 1999.
- Bachiman, R: Dental Caries in Older Adults: Current Status and Management. NYSDJ, Vol 62, #6. June/July 1996.
- Berg, R. et al: Dentistry and Aging Patients. Quintessence International, Vol 28, #9. Sept. 1997.
- Biocare(tm) Advanced Oral Care Systems: Why is Oral Care Important? (undated)
- Biotene(r) Oral Balance Dry Mouth Hawaii Drawing Contest Winning Letter. RDH, October 1999.
- Bray, K. et al: Epidemiology of Oral Diseases in Older Adults. ACCESS: ADHA, Chicago. Vol. 11, #10. Dec 1997.
- Clinician`s Guide to Treatment of Common Oral Conditions. The American Academy of Oral Medicine. Spring 1997.
- Dietz, E. Causes and Treatment of Xerostomia (Dry Mouth). One-credit accredited continuing education course. The Explorer: NADA, Falls Church, VA. 1999.
- Dietz, E: Geriatric Dentistry: Dental Issues Relevant to the Aging Population. GSC Home Study Program, 1999.
- Dietz, E: Premedication for Dental Patients. GSC Home Study Program, 1998.
- Fox, C. Management of Dry Mouth. Dental Clinics of North America. Volume 41, Number 4. October 1997.
- Haveman, W. et al. Dental management and Treatment of Xerostomic Patients. Texas Dental Journal, Volume 115, Number 6. June 1998.
- Joko, A. et al: Dissatisfaction with Oral Health Status in an Older Adult Population. J Public Health Dent Vol 57, #1. Winter 1997.
- Jones, J. et al: Restorative Considerations for Aging Baby Boomers. Quintessence International, Vol 28, #9. Sept. 1997.
- Lynch, P: Xerostomia: What`s Hot and What`s Not. Western Regions 8th Biannual Oral health Conference, Sedona, AZ. Aug 1999.
- Iacopino, A: Understanding and Treating Aging Patients. Quintessence International, Vol 28, #9. Sept. 1997.
- ICP Medical Questions and Answers/OralBalance and Biotene (undated).
- Mallatt, M: Preventive strategies for the older dental patient. IDA Jour, Vol 76, #4. Winter 1997-98.
- Niessen, L. et al: Oral Health for a Lifetime: Preventive Strategies for the Older Adult. Quintessence International, Vol 28, #9. Sept. 1997.
- Rosenthal, L: The Art of Aging: The Fountain of Youth. Quintessence International, Vol 28, #9. Sept. 1997.
- Shay, K.: Older Dental Patients: Myths and Realities. Dental Hygienist News. Vol 9, #3. 1996.
- Sreebny, L. et al: A reference guide to drugs and dry mouth-2nd edition. Gerodentology Volume 14, Number 1. July 1997.
- Wind, Denisa A., RDH. Management of Xerostomia: An Overview. Journal of Practical Hygiene. September 1996.
- Xerostomia: Examples of Some Drugs Causing Dry Mouth. Product brochure published Laclede, Inc., Rancho Dominguez, CA.