Oral Exams: Are you performing a complete exam?
by Leslie DeLong, RDH, MHA,
and Nancy Burkhart, RDH, BS, MEd, EdD
Educators view dental hygiene students with enthusiasm, and students have the sincere hope that they can change the lives of patients by providing excellent care. Students are educated in an ideal environment and required to practice under the scrutiny of professionals who demand the highest standards in treatment. It is hoped that students who are taught these high standards will practice them after graduation. However, once students graduate and enter private practice, they often enter less than perfect environments and develop poor work habits and short cuts that alter the valued priorities of the academic setting. Many hygienists and even dentists admit they no longer spend time performing the thorough oral screening exam they learned in school.
The purpose of this article is to encourage clinicians who are providing this service to (1) continue to do so, (2) motivate other clinicians to provide this service, and (3) review appropriate technique, documentation and referral protocols. The American Cancer Society estimates that 34,360 new cases of oral cavity and pharyngeal cancer will be diagnosed in 2007, and that 7,550 deaths from oral and pharyngeal cancer will occur in 2007.1 The five-year and 10-year survival rates for oral and pharyngeal cancers are 60 percent and 48 percent respectively.1 This five-year survival rate is one of the lowest of all major cancers because a majority of the lesions are not diagnosed until they are more advanced.
Early detection increases the chances of survival. However, between 1990 and 1995, 36 percent of oral and pharyngeal cancers were diagnosed at Stage 1 (localized), leaving 64 percent of victims diagnosed during later stages.2 What is our response to this information? What can we do? Public service announcements have raised awareness to the benefits of oral cancer screening exams, but many individuals still do not seek annual dental care. Using data from the National Health and Nutrition Examination Survey for 1999 through 2004, the Centers for Disease Control and Prevention (CDC) reports that approximately 60 percent of adults ages 20 to 64 had at least one dental visit during the previous year.3 Sixty percent is a significant number of people with access to dental professionals who can provide oral cancer screenings, yet in 1998 only 13 percent of adults taking part in the National Health Interview Survey reported having an exam to detect oral and pharyngeal cancers.4
A recent Florida study noted that 19.5 percent of adults reported having an oral cancer screening exam after being told the steps preformed in completing an oral cancer screening.5 Why did so few patients report that they had an oral cancer screening exam during their dental visits? Two studies found that dental hygienists do not consistently provide oral cancer screening exams for their patients even though a majority know it should be done.6,7 In March of 2004, Case Western Reserve University’s School of Dental Medicine presented the results of a similar survey to the annual research meeting of the American Dental Education Association. Their results showed that although hygienists place a high value on oral cancer screening, only 53 percent actually do the exams on their patients. Another interesting finding from the study was that the level of knowledge about oral cancer, specifically the causes, appearance and risk factors, among the dental hygienists surveyed was comparable to that of the general dentists who responded to similar survey questions.8 Dental hygienists are not the only oral health providers who are falling short of their ethical responsibilities. One 1995 study reported that 34 percent of dentists and 37 percent of physicians did not feel that early detection was an important means of reducing morbidity and mortality associated with oral and pharyngeal cancers.9 Another study found that only 14 percent of dentists performed all aspects of the head and neck and intraoral exam.10
Only 57.7 percent of the dental students in a 2005 study done in South Carolina knew all of the components of a tongue examination.11 A 2007 study found that 92 percent of Illinois dentists reported providing oral cancer screening examinations, but many were not being done correctly or at the appropriate intervals.12 Healthy People 2010 addresses the detection and diagnosis of oral and pharyngeal cancers with these two goals:
• Goal 21-7. Increase the proportion of adults who, in the past 12 months, report having had an examination to detect oral and pharyngeal cancers (Target: 20 percent).13
•Goal 21-6. Increase the proportion of oral and pharyngeal cancers detected at the earliest stage (Target: 50 percent).13
The dental community must maintain an appropriate level of knowledge about oral cancer detection and diagnosis, provide appropriate oral exams, and educate the public about oral cancer and its risk factors. In addition, as all dental professionals are aware, the head and neck and intraoral exams are not done solely to identify pre-malignant and malignant lesions. While the immediate emphasis may be to identify these lesions, there are many other reasons to perform these exams. Refer to Table 1 for objectives of the head and neck and intraoral examination.
These exams are crucial for identifying many systemic conditions that may be present in or around the oral cavity as well as localized oral conditions that need to be treated or followed by the dental professional. For example, chronic aphthous-like ulcerations may be the first indication of Crohn’s disease. A patient may have other clues in their medical history that might cause the dental professional to refer to a physician for a complete evaluation. Also, the hygienist may be suspicious of intraoral trauma in a child and be the first professional to identify physical abuse.
Every dental hygienist learns how to perform a complete head and neck evaluation and intraoral exam. How many of us have graduated, obtained our license, and plunged into the real world ready to make our mark on the dental health of our patients, only to find that we are constrained by our schedules? The novice hygienist often makes the choice to forego certain elements of the patient assessment in order to manage scheduled patients in a timely fashion. Once this procedure is eliminated from the hygienist’s routine, it is likely lost forever. Some hygienists, both new and seasoned, think they can look at the oral tissues thoroughly while performing debridement and other routine procedures. This is a poor choice and may result in a less than adequate oral cancer screening. Some may decide that only those patients with a history of tobacco and/or alcohol use need to be carefully examined, or they may decide that children do not need to be examined because they are too young to have conditions like oral cancer.
This reasoning may be very costly for patients.14 Results of recent studies indicate that oral cancer has sharply increased in young adults who have no risk factors. Studies by Schantz in 2002 report an alarming rate of squamous cell carcinoma in the tongues of adults under the age of 40 in the United States.15 In addition, the mortality rates for the past two decades in Europe have increased six fold in people ages 20 to 39.16 The cancers being discovered in younger people are reported to be more aggressive and associated with a poorer prognosis than those seen in older populations.
Whatever your reasons for deleting or shortening a good oral screening exam, they are not good enough to neglect performing this vital service. The following is a review of the key elements and techniques for performing a thorough head and neck and intraoral exam.
The clinician should develop a systematic approach to the head and neck and intraoral assessments. The exams should be done in the same order and manner each time, making sure that no areas are missed. Each area should first be visually examined, followed by thorough palpation, if possible. The prime areas for the development of oral cancer in the wet oral tissues are:
- Tongue
- Floor of the mouth
- Salivary glands
- Gingiva.
The lip is excluded in the data since it is not considered a “wet” oral tissue. However, the lip is also considered to be a high-risk area due to its exposure to ultra-violet light sources.
A visual assessment of the patient’s general physical characteristics and head and neck area should be started during seating and obtaining of the medical/dental history and vital signs. Refer to Table 2.
The initial assessment and health history will give the clinician a chance to assess the patient’s mental and cognitive abilities and clarify points on the history. The head and neck and intraoral exam can be performed after the clinician has analyzed the information from the medical/dental histories and general physical assessment and decided there are no contraindications to continuing with the assessment. For example, the presence of a productive cough and night sweats would alert the hygienist to a potential active tuberculosis infection, and the assessment process would be stopped and the patient would be referred to his or her physician or health department.
It is important to tell the patient you are performing an oral exam and why. Individuals are often not aware that this service is being provided. Dental hygienists are in the perfect position to correlate risk factors with oral conditions and provide important education throughout the exam.
Head and Neck Evaluation
The head and neck evaluation is comprised of a visual inspection of the skin and structures of the head and neck, and palpation of the lymph nodes, salivary glands, thyroid gland and temporomandibular joint. The clinician is looking for asymmetry in structure or function, obvious superficial lesions, abnormalities in color or texture, and changes in tissue consistency when palpating the areas. Using a bidigital technique for most structures in the head and neck exam, in addition to evaluating each side of the head and neck, affords the clinician the added advantage of noticing asymmetry of the structures during function.
The clinician should observe all areas of exposed skin, paying particular attention to areas that patients can’t examine themselves, such as behind the ears and the back of the head and neck. Always have patients remove eyeglasses. The clinician should view the area under the frames for nevi (moles) and skin lesions including growths, ulcers, infections, rough patches, and discoloration. The area under the frame is a prime area for basal cell carcinoma, and this is especially true for patients who wear metal frames. The area extending into the hairline should also be evaluated. The lips should have a normal and well-defined vermilion border. An indistinct border, blotchy coloration, dimpling, indurations or tissue with a stretched appearance indicate sun damage and should be documented. The patient should be informed of these changes and possible preventive measures such as sunscreen. More advanced cases presenting with induration, dimpling and/or ulceration should be referred to an oral surgeon or dermatologist for biopsy.
Again, the lip is a prime area for sun damage and skin cancer. If an abnormal area is found on an external surface of the face, head or neck, the clinician may need to palpate the area for the information needed to document the finding. When the visual inspection and palpation of the skin is complete, the assessment process continues with the examination and palpation of the lymph nodes.
The occipital, auricular, buccal, submandibular, submental, and supraclavicular lymph nodes and the anterior and posterior lymph nodes of the cervical chain should be palpated. Normal lymph nodes should not be detectable during palpation. Abnormal findings indicative of lymphadenopathy (disease of the lymph nodes) include enlarged, hardened (indurated), and painful nodes and nodes fixed to the underlying tissues (not freely moveable). Submandibular nodes are often enlarged and indurated due to numerous previous infections; however, the nodes should not be painful or tender and should be freely moveable. Figure 1 depicts examination of the submandibular lymph nodes.
A current infectious process will usually affect several nodes in the area. These will be tender or painful upon palpation and freely moveable. While in the area of the mandible, the clinician should ask the patient to tilt the head up, put his or her teeth together and press the tongue firmly against the roof of the mouth. This contracts the mylohyoid muscle and allows the clinician to easily palpate salivary glands or lymph nodes that may be indurated or abnormal. Nodes that are fixed to the underlying tissues are very suspicious for cancer and the patient should be referred to a physician for a complete evaluation. The salivary glands can be examined while palpating the lymph nodes in the vicinity.
The salivary glands are usually not detected by palpation and exhibit no tenderness. Abnormal salivary glands might be painful, swollen, and indurated. The parotid gland (Figure 2 depicts an exam of the parotid gland) can be examined while palpating the preauricular/post auricular areas and buccal region. The anterior cervical lymph nodes and supraclavicular areas are in the chain of nodes extending on each side of the neck. Having the patient turn his or her head as each side of the neck is examined allows for a better visual field. The submandibular salivary glands may be palpated while examining the submandibular lymph nodes. Palpation of the sublingual salivary gland and a careful assessment of each duct and the total salivary flow should be accomplished during the intraoral exam. The thyroid gland is examined next.
The thyroid gland lies to both sides of and below the thyroid cartilage. Normally the thyroid gland is not detected by palpation. An abnormal gland could be indurated, enlarged on one or both sides, or contain palpable nodules. Figure 3 shows palpation of the thyroid gland. Asymmetrical movement of the thyroid cartilage during swallowing might indicate that the gland is fixed to the underlying tissues. Suspicious thyroid gland findings should be referred to the patient’s physician for evaluation. This is an area of concern for thyroid diseases and cancer.
The temporomandibular joint should be evaluated so that the motion of the jaw can be seen clearly. The clinician’s finger pads should be placed over the joint just anterior to the ear, and the patient should be instructed to open and close the mouth and move the jaw laterally to the left and to the right. Finally, the patient should be instructed to slide the jaw forward and back. The clinician should document abnormal sounds or feelings noted during function, and the patient should indicate if he or she experienced any pain or tenderness during the exam. Additionally, while performing the exam, the clinician should watch the patient’s eyes for any sign of discomfort while palpating the structures. Upon completion of the head and neck evaluation and documentation of abnormal findings, the hygienist should change patient care gloves and begin the intraoral exam.
Intraoral Examination
The intraoral examination is a continuation of the head and neck evaluation and may overlap in several areas, especially near the lips and buccal mucosa. Clinicians tend to begin the exam either in the area of the oropharynx or at the entrance to the oral cavity. The sequence learned in dental hygiene school usually follows individuals throughout their careers. It is important to establish a sequence to perform in the same manner on each oral exam. Each area should be visually inspected then palpated against the bones of the jaw or between the clinician’s fingers. Keep in mind to always try to press against a structure that is firm.
•Check the entire area of the oropharynx. Press the tongue down toward the floor of the mouth and have the patient say “ah” (Figure 4). Tell the patient not to stick the tongue out as this makes it more difficult to visualize the oropharyngeal area. The clinician should be able to evaluate the tonsil region for presence, color, size or any noted abnormalities. Dental and medical professionals often overlook this area. Often “quick” assessments are not adequate to determine subtle abnormalities. This area is normally not palpated, however, if there is any indication of an abnormality, further evaluation should be accomplished either in the dental or medical office.
•The soft and hard palates and maxillary tuberosity should be visually inspected with direct and indirect vision and the tissues palpated. The clinician should assess the areas for any color variation (other than the variation normally observed between the soft and hard palate), nodules, exudate or indurated areas. This area contains major blood vessels and nerves, so it is important to palpate it well.
•Stretch out the buccal mucosa and roll the labial mucosa over the fingers or thumbs to visualize all areas and palpate the tissues between the thumb and fingers. This area of the mouth is a prime area for lesions associated with spit tobacco use (leukoplakia, Figure 5) and trauma (mucoceles).
•Visually inspect and palpate the mandible and the floor of the mouth. Make sure you can see the tissues close to the lingual surface of the mandible. Since the floor of the mouth is a major oral cancer site, the area should be viewed very critically. Figure 6 shows healthy tissues in the floor of the mouth. Stretch the tissues away from the inferior border of the mandible with a mirror if necessary. Palpate the floor of the mouth using one finger to press down intraorally against fingers of the other hand positioned under the chin (Figure 7). The clinician is palpating for any firm tissue, masses or feelings of tenderness.
•Examine the tongue by grasping the tip with a wet gauze square and gently rolling the tongue to visualize both lateral borders, palpate the tongue and visualize the dorsal and ventral surfaces. Figure 8 demonstrates grasping the tongue and examination of the lateral border. Make sure to observe the tip of the tongue before or after grasping it with the gauze. A tongue blade or mirror may be used to deflect the buccal mucosa or elevate the tissue in addition to using the gauze. The tongue is a high-risk area for oral cancer, and is often associated with candida infections which may indicate an underlying systemic disease process.
•Observe and palpate the attached gingiva on both arches. Assess the tissues of the free gingival margin for normal color and gingival contour.
•Assess the quality and amount of saliva. Note the consistency of the saliva: is it mucous, serous, ropy or foam-like? The amount and consistency of the saliva is a good indicator of xerostomia. Many salivary gland diseases or systemic diseases may be undiagnosed. The parotid gland flow may be assessed by pressing below the tail of the parotid gland and pressing forward to milk the gland. The sublingual and the submandibular flow may be checked by drying the duct and gently pressing toward the duct in both areas.
•Question the patient about para-functional habits such as bruxing or clenching, and obtain an occlusal classification. Linea alba and morsicatio buccarum could indicate bruxing and underlying stress or anxiety.
Documenting Abnormal Findings
Written documentation of any abnormal areas discovered during exams must be detailed enough to ensure that someone who has not seen the abnormality can examine it later and determine if it is resolving, staying the same or becoming worse. Many professionals take digital photographs of abnormal areas to supplement their written descriptions. This is an excellent practice, but it should be noted that the written physical description is still a very important component of the patient’s record. The following information should be included in the written description:
•History. The patient should be shown the area in question and asked if they are aware of its presence. If so, the clinician should ask follow-up questions related to duration, change in sensations, change in appearance or size, and possible etiologic events associated with the lesion such as trauma or infection, and record the answers.
•Location. Describe the exact location of the abnormality using anatomic landmarks, fixed reference points, and metric measurements obtained by using a probe. Describing a lesion as “3cm anterior to the tragus of the right ear” is much more defined than “on the right cheek.” Another clinician will be more likely to state with certainty that a lesion described in the former fashion is resolving or gone.
•Size and shape. Use a probe to measure the length and width or diameter of lesions. If the area is elevated the height should also be recorded. Shape should include information on the margins or borders of the area, direction of growth and mode of attachment to the underlying tissues. Examples of terms used to describe the shape of lesions include round, oval, triangular and linear. The margins or borders of the lesion can be described as regular or irregular, smooth or raised. Skin cancer, specifically melanoma, often manifests as lesions that are larger than 6mm in diameter and have irregular borders or margins. Irregular margins are significant and may indicate a more serious condition. Lesions can also be described as to the direction of their growth, exophytic (outward growing), or endophytic (inward growing), and their mode of attachment to the underlying tissues, sessile (attached by a base that is as broad as the overlying lesion) or pedunculated (attached to the underlying tissues by a thin stalk).
•Color. Describe the color of the area accurately. Note variations in color and recent changes in color as reported by the patient. White-colored lesions are normally caused by an increase in keratin or in the thickness of the mucosa. Leukoplakia associated with spit tobacco (Figure 5) is an example of both an increase in keratin and an increase in the thickness of the mucosa. Red indicates a thinning of the mucosa or an inflammation of the tissues. Erythroplakia is an example of thinning of the mucosal tissues, and is found to be dysplastic (pre-malignant) in over 90 percent of cases. Yellow may indicate the presence of purulent exudates, indicating an underlying infectious process. Blue lesions may be associated with blood vessels, for example, labial or lingual varices. Brown, black or blue pigmentations may be caused by either exogenous (external) or endogenous (internal) sources. Normal physiologic pigmentation is an example of an endogenous brown to black pigmentation. Amalgam tattoos are examples of an exogenous pigmentation, as are intentional tattoos. A nevus may be brown, black, blue, red or any combination. Variations in color and changes from brown to black or blue are significant findings that may indicate a malignant process. The etiology of any darkly pigmented lesion discovered in the head and neck and intraoral area should be determined because early melanoma and early oral melanoma may mimic many benign oral conditions such as an amalgam tattoo (Figure 9).
•Consistency. Consistency refers to how something feels when pressed or palpated between, for example, two fingers. Terms used to describe consistency include firm, indurated, soft, fluctuant, resilient, and rubbery. Malignant lesions tend to be indurated, hard and/or firm, such as the lymphadenopathy associated with metastatic cancers. Fluctuant lesions are often associated with lymph or blood vessel neoplasms such as the lymphangioma.
•Surface texture. Surface texture refers to how the surface or lesion feels when the pad of the fingertip is lightly rubbed across it. A smooth surface texture is normally associated with submucosal lesions that have a normal mucous membrane covering. Rough surface textures can be further described as papillary (consisting of finger-like projections), corrugated (washboard-like), fissured (deep cracks) or crusted (covered by a scab or exudate). Figure 10 demonstrates fissures in a fissured tongue.
•Mobility. Lesion mobility should be determined while palpating the area. Lesions that are fixed to the underlying tissues are indicative of malignancy, while those that are moveable are less likely to be malignant.
•Type. Lesions may also be described by type. The major categories are flat, elevated and depressed. Refer to Table 3 for terms that can be used to further describe each of these major categories.
When describing lesions it may not be necessary to include every element that has been discussed here. However, the need for detailed, accurate information about each suspected abnormality cannot be overemphasized. A complete description might read as follows: “Round, 1 cm diameter exophytic (2mm), sessile, white, nodule located on the right lateral border of the tongue adjacent to No. 30, fixed, indurated, corrugated, the patient was not aware of its presence, and there is no pain or altered sensation in the area.”
Now that the lesion has been identified and described, the need for biopsy must be determined. It is the authors’ opinion that clinicians do not refer individuals for biopsy or definitive diagnoses as often as they should. When should we refer for a definitive diagnosis?
Protocol for Referral
When significant lesions are found in the mouth, the need for referral is evident. There is usually no doubt in a clinician’s mind that the etiology of the lesion needs to be determined. The problem arises when the lesions appear subtle and their appearance is not viewed as threatening. Some areas in the mouth may have been biopsied previously with a definitive diagnosis, but now exhibit a change in the tissue. The clinician may believe that the lesion is, for example, lichen planus that has changed since the last visit and exhibits more inflammation. A dilemma now exists as to whether the patient should be referred for an evaluation, biopsied during the current appointment or just followed. Also, the patient’s risk factors or lack of risk factors should be considered. Patients who have a history of tobacco and alcohol use might be sent for a definitive diagnosis, while someone who does not have these risk factors might be watched carefully over a short period of time to see if the lesion resolves. The clinician should try to rule out any etiology for the lesion in question. There are currently several different screening aids available to help in this decision making process.
New techniques such as the brush biopsy, Toluidine blue, ViziLite, ViziLite Plus System, VelScope or combinations of these tests can be used to help clinicians make this decision. Lynch (2007) states that some offices use these non-invasive devices as routine screening aids, in conjunction with the visual exam, radiographs and palpation.16 Auto fluorescence and chemiluminescence screening is suggested, and depending on the findings, the patient may be biopsied, examined more frequently or treated. Lynch also suggests that if there is no clinically suspicious lesion, the patient may be screened annually or semi-annually, depending on the risk factors of the patient. At the Baylor College of Dentistry Stomatology Center, some patients are seen frequently for evaluation of lesions, as often as every two to three months. In following patients, the chance that they may not return for an evaluation is always a possibility. The devices described above offer patients additional information that supports the clinician’s decision to closely follow them or refer for a biopsy.
Oral exams including cancer screenings need to be part of every dental appointment. Statistics suggest that the public may not be fully aware of the need for this service. In addition, they often do not know they have received this service, even when it has been done during a dental appointment. Dental professionals must not only make sure they are performing complete head, neck and oral exams, but they must also inform their patients about what they are doing and why. Every state’s dental practice act includes mandates for appropriate head and neck and oral examinations. The public expects dental professionals to practice ethically and with high standards of care. It is unethical to omit or partially perform these exams. Death and disfigurement caused by oral cancer will decrease if we detect cancers in their earliest stages. We must also emphasize the importance of decreasing risk factors.
Counseling patients about known risk factors such as alcohol, tobacco and nutrition is vitally important in decreasing the rate of oral cancer. As health-care providers, we should emphasize that the oral cavity cannot be separated from the whole body, and our assessments play an integral role in the total health of our patients. Studies suggest that human papilloma virus (HPV) 16, 18, 33 and 35 play a role in head and neck cancers.17 Oral/genital sex has been implicated as a possible mode of transmission in the HPV/oral cancer connection.
Why not make the health-care providers and patients in your community aware that your office performs an oral cancer screening on each and every patient?
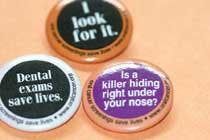
The Oral Cancer Foundation (http://www.oralcancerfoundation.org/) provides educational information that can be distributed to patients explaining the exam. Buttons can be ordered from http://www.oralcancerfoundation.org/products/dentist_products.htm for patients that show that he/she received an oral cancer screening, and for office members to reinforce that the office looks for oral cancer (Figure 11). The hygienist can be instrumental in the early detection of oral cancer and the ultimate health of all of patients. Hygienists are in a unique position because we are probably the only health-care providers who have a captive audience for our hour appointments. It is amazing what we can tell a patient during a 60-minute, uninterrupted time period. Start talking to your patients; they will listen! We need to make oral cancer screening a standard part of every office visit.
References
1. American Cancer Society. Cancer Facts & Figures 2007. Atlanta: American Cancer Society: 2007.
2. Healthy People 2010 Progress Review: Oral Health. (March 17, 2004) U.S. Department of Health and Human Services, Public Health Service, Available at: http://www.healthypeople.gov/data/2010prog/focus21/OralHealthPR.pdf.
3. Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. National Center for Health Statistics. Vital Health Stat 11(248). 2007.
4. Truman BI, Gooch BF, Sulemana I, et al. The Task Force on Community Preventive Services. (2002) American Journal of Preventive Medicine, 23(1S): 21-54.
5. Tomar SL, Logan HL. (2005) Florida Adults’ Oral Cancer Knowledge and Examination Experiences. Journal of Public Health Dentistry, 65(4); 221-230.
6. Forrest JL, Horowitz AM, Shmuely Y. Dental hygienists’ knowledge, opinions, and practices related to oral and pharyngeal cancer risk assessment. Journal of Dental Hygiene Fall 2001; 75 (IV): 271-281.
7. Horowitz AM, Siriphant P, Canto MT, et al. Maryland dental hygienists’ views of oral cancer prevention and early detection. Journal of Dental Hygiene Summer 2002; 76 (III): 186-191.
8. Dental school survey shows dental hygienist’s role in catching cancer. Cancer Weekly May 11, 2004. Available at: http://www.NewsRx.com. Accessed: Summer 2004.
9. Yellowitz, JA, Goodman HS. Physicians’ and dentists’ oral cancer knowledge, opinions and practice. J Am Dent Assoc 1995;126:53-60.
10. Maguire BT, Roberts EE. Dentists’ examination of the oral mucosa to detect oral cancer. J Public Health Dent 1994;53:115 (abstract).
11. Cannick GF, Horowitz AM, Drury TF, et al. (2005) Assessing Oral Cancer Knowledge Among Dental Students in South Carolina. JADA, 135; 373-378.
12. LeHew CW, Kaste LM (2007). Oral Cancer Prevention and Early Detection Knowledge and Practices of Illinois Dentists - A Brief Communication. Journal of Public Health Dentistry 67(2); 89-93.
13. U.S. Department of Health and Human Services. Healthy People 2010. Second ed. With Understanding and Improving Health and Objectives for Improving Health. 2 vols. Washington, DC: U.S. Government Printing Office, November 2000. Available at: http://www.healthypeople.gov/Document/tableofcontents.htm#Volume2
14. Llewellyn CD, Johnson NW, Warnakulasuriya S. (2004). Factors associated with delay in presentation among younger patients with oral cancer. Oral Surg Oral Med Oral Pathol 2004:97:6, 707-713.
15. Schantz SP, Yu GP. (2002). Head and neck cancer incidence trends in young Americans, 1973-1997, with a special analysis for tongue cancer. Arch Otolaryngol Head and Neck Surg. 2002;128(3):268-274.
16. Lynch DP, Oral Cancer Risk and Detection: The Importance of Screening Technology. RDH Sept 2007, 101-112.
17. Massano J. Regateiro FS, Januario G, et al. Oral squamous cell carcinoma: review of prognostic and predictive factors. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:67-76.
About the Author
Leslie DeLong, RDH, MHA, is freshman clinic coordinator in the dental hygiene program at Lamar Institute of Technology in Beaumont Texas. Leslie can be contacted at [email protected]. Nancy Burkhart, RDH, EdD, is an adjunct associate professor in the Department of Periodontics at Baylor College of Dentistry and Texas A&M Health Science Center in Dallas. Nancy is also a co-host of the International Oral Lichen Planus Support Group through Baylor (www.bcd.tamhsc.edu/lichen). Leslie and Nancy are co-authors of “General and Oral Pathology for the Dental Hygienist,” published by Lippincott Williams & Wilkins in Baltimore, which was released in October 2007.
Table 1
Objectives of the Head and Neck and Intraoral Examination
- Oral cancer screening
- Determine if the patient is well enough to continue dental treatment
- Determine the need for medical or other consultations
- Enable early diagnosis of pathology
- Determine possible treatment modifications
- Prepare and record baseline patient assessment information
- Determine if additional diagnostic procedures are necessary
Taken from DeLong, L. and Burkhart, N. General and Oral Pathology for the Dental Hygienist, Wolters Kluwer/Lippincott Williams & Wilkins; Baltimore: 2007
Table 2
Physical Characteristics
- Gait
- Posture
- Disabilities
- Injuries
- Weight and height
- Speech
- Exposed skin surfaces
Table 3
- Flat
- Macule (area less than 1cm differentiated from the surrounding normal tissues by color only)
- Patch (area greater than 1cm differentiated from the surrounding normal tissues by color and/or surface texture)
- Elevated
- Solid
- Plaque (broad, flat-topped lesion with a pasted-on look)
- Papule (small growth less than 5mm in diameter)
- Nodule (small growth greater than 5mm in diameter)
- Tumor
- Fluid-filled
- Vesicle (5mm or less filled with clear fluid)
- Bulla (larger than 5mm filled with clear fluid)
- Pustule (pus-filled lesion)
- Depressed
- Erosions (loss of epithelial tissue that does not extend into the dermis)
- Ulcers (tissue loss extends through the epithelium into the dermis)