Risky business
Following the trail of infection prevention to discover the safest course of action
By Rachael C. Dorn, RDH, MSDH
Infection prevention is at the core of everything we do as dental professionals. During the scope of our days, we can sometimes forget that the risk to us and our patients is very real. According to Business Insider, dental professionals are at the top of the 37 riskiest jobs to personal health. Hygienists rank number one, dentists rank number two, and dental assistants rank number five.1
The Centers for Disease Control and Prevention (CDC), Food and Drug Administration (FDA), and the Environmental Protection Agency (EPA) all play roles in infection prevention. There are many groups that publish regulations and recommendations; therefore, it is important as dental professionals to know the differences in the groups.
Recommendations are made by groups that often do not have the authority to enforce compliance. Examples include the American Dental Association (ADA), the Organization for Safety, Asepsis and Prevention (OSAP), and the CDC. The CDC makes recommendations only on infection control, and these are not binding or mandatory. However, state dental boards can determine that all dental professionals must follow the CDC recommendations, thereby making them mandatory. However, regulations are made by groups that have the authority to enforce compliance, such as the Occupational Safety and Health Administration (OSHA), the FDA, and the EPA. These regulations are mandatory to follow and if not followed will result in violations and penalties.
Instrument processing
Proper instrument processing is critical to protect patients and clinicians from bloodborne pathogens and enveloped viruses. The presence of specific disease-producing organisms is rarely known; therefore, application of protective equipment is needed before, during, and after all patient appointments.
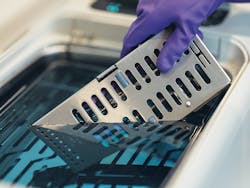
When exposure to bloodborne pathogens is possible, it is mandated under OSHA’s Bloodborne Pathogens Standard to wear puncture-resistant gloves. To prepare for transport, instruments should be placed in an appropriate container at the point of use to prevent percutaneous injuries. Contaminated instruments should be transported in instrument cassettes, trays with sides, or labeled containers with lids when cassettes are not an option. Published in the guidelines by the CDC, occupational safety must be followed by clinicians to reduce the risk of sharps injuries and exposure to contaminated instruments.2 There should be minimal handling of loose contaminated instruments during transport to the instrument reprocessing area.
There are considerations to be made when dental professionals select their cleaning methods and equipment. The CDC states, “Using automated equipment can be more efficient and safer than manually cleaning contaminated instruments.”2 Automated equipment such as ultrasonic baths and instrument washer disinfectors are the methods of choice for many practices for removing debris from instruments before sterilization. Once the instruments are sterilized in FDA-approved packaging, it’s important to store them unopened in a clean, dry cabinet. Instruments that are stored without sealed wrappers are only momentarily sterile because of airborne contaminants.3
Hand hygiene
Hand hygiene, including handwashing, is critical for reducing the bacterial flora of the hands, and is considered the most important single procedure for the prevention of cross contamination.3 Hand hygiene should be performed whenever hands are visibly soiled, before donning and after removing gloves, and before donning new gloves if swapping them out during a procedure (due to loss of integrity).2 In 2016, the FDA issued a final rule saying that over-the-counter (OTC) consumer antiseptic wash products (not designed for health use) containing certain active ingredients, such as triclosan and triclocarban, can no longer be marketed. Companies will no longer be able to market antibacterial washes with these ingredients because manufacturers did not demonstrate that the ingredients are both safe for long-term daily use and more effective than plain soap and water in preventing illness and the spread of certain infections.4
Fingernails should be kept clean and smoothly trimmed to prevent breaks where microorganisms can enter. According to multiple studies, artificial nails are associated with bacterial pathogens and fungal infections and are not recommended for clinicians. In addition to artificial nails, rings and nail polish are not recommended because chipped fingernail polish and skin under the rings may harbor bacteria.5,6
Surface disinfection
There are many different microorganisms that can last on a multitude of surfaces for days, even months. Best practice is to use barrier protections on all surfaces that someone will be touching. It is extremely important for all health-care workers to understand and use disinfectants that follow the guidelines for disease prevention to protect themselves and patients. On a daily basis we are subjected to blood and other potentially infectious waste, and we need to ensure we’re cleaning with appropriate chemicals.
According to the CDC, an intermediate-level disinfectant with a tuberculocidal claim should be used when a surface is visibly contaminated with blood.2 In addition, the disinfectant should be a germicide that is EPA-registered as a hospital disinfectant. The EPA registration number is on the packaging. Most products contain a disinfectant and cleaning agent (detergent). The product label verifies whether the product is designed for a one- or two-step process. Kill times for various organisms should be considered, including for TB and HIV/HBV. The product must remain wet on the surface for that length of time to kill the microorganisms. It is important to be aware of this time and how it will affect your workflow.2
Specialties
Hygienists recognize the importance of high-volume evacuation during preventive procedures, especially when using powered instruments. Keeping the high-volume evacuation lines clean helps prevent vacuum pump failures. The EPA identifies the guidelines for evacuation line cleaning, and in 2017 it published new guidelines specifically addressing amalgam separation and evacuation line cleaners.
Due to these regulation changes that are to be implemented by clinicians, manufacturers are working to create new and innovative products to support us in our infection prevention efforts. An example of this is Purevac SC, a neutral pH formula evacuation cleaner from Dentsply Sirona. Part of the Practice Protect range of products, Purevac SC removes a wide range of dental debris, and is nonfoaming and biodegradable. The Purevac system includes a walkabout, which is a bucket that can serve up to four operatories at a time.
An important point to remember regarding suction lines is backflow. Creating a tight seal around the saliva ejector can potentially pull fluids from suction lines back into a patient’s mouth. The CDC recommends that dental health-care professionals do not advise patients to close their lips tightly around the tip of the saliva ejector.7 This reduces the risk of debris in the suction line being aspirated into another patient.
Disposables
The CDC recommends single-use disposable items whenever possible. These must be discarded after use with a single patient during a single visit. Single-use disposables offer a number of advantages, including no need for reprocessing, which saves time and effort. They also improve patient safety by eliminating the risk of patient-to-patient contamination because the item is discarded and not used on other patient.8
These disposables are typically made of plastic or inexpensive metals so they are not heat tolerant, and they should never be reused. Many dental professionals may not know that single-use disposables carry a circular image that shows the number 2 with a diagonal line through it. This denotes that the object may not be used a second time.
High quality disposable air and water syringes with separate air and water channels designed to help minimize air and water crossover are recommended. Other examples of single-use disposables include bib clips/bib chains, single-use diamond burs and endodontic files, single-unit fluoride varnish units and applicators, prophy angles, cups and brushes, traps, high volume evacuation suction tips, and saliva ejectors.
Masks are also important and should be chosen carefully based on the procedure. A recent dental study stated, “All procedures performed with the use of dental unit handpieces cause the formation of aerosol and splatter, which are commonly contaminated with bacteria, viruses, fungi, and often also with blood.”9
The American Society of Testing and Materials (ASTM) provides specifications for face masks used in providing dental and medical care. An ASTM-1 mask is used only when low amounts of splatter, spray, or aerosol generation is anticipated. These procedures include patient exams, operatory cleanup, lab trimming and finishing, impressions, and orthodontic care. For procedures with low to moderate fluid or aerosols and/or sprays, including sealants and prophylaxis, an ASTM-2 level mask is recommended. For procedures with moderate to heavy fluid, aerosols, and/or sprays, an ASTM-3 level mask is required. These procedures include the use of an ultrasonic scaler and piezo scaler with water or periodontal surgery.
It is important to replace masks after each patient or when visibly soiled or wet. Characteristics of an ideal face mask include fitting snugly around the entire edges of the mask, no fogging of eyewear, material that does not irritate the skin, and does not collapse when wet. Lastly, to remove your mask, avoid touching the outside of the contaminated mask, grasp the ear loops, lift the mask off your face, and dispose of in the trash.9
Summary
Successful infection prevention depends on the cooperative efforts of the entire dental team. As dental professionals, we have an obligation to serve all patients with comprehensive care and to deliver that care in a safe environment. Remember the difference between regulations and recommendations, and apply them in your everyday practices. To assist dental professionals, manufacturers continue to design instruments and equipment to not only meet our clinical and patient needs, but also with infection prevention in mind to help us meet requirements and regulations. Some are also making it easier to find products by color coding the product lines to eliminate confusion, and by matching universal color coding standards, such as the Practice Protect range of products. With good infection prevention strategies, we can protect ourselves and our patients and stop the spread of infectious diseases.
Rachael Dorn, RDH, MSDH, is a global clinical education curriculum developer for Dentsply Sirona. She received her master’s degree in dental hygiene education and research from Old Dominion University. She holds a BS in dental hygiene with an emphasis in health policy and administration from Pennsylvania College of Technology, and an associate degree in dental hygiene from Allegany College of Maryland. She has been a clinical hygienist for 12 years, and was an instructor in an accredited dental hygiene school. She can be contacted at [email protected].
References
1. The 37 jobs that are most damaging to your health. Business Insider website. http://www.buinessinsider.com/most-unhealthy-jobs-in-america-2017-4/#34-tie-radiologist-1. April 2017.
2. CDC. Guidelines for infection control in dental health-care settings–2003. MMWR 2003; 52 (No. RR-17): 1-66.
3. Wilkins EM. Clinical Practice of the Dental Hygienist. Philadelphia: Wolters Kluwer. 2017.
4. FDA. 2016. Food and Drug Administration website. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm517478.htm.
5. Arrowsmith VA, Taylor R. Removal of nail polish and finger rings to prevent surgical infection. Cochrane Database Syst Rev. 2012;5:CD003325.
6. World Health Organization. WHO Guidelines on Hand Hygiene in Health Care. 2009. http://apps.who.int/iris/bitstream/10665/44102/1/9789241597906_eng.pdf.
7. CDC. Frequently asked questions. Saliva Ejector & Backflow https://www.cdc.gov/oralhealth/infectioncontrol/questions/saliva.html.
8. Single-use (disposable) devices. Centers for Disease Control and Prevention website. https://www.cdc.gov/oralhealth/infectioncontrol/questions/single-use-devices.html.
9. Dental Advisor. Translating the science. October 2014. https://www.dentaladvisor.com/pdf-download/?pdf_url=wp-content/uploads/2015/02/face-masks-what-to-wear-and-when.pdf.