When are bitewings not enough?
A cause for concern among pediatric patients
By Sarah Fenlon, RDH, BS
We know, of course, that bitewings are an integral tool for assessing dental and periodontal health. What warrants additional radiography? What should we be on the lookout for, and what can these findings tell us? This article will focus on the clinical and radiographic findings in the primary and mixed dentition that may call for additional diagnostics, specialized treatment planning, and/or referrals to specialists.
Three of the permanent first molars have erupted in your seven-year-old patient. Where is tooth No. 3? Upon exposing routine bitewings, you find that pesky molar resorbing the distal portion of the upper right primary second molar. This evidence of ectopic eruption may or may not warrant additional radiography. But it is crucial that a decision is made about what can be done to arrest or correct this process.
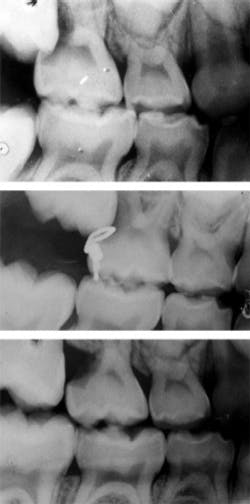
A viable option is the extraction of tooth A in order to allow for eruption of tooth No. 3. The lost space can then be gained with orthodontia, with hopes that No. 4 will erupt without compromise. An orthodontic consultation, however, should be considered prior to the extraction. Another option is the brass wire technique, as demonstrated in Figure 1.
An eight-year-old patient’s maxillary left central incisor has erupted in crossbite. Her other three maxillary incisors have erupted in proper occlusion. Radiography, possibly an occlusal radiograph, may reveal a mesiodens. This mesiodens would most likely be located palatal to the root of tooth No. 9, pushing the apex labially and thus causing the crown to erupt lingually.
Other indications that a mesiodens may be present include an asymmetrical eruption pattern of the maxillary incisors or unexplained delayed eruption of maxillary incisors.1 The diagnosing doctor will decide whether surgical management and/or orthodontic treatment are necessary.
In another example, the clinician takes a set of bitewings on a nine-year-old patient. You would expect to see evidence of the permanent premolars preparing to erupt. The lower first premolars are raring to go, but, in place of the second premolars, you find only trabecular bone. This would most likely warrant a periapical or a panoramic radiograph to assess for congenitally missing teeth. Inquiring about a family history of agenesis is another helpful clue in this diagnosis. Based on the patient’s dental age, the diagnosing dentist would most likely make a decision as to when would be the appropriate time for an orthodontic evaluation.
Submergence in the primary dentition can be a clinical clue that the successor is absent. A submerged deciduous molar is also typically assessed for ankylosis, another condition that is related to submergence. A periapical exposure can be used to determine whether the periodontal ligament space is obliterated and thus the tooth is ankylosed. Percussion testing may reveal a more solid sound when compared to teeth that are not ankylosed. The periapical should also be sufficient evidence as to whether or not the succedaneous tooth is present.
Treatment of the submerged tooth depends on the “degree of submergence, presence or absence of a successor, and the relationship of the adjacent and opposing teeth.”2 A submerged tooth with a successor may be extracted and replaced with a space maintainer, or monitored for normal exfoliation. If the latter option is elected, the function of the submerged molar can be maintained using a crown or resin buildup. This will help prevent adjacent teeth from tipping into the space not occupied, and prevent supraeruption of teeth in the opposing arch.2 The recommended treatment for an ankylosed primary molar is extraction followed by orthodontics.3
Three of the four primary canines have exfoliated in your 11-year-old patient, and the successors are erupting. The fourth deciduous canine is still present and nonmobile, with no signs of the clinical crown of the successor. Negative findings when observing and palpating for the canine eminence may indicate an ectopic, impacted, or, although rare, congenitally missing permanent canine. Radiography, usually a panoramic, will aid in diagnosis. Localization of an ectopic canine can be accomplished using the buccal object rule, where two periapicals are taken of the canine, and the mantra “same lingual, opposite buccal” is applied. Expose one periapical as a reference point. For the second film, angle the X-ray tube head from a more distal point.
Did the canine appear to move distally (or in the “same” direction as the tube head)? This indicates that the canine is located palatally (“lingual”), as seen in the majority of cases.4 Did the canine appear to move mesially (or “opposite”)? This indicates that the canine is located buccally. Extraction of the deciduous canine may be necessary to facilitate repositioning of the permanent canine, whether by spontaneous eruption or through surgical exposure and orthodontic treatment.
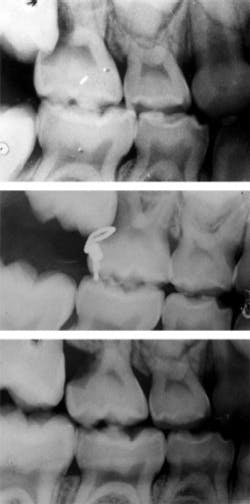
Other findings also often require orthodontic intervention. Posterior crossbites, whether unilateral or bilateral, require orthodontic treatment to correct. Early exfoliation of deciduous teeth (such as lower primary canine exfoliation upon eruption of permanent lateral incisor), or delayed eruption of permanent teeth may also warrant orthodontic involvement to allow for a proper and stable eruption of permanent teeth. Mobility of the permanent dentition, which may present itself in incisors as ectopic canines resorb their roots (see Figure 2), can also be a cause for concern and requires additional evaluation.
The review of these conditions should remind you what tools can be used by you and the treating dentist to best determine the needs of your patient. Our patients rely on us to use our knowledge for their individual needs, and knowing which findings may require further evaluation helps us to do just that. Whether your patient population is comprised of few children or you work in a pediatric practice, keeping a firm grasp on this basic knowledge will have an impact on their future dental health.
Sarah Fenlon, RDH, CDA, BS, is a practicing clinician in the greater Boston, Massachusetts, area. Her multi-specialty work week consists of pediatrics, orthodontics, and general dentistry.
References
1. American Academy of Pediatric Dentistry: Guideline on Pediatric Oral Surgery. Pediatric Dentistry 2010; Reference Manual 33:256.
2. Shekar I. Multiple submerged primary molars. A case report. Saudi Dental Journal 2003; 15:149-50.
3. Ngan P, Heinrichs D, Hodnett S. Early management of congenitally missing mandibular second premolars: a review. Hong Kong Dent J 2011; 8:41.
4. McSherry PF. Ectopic maxillary canine: A review. Br Journal of Orthodontics 1998; 25:209.
Past RDH Issues